Ultrasound examination (ultrasound) is used to diagnose many tissues, organs and systems of the body.
How it works: the principle of image formation is that ultrasound is reflected differently from tissues of different densities and after the computer processes the received signal, the doctor receives informative images of organs measuring tissue density, volume, size, and blood flow speed in the organ. Ultrasound is usually completely painless. We conduct ultrasound examinations using modern equipment.
We perform ultrasound of various organs. Read more about the research below.
- Ultrasound of nerves - used for diseases and injuries of nerves, to identify the location of damage.
- Ultrasound of muscles – for various muscle pains, muscle inflammations, parasitic lesions, injuries and hemorrhages in the muscles.
- Ultrasound of the salivary glands is a research method for diagnosing inflammation of the salivary glands, lesions of the facial and trigeminal nerves associated with their compression by enlarged salivary glands.
- Ultrasound of the thyroid gland is used to diagnose various diseases of the thyroid gland, oncology and autoimmune processes suspected as a result of changes in tumor markers and the appearance of antibodies to the thyroid gland identified in blood tests.
- Ultrasound of the mammary glands is carried out as a preventive examination during a clinical examination, which makes it possible to detect pathology in the early stages of mammary gland disease. This research method is used for various pains in the mammary glands, with their enlargement, decrease, deformation, discharge from the mammary glands
- Ultrasound of the mammary glands in men and boys
- Ultrasound of lymph nodes - used to determine the causes of enlarged lymph nodes, in the diagnosis of infections and malignant tumors, and diseases of the immune system.
- Ultrasound of the kidneys, bladder and prostate gland - performed for diseases of the genitourinary system, identified by changes in urine tests, as well as in the presence of pain in the lumbar regions or pelvic area.
- Ultrasound of the male genital organs is performed during a preventive examination, the presence of chronic prostatitis, abnormalities in tests, erectile dysfunction, and pain during sexual intercourse.
- Ultrasound of the female genital organs - performed during a preventive gynecological examination, in case of changes in gynecological smears, deviations from the norm in the results of tests for female sex hormones. Diagnosis of tubal patency and tubal infertility. Salpingography / Sonosalpingography / Hysterosalpingography / SGSG - for diagnosing patency of the fallopian tubes and identifying the causes of infertility.
- Ultrasound of joints - the main advantage of ultrasound of joints over X-ray examination is that ultrasound can see not only the cartilage of the joint itself, joint fluid and tissues lying nearby (ligaments, tendons, muscles), but also avoids radiation exposure to the patient’s body. Ultrasound examination is used for various pains and deformities in the joints, rheumatic diseases and previous injuries, to determine the safety of cartilaginous surfaces.
- Ultrasound of the abdominal organs;
- Ultrasound of the pancreas, liver and gall bladder, spleen - is used to determine the causes of digestive problems, flatulence, diarrhea and constipation.
- Ultrasound of entheses in the diagnosis of fibromyalgia. Ultrasound examination for fibromyalgia, enthesopathy, tendinitis, muscle pain - examination of entheses i.e. places where muscles attach to bones, which are often the cause of pain.
Ultrasound of peripheral nerves
We have the experience and state-of-the-art diagnostic equipment to determine the cause of nerve damage. In particular, we perform ultrasound examination of nerves and electroneuromyography (ENMG). Ultrasound examination of nerves allows you to more accurately determine the location of damage or compression of the nerve. Ultrasound of peripheral nerves does not require special preparation.
For correct and accurate treatment of any nerve disease, it is important to accurately determine the location and cause of its damage.
We perform ultrasound examination of the nerves:
- Ultrasound of the ulnar nerve,
- Ultrasound of the radial nerve,
- Ultrasound of the median nerve/carpal tunnel/Guyon's canal,
- Ultrasound of the common peroneal nerve,
- Ultrasound of the tibial nerve at the level of the popliteal fossa,
- Ultrasound of the tibial nerve in the lower 1/3 of the leg,
- Ultrasound of the sciatic nerve.
If necessary, we will offer you the necessary treatment .
Causes and symptoms of peripheral nerve damage
The main cause of nerve damage is most often its compression, which occurs for one of the following reasons:
- inflammation of surrounding tissues. When inflammation occurs, swelling occurs, the tissue enlarges and puts pressure on the nerve.
- injury. The integrity of the nerve is compromised either due to compression by surrounding tissues (bone fragments), or due to excessive impact on the nerve under which it “breaks”.
- occupational injury. The nerve can be damaged during prolonged work at the computer with the hand in an awkward position.

The location where symptoms of nerve damage appear depends on which nerve is damaged. However, there are general symptoms of damage to almost any nerve:
- pain;
- limb weakness;
- change in sensitivity. For example, the appearance of tingling, burning, numbness, etc.;
The location of nerve damage or compression can be seen on ultrasound. Taking into account the ultrasound data of the nerves, the correct treatment regimen is constructed.
How is ultrasound of nerves performed?
To study peripheral nerve trunks, multifrequency linear sensors 8-14 MHz, or convex sensors 3.5-5 MHz are used.
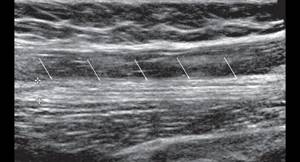
The ultrasound procedure of peripheral nerve trunks begins with finding the point at which the nerve trunk is best visualized. The assessment is carried out in a cross section all the way up and down from this point. It is very important that the specialist has a good understanding of the topographic anatomy of the peripheral nervous system.
When scanning nerve trunks, it is necessary to evaluate their structure, contours, as well as surrounding tissues. If the integrity is violated, the specialist pays attention to the depth of the lesion, the extent of the lesion, and the possible impact of surrounding tissue on it.
If a space-occupying lesion of the nerve trunk is detected, the size, structure, contours of the formation and the presence or absence of blood flow are assessed.
The procedure time is about 20 minutes.
Preparing for the study
The method is characterized by the absence of a preparatory stage. At any time convenient for him, the patient can undergo an ultrasound scan of the nerves and immediately after the procedure receive diagnostic results, on the basis of which treatment is prescribed.
Ultrasound of muscles, muscles, tendons, ligaments
We perform examination of almost all muscles accessible to ultrasound, muscle attachment points (entheses), tendons, ligaments, and joints. Using ultrasound, you can see changes in muscle, ligament and tendon tissue. Soft tissues weakly block x-rays, so ultrasound provides much more information than x-rays. Ultrasound reveals inflammatory processes (myositis, tendinitis, bursitis, ligamentitis), disorders of the anatomical structure of muscles, parasitic muscle lesions (trichinosis, etc.), hemorrhages, ruptures, tumors and other pathological processes. If necessary, we will offer you the help of an appropriate specialist: a surgeon, neurologist, rheumatologist and other diagnostic tests of muscles.
What muscles can be examined using ultrasound: muscles of the buttock, thigh, lower leg, back, arms, muscles of the trunk, abdomen, neck, face, masticatory muscles. Preparation for ultrasound of muscles, tendons, ligaments. No special preparation is required. We recommend that you take with you to the study the results of previously performed studies, analyzes and consultations. This may be useful for correctly constructing an examination technique, targeted search for a particular pathology, and detailed interpretation of ultrasound results.
The main indications for ultrasound examination of muscles:
- Muscle pain of unknown origin
- Muscle swelling, muscle mass
- Hereditary muscle diseases - myopathies
- Inflammatory diseases of muscle tissue: myositis, polymyositis (in this case, the examination standard also includes electromyography)
- Muscle injuries, when there is a question about rupture of muscle fibers and hemorrhage into muscle tissue, removal or puncture of the hematoma
- Parasitic muscle damage - trichinosis, etc.
- Muscle tissue infarction
The main indications for ultrasound examination of ligaments and tendons:
- Pain at muscle attachment points
- Swelling at muscle attachment points
- Inflammatory diseases of tendons and ligaments: bursitis, tendonitis, tendovaginitis, ligamentitis, periarthritis, etc.
- Tendon and ligament injuries when a tendon or ligament rupture (severance) is suspected
- Fibromyalgia
The combination of ultrasound with the needle myography method allows us to more successfully clarify the cause of the pathological process in muscle tissue.
Ultrasound of the soft tissues of the buttocks
Diseases leading to pain in the buttocks can be caused by:
- injuries to the gluteal muscle;
- development of arthrosis or arthritis of the hip joint,
- inflammation of the soft tissues, muscles, ligaments and tendons surrounding the hip joint;
- inflammation of the subcutaneous fat of the buttocks;
- inflammatory skin diseases (boils, atheromas);
- inflammation of the sciatic nerve and piriformis syndrome.
If the following symptoms appear, it is recommended to do an ultrasound of the piriformis muscle:
- Pain in the gluteal region, aggravated by walking, sharp or aching;
- Discomfort or pain that occurs while standing;
- Inability to cross your legs while sitting;
- Unpleasant sensations during squats.
The procedure is carried out in accordance with standard methods, therefore it allows us to identify any pathological processes at an early stage of their development.
Sign up for an ultrasound of the piriformis muscle
Ultrasound of the salivary glands: parotid and submandibular
The parotid and submandibular salivary glands are clearly visible on ultrasound. The structure of the salivary glands, their size, the presence of salivary duct stones, the inflammatory process, and tumor formations are visible. We perform ultrasound of the salivary glands using modern ultrasound equipment.
If necessary, we will offer you saliva tests for viral and bacterial infections of the salivary glands, autoantibody testing for Sjögren's disease and syndrome, and assistance from a rheumatologist or immunologist for inflammatory processes of the parotid and submandibular salivary glands. Our clinic also specializes in the field of facial neurology (facial pain, trigeminal neuralgia, facial paresis, neurological complications in dentistry). Ultrasound of the salivary glands, in most cases, is performed simultaneously on both the right and left sides, for comparison and more accurate interpretation of ultrasound data.
Preparation for ultrasound of the parotid and submandibular salivary glands. Ultrasound examination of the salivary glands does not require special preparation. We recommend that you take with you to the clinic the results of previously performed tests, MRI results, if one was performed, and medical reports. These data may be useful for more accurately interpreting ultrasound results and for comparing the current state of the salivary glands with data from previous studies.
The main indications for ultrasound examination of the parotid and submandibular salivary glands:
- Facial nerve paresis and trigeminal neuralgia associated with enlarged salivary glands and their pressure on the nerves, atypical facial pain
- Pain and enlargement of the salivary glands
- Dry mouth due to insufficient saliva production
- The presence of stones in the ducts of the salivary glands
- Inflammatory diseases and rheumatic lesions of the salivary glands - sialadenitis, mumps (inflammation of the parotid salivary gland), Sjögren's syndrome (autoimmune disease of the salivary glands)
- Oncological diseases of the salivary glands
- Sarcoidosis
Diseases detected by ultrasound
Ultrasound of peripheral nerve trunks allows you to diagnose the following pathological conditions:
- traumatic nerve injuries (they are characterized by a violation of the integrity of the nerve trunk, a change in echogenicity);
- tunnel syndromes (they consist of compression of the nerve roots in the bone and ligamentous canals - the nerve is flattened directly in the area of compression, which is reflected in the appearance of its cross-section, an increase in the diameter of the nerve is visualized above the compression site);
- space-occupying formations in the area of nerves (they have a different echogenic structure).

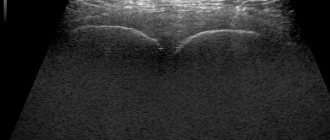
1 Longitudinal scan of the radial nerve in the upper third of the shoulder

2 Transverse scan of the radial nerve in the middle third of the shoulder

3 Radial nerve in the spiral canal, (arrow 1 nerve, arrow 2 artery)
Ultrasound of the thyroid gland. Ultrasound of the parathyroid glands
Ultrasound of the thyroid gland is performed to identify diseases of various natures, monitor their course and the effectiveness of treatment. Ultrasound of the thyroid gland reveals inflammatory processes (thyroiditis), cysts, nodules, tumors, an increase in the size of the thyroid gland, which is often accompanied by a feeling of a lump in the throat, and even difficulty swallowing and breathing. The activity of autoimmune thyroiditis during ultrasound can be assessed by the characteristics of blood circulation in the thyroid gland: with active autoimmune thyroiditis, blood flow in the gland is increased. Learn more about thyroid screening, including tests
Ultrasound of the parathyroid glands. The parathyroid glands are very small in size and differ little in density from the surrounding tissue, so they are not always visible on ultrasound scans. Ultrasound is mainly used to diagnose parathyroid tumors when parathyroid hormone (PTH) levels are elevated. Read more about the treatment of diseases of the parathyroid glands .
Preparation for ultrasound of the thyroid gland and parathyroid glands. Ultrasound examination of the thyroid and parathyroid glands usually does not require special preparation. We recommend that you take with you to the clinic the results of previously performed tests, the results of scintigraphy, if one was performed, and medical reports. These data may be useful for more accurate interpretation of ultrasound results.

Ultrasound of the thyroid gland
The main indications for ultrasound examination of the thyroid gland:
- Thyroiditis – inflammation of the thyroid gland
- Deviation from the norm in tests for the levels of hormones T3, T4, TSH in the blood
- Lumps (nodules) in the thyroid gland
- Thyroid enlargement
- Difficulty swallowing, feeling of a lump in the throat
The main indications for ultrasound examination of the parathyroid glands:
- Increased or decreased production of parathyroid hormones
- Disturbance of calcium-phosphorus metabolism
- Suspicion of a parathyroid tumor
Ultrasound examination of the peripheral nervous system
19/07/16
The incidence of soft tissue damage involving peripheral nerves is 25-65%.
The incidence of tunnel neuropathies is 30-40% of all diseases of the peripheral nervous system.
More than 60% of victims become disabled.
ADVANTAGES OF ULTRASOUND
- Safety and harmlessness of the study.
- Possibility of repeated - dynamic research
- Cost-effectiveness, relative simplicity and speed of research.
- Lack of necessary preparation of the patient.
- The ability to visualize the nerve trunk with differentiation into bundles.
- Possibility of research in the presence of metal structures.
Ultrasound can evaluate:
- Brachial plexus
- Median nerve
- Ulnar nerve
- Radial nerve
- Digital nerve cysts
- Femoral nerve
- Sciatic nerve
- Tibial nerve
- Common peroneal nerve
- Digital nerves of the foot
It is possible to evaluate neuropathies associated with tunnel syndromes:
- -compression of the median nerve (carpal tunnel syndrome)
- -compression of the ulnar nerve (cubital canal and Guyon)
- -compression of the radial nerve (sm spiral canal)
- -compression of the sciatic nerve
- -compression of the tibial nerve
- -compression of the digital nerve of the foot
Basic methods for diagnosing a nerve:
Electrophysiological (ENMG) is the “gold” standard (determines the severity of impulse conduction disturbances), but:
- does not provide an image of the nerve trunk
- does not evaluate the structure of surrounding tissues
- does not indicate the nature and cause of damage
- Localization is not always accurately reflected
MRI—
- requires sophisticated equipment
- impossibility of carrying out in the presence of metal in the body.
Ultrasound is a modern method that can determine the level, type of pathological process, and the cause of its occurrence.
Ultrasound CAPABILITIES:
1. Assess damage to the nerve trunk:
- partial damage
- complete breaks
- assessment of the size of the neuroma, the length of diastasis.
2. Evaluates TRACTIONAL-COMPRESSION changes
3. Evaluates VOLUME LOCATIONS (tumor and non-tumor)
- schwannoma
- neurofibroma
- intraneural ganglia
Type of pathological process Sensitivity of ultrasound Specificity of ultrasound Accuracy of ultrasound
Compression neuropathies 98,7% 90,1% 92,6%
Traumatic injuries 97,5% 99,7% 99,4%
Nerve trunk tumors 97,8% 92,6% 89,7%
The use of ultrasound allows you to:
- -optimize the differential diagnostic search for the causes of pain
- -minimize the number of studies (avoid unnecessary manipulations)
- -reduce radiation exposure to the patient
- -increase diagnostic efficiency
Our clinic conducts research on adults and children.
Ultrasound of the mammary glands and peripheral regional lymph nodes
Ultrasound of the mammary glands is relevant, first of all, for the diagnosis of benign and malignant neoplasms of the mammary glands, inflammation (mastitis), and mastopathy. Simultaneous examination of the lymph nodes that “serve” the mammary glands increases the accuracy of diagnosing tumor diseases. Ultrasound of the mammary glands is advisable when there is a change in size (increase or decrease), deformation of the mammary gland, when discharge appears, any discomfort, and, especially, pain in the mammary glands, with enlargement of the axillary and supraclavicular lymph nodes.
Ultrasound control is also used during puncture of the mammary glands to determine the malignancy of a tumor-like neoplasm in the mammary gland.
Preparation for ultrasound of the mammary glands. Ultrasound examination of the mammary glands does not require special preparation; it is usually performed from the 5th to the 10th day of the menstrual cycle. If there is a need for an urgent examination of the mammary glands, an ultrasound scan can be performed on any other day of the menstrual cycle.
Main indications for the study:
- Preventive breast examination
- Mastopathy and suspicion of it
- Changes in size and/or deformation of the glands
- The appearance of discharge from the mammary glands
- Any kind of discomfort and pain in the mammary glands
- Enlarged axillary and/or supraclavicular lymph nodes
- Neoplasms in the mammary glands
- Performing a puncture under ultrasound guidance
Advantages of ultrasound of peripheral nerve trunks
The positive aspects of ultrasound examination of peripheral nerve trunks are as follows:
- relatively low cost compared to MRI;
- absence of ionizing effects;
- safety at any frequency of research;
- high visualization of nerve trunk structures;
- assessment of all characteristics in real time;
- the possibility of using additional techniques (for example, Doppler sonography, panoramic scanning).
Among the negative aspects of ultrasound examination of peripheral nerve trunks that complicate visualization, one can note: the deep location of the nerve trunks, screening by dense structures (bone), distal parts of the nerve trunks (terminal branches).
Ultrasound of the mammary glands in men and boys
As you know, not only women, but also men have mammary glands. In men, breast tissue and milk ducts are reduced, i.e. are in their infancy.
Sometimes, the size of the male mammary glands can change, depending on the decrease or increase in fat reserves in the body. Also, breast enlargement in men can be observed due to pathology of the endocrine system - increased levels of prolactin, insulin resistance, gynecomastia. Ultrasound of the mammary glands helps to distinguish the usual “fatty” breast enlargement in men from gynecomastia. On an ultrasound examination of the male breast, we clearly see its structure, foci of inflammation, if any, and other pathologies: dilated milk ducts, cysts, fibroadenomas, malignant neoplasms, etc.
The main indications for performing ultrasound of the mammary glands in men:
- Enlargement of the mammary glands, their swelling;
- Enlargement of the nipple, its deformation;
- Discharge from the nipples (this is normal for men and should not be)
- High values of prolactin and estrogen in blood tests
Ultrasound of the male mammary glands does not require special preparation. If necessary, we will offer you a consultation with an endocrinologist or urologist-andrologist.
In European medicine, ultrasound has long been used to study nerve pathologies. Its important advantage is ease of execution and low cost of research. Ultrasound diagnostics does not require special preparation and can be performed at any age. The examination time does not exceed 30 minutes. Ultrasound provides a complete picture of the main nerve trunks of the lower and upper extremities and the places where they are pinched (the so-called tunnels).
Modern ultrasound machines allow visualization of the nerve along its entire length.
In real time, you can see changes in the position of the nerve and everything that is adjacent to it, namely muscles, vessels, tendons, etc. An important advantage of the method is the simultaneous assessment of the intensity of blood flow in the vessel that supplies the nerve under study. The procedure takes little time and does not cause any inconvenience to the patient.
The only drawback of ultrasound is the inability to see the nerve where it passes under the bone structures. In this case, MRI must be selected for diagnosis.
Indications for ultrasound of peripheral nerves
- Focal neurological impairment occurring immediately after injury (suspected peripheral nerve injury).
- Neurological disorder identified in patients with chronic diseases.
- Ultrasound monitoring after operations on peripheral nerves of the musculoskeletal system (neurolysis, neurorhaphy, autoplasty, etc.) and in close proximity to them.
Most often, MRI and ENMG (electroneuromyography) are used to diagnose diseases of the nervous system. These methods provide a fairly accurate picture of the damage. But each of them has its own limitations. Changes in nerve function can be assessed with high accuracy using electroneuromyography. It allows you to identify disturbances in the conduction of impulses along nerve fibers. But sometimes, for a more accurate diagnosis, the doctor needs to see the nerve. This requires the use of radiation imaging methods. Traditionally, MRI is considered the method of choice for radiological diagnosis of diseases of the nervous system. However, when studying peripheral nerves, the use of MRI is limited - the cost and duration of the study do not allow studying the entire length of the nerve trunk or examining both hands. This reduces the information content of the technique and makes it difficult to make an accurate diagnosis. The main advantage of nerve ultrasound over MRI and ENMG is a more detailed picture of the nerve trunk and its damage. Moreover, the research process itself does not bring any discomfort to the patient and has no side effects. ENMG and ultrasound of the nerve are studies that complement each other!
Ultrasound of lymph nodes (lymph nodes)
Our specialists perform ultrasound of all groups of lymph nodes, including cervical, supraclavicular, axillary, intra-abdominal and inguinal lymph nodes. If necessary, we will offer you medical assistance, a lymph node biopsy, and examination for tumor, infectious and autoimmune diseases.
Preparation for ultrasound of lymph nodes.
Ultrasound examination of the cervical, supraclavicular, axillary and inguinal lymph nodes does not require special preparation.
Ultrasound of intra-abdominal lymph nodes can be difficult when gas accumulates in the intestines and after eating. Therefore, two days before an ultrasound scan of intra-abdominal lymph nodes, it is advisable to avoid eating foods that promote gas formation, and perform the examination itself on an empty stomach. We recommend that you take with you to the clinic the results of previously performed ultrasound of the lymph nodes and other studies, tests, and medical reports: these data may be useful for clarifying the scope of the study and a more detailed description of the area of interest.
Ultrasound of lymph nodes is a convenient study to find the causes of their enlargement and pain. Enlarged lymph nodes can often be the result of infections, malignant tumors, or diseases of the immune system. Lymph nodes can also be affected by parasites (for example, filaria), which clog the lymphatic ducts and can cause lymphostasis (lymphatic swelling below the affected lymph node). The bodies of large parasites are visible on ultrasound scans.
Indications for ultrasound:
- Enlarged lymph nodes of various natures
- Evaluation of the treatment in accordance with the dynamics of the condition of the lymph nodes.
- Parasitic infection of lymph nodes, chronic infection
- Prolonged increase in body temperature without an established cause
- Pain in the area of the lymph nodes
Ultrasound of lymph nodes if certain tumor and inflammatory processes in various areas of the body are suspected:
- Ultrasound of the lymph nodes of the neck (submandibular, occipital, tonsillar) - head, ear, throat, nose, neck, thyroid gland;
- Ultrasound of supraclavicular lymph nodes - neck, thyroid gland, mammary glands, lungs, esophagus, organs of the thoracic cavity and mediastinum, upper extremities;
- Ultrasound of axillary lymph nodes - neck, thyroid gland, mammary glands, lungs, esophagus, organs of the thoracic cavity and mediastinum, upper extremities;
- Ultrasound of intra-abdominal lymph nodes – abdominal organs, kidneys, bladder, genitals;
- Ultrasound of inguinal lymph nodes - abdominal organs, bladder, genitals, lower limbs.
Ultrasound examination of peripheral nerves
For all questions regarding ultrasound examination of peripheral nerves, existing contraindications and specifics of its implementation, you can contact the doctors of our center.
In recent years, there has been a growing interest in such methods of neuroimaging of peripheral nerves as MRI and ultrasound for various types of neuropathies, both acquired and hereditary origin. The main objective of using neuroimaging methods in combination with neurophysiological and laboratory testing is to facilitate the differential diagnostic search. Previously, the use of ultrasound of peripheral nerves was limited to verification of the anatomical integrity of nerve trunks in the event of traumatic injury and visualization of tumor processes. In the following, the advantages of the ultrasound method for various diseases of the peripheral nerves are shown.
The undoubted advantage of the peripheral nerve ultrasound method is its non-invasiveness, safety for the subject, and the possibility of performing it an unlimited number of times. Moreover, the method is highly informative for a wide range of peripheral nerve pathologies.
According to the results of transverse ultrasound scanning, the peripheral nerve is an oval or round formation with a clear hyperechoic contour and an internal heterogeneous ordered structure (like a “honeycomb”); with longitudinal scanning, the peripheral nerve is located in the form of a formation of a linear structure with a clear hyperechoic contour, which includes hypo-hyperechoic stripes alternate (like an “electrical cable”). The analyzed parameters during ultrasound can be divided into two large groups: qualitative and quantitative. One of the main quantitative parameters assessed is the cross-sectional area (CSA) of the nerve. This parameter is highly reproducible and normative values exist for each nerve in adults at standard levels of measurement. Measurements are taken at several points, including nerves in the arms in the proximal and distal sections (median, ulnar), spinal nerves of the brachial plexus (C5/C6/C7), nerves in the legs (sciatic nerve and its branches).
Protocols do not vary greatly between laboratories, mainly due to the inclusion of additional ulnar nerve points and a posterior tibial nerve point at the ankle level. The ultrasound protocol we developed for assessing the cross-sectional area includes 13 measurements on each side (26 measurements in total).
The qualitative characteristics of the restructuring of peripheral nerves are based on the work of L. Padua. It is based on the visually determined principle of preserved differentiation of the nerve into fascicular groups, applicable for the median and ulnar nerves at the level of the shoulder and forearm during transverse scanning.

Differentiation into fascicular groups may be absent (Type 1), preserved with enlargement of one or more hypoechoic fascicles (2B), or at the expense of all distinguishable fascicular groups (2A).
Table 1. Main types of changes in the sonographic structure of the nerve.

Changes in peripheral nerves described by many researchers not only in dysimmune, but also hereditary neuropathies. The basic principles for describing changes in nerves during neuropathies are the symmetry and prevalence of enlargement of nerve trunks. Researchers today believe that the reason for the increase in PPS is edema and the alternation of demyelination and remyelination processes during periods of exacerbation and remission of CIDP, which is confirmed by histological examination of the nerve in the detection of “onion-head” type changes.
Patients with a course of the disease of 6 months or more, according to the results of ultrasound scanning, have a diffuse increase in CSA, in contrast to newly diagnosed patients, in whom an increase in CSA was noted only in the proximal parts of the nerve trunks.
In accordance with this, several scales have been validated, the use of which in routine practice is difficult due to their cumbersomeness. The table shows some of them, as well as nosological forms that are compared with each other.
In addition, it turned out that it is of great importance at what time the study was carried out regarding the manifestation of the pathological process and its therapy. Thus, in naive patients with CIDP, the previously detected diffuse symmetrical increase in CSA of all nerves regresses during therapy. The assessment of parameters such as vascularization and echogenicity of nerves is not widely used due to the technical limitations of modern ultrasound scanners.
Today, the search for optimal PN ultrasound protocols continues for patients with suspected polyneuropathy, both dysimmune and hereditary origin.
Despite the discussed limitations, the main advantage of ultrasound as opposed to MRI is the inexpensive cost of the study, its mobility and the ability to perform an unlimited number of times with assessment of the dynamics of changes in ultrasound parameters of PN, which, as studies have shown, is important when assessing the effectiveness of therapy for patients with dysimmune neuropathies.
We can offer the full range of ultrasound examinations of peripheral nerves using established examination protocols. The research and interpretation of data is carried out at a high level by specialists who have proven their professional level with time and publications.
Author of the text: Doctor of Medical Sciences Druzhinin D.S.
Ultrasound of the kidneys and bladder in men and women
Using ultrasound, you can see abnormalities in the structure of the kidneys and bladder, inflammatory changes (cystitis, pyelonephritis, glomerulonephritis), tumor neoplasms (polyps, solid tumors, etc.), renal vessels and blood flow in them, the volume and speed of urine release from the ureters into the bladder , kidney and bladder stones.
If necessary, we will offer you the help of a urologist, therapist or other specialist, urine and blood tests for kidney function, urine tests for bacteria, viruses and fungi. In case of autoimmune kidney disease, we will offer you the help of an immunologist and blood tests for autoimmune markers (diagnosis of glomerulonephritis).
Preparation for ultrasound of the bladder and kidneys. Before the ultrasound, the bladder must be full (you need to drink about 1 liter of water 1 hour before the examination). We recommend that you take with you to the clinic the results of previously performed studies, tests, and medical reports: these data may be useful to clarify the scope of the study and more accurately interpret the ultrasound results.

Using ultrasound, you can detect various pathologies of the kidney structure, inflammatory processes, kidney stones and tumor formations
In what cases is an ultrasound of the bladder performed to determine residual urine? Residual urine is some amount of urine that remains in the bladder after urination. If there is difficulty urinating, the amount of residual urine increases. The volume of residual urine can be calculated by ultrasound and used to clarify the diagnosis and evaluate the outcome of treatment. The indication for an ultrasound examination of the bladder with determination of residual urine is a violation of urination: frequency, difficulty urinating, a decrease in the diameter of the stream, sluggishness of the stream, a feeling of incomplete emptying of the bladder, repeated copious urination after a short period of time.

This is what the kidney looks like on an ultrasound. The arrow indicates a kidney stone
The main indications for ultrasound examination of the kidneys:
- Deviation of urine tests from the norm
- Inflammatory processes of the kidneys (interstitial nephritis, pyelonephritis, glomerulonephritis, etc.)
- Kidney stones, “sand” in the kidneys
- Hypertension - in this case, the kidneys and renal arteries are examined for their role in increasing blood pressure
- Pathological discharge from the genital tract
- Pain when urinating
- Tumor neoplasms of the genitourinary system
The main indications for ultrasound examination of the bladder:
- Deviation of urine tests from the norm
- Blood in the urine, blood clots in the urine
- Pain during urination or sexual intercourse
- Urination disorders (frequency, difficulty urinating, decreased stream diameter, sluggish stream, feeling of incomplete emptying of the bladder, repeated copious urination after a short period of time)
Ultrasound of the female genital organs (pelvis)
With us, you can undergo an ultrasound examination immediately at an appointment with a gynecologist or sign up for an ultrasound examination as a separate service.
Which female genital organs are examined during a pelvic ultrasound: the uterus, ovaries, the presence of inflammatory fluid effusion or blood in the pelvis. A special technique is also used to determine the patency of the fallopian tubes using ultrasound.
Preparation for ultrasound of the female genital organs (pelvis). Ultrasound examination of the internal female genital organs usually does not require special preparation. If examination with a vaginal probe is intended (this is considered a more informative examination), it is necessary to empty the bladder immediately before the examination. During an ultrasound of the female pelvis through the anterior abdominal wall, the bladder must be full (you need to drink at least 1 liter of water 1 hour before the examination). In some cases, examination of the female genital organs is performed on certain days of the menstrual cycle, so we recommend that you check with your doctor about the purpose of the examination and take with you the results of previously performed examinations: this may be useful in describing the results of the ultrasound.
Frequent assistance in performing pelvic ultrasound in women:
- Inflammatory diseases (adnexitis, salpingoophoritis, etc.)
- Tumor-like neoplasms (cysts, uterine fibroids, polyps, etc.)
- Infertility
- Miscarriage
- Adhesive disease of the pelvis
- Painful menstruation, pain of unspecified origin
- Pain during intercourse
Often, simultaneously with the examination of the female pelvic organs, an ultrasound of the mammary glands is performed. This study is best performed between the 5th and 10th days of the menstrual cycle.
Diagnosis of pinched sciatic nerve
- Accurate diagnosis and effective treatment of pinched sciatic nerve.
- We have been helping people with diseases of the spine and joints for more than 30 years.
- Relief from pain after just 1-2 sessions using Dr. Bobyr’s original technique – defanotherapy.
Pinched sciatic nerve is a condition that can be caused by various reasons associated with pathological processes in the spinal column, muscles, and sacroiliac joint. It is important to establish the correct diagnosis, since the effectiveness of treatment depends on this.
To diagnose the causes of pinched sciatic nerve, the following studies are used:
- X-ray of the lumbar spine.
- Ultrasound examination of the spinal column.
- CT scan.
- MRI.
- Electroneuromyography.
Doctor's appointment
During the initial appointment of a patient with symptoms of sciatic nerve compression, the doctor collects an anamnesis of the disease, life, and conducts an examination.
First of all, the doctor will most likely ask you the following questions:
- How long have you had symptoms, how strong are they, how often do they bother you?
- When did they first arise, what preceded it?
- Do you experience a feeling of numbness or weakness in your legs?
- Do pain and other symptoms get worse when you are in a certain position?
- Does pain interfere with your daily activities?
- What usually helps you cope with pain? Do you take any over-the-counter pain medications?
- How do pain sensations change during the day?
It is important for the doctor to find out what profession the patient has, whether his work involves intense physical activity, heavy lifting, or, on the contrary, prolonged sitting in one place, and whether he plays sports. It is necessary to clarify whether there were any previous problems with the spine.
Medical examination
If a pinched sciatic nerve is suspected, the doctor examines the area of the lower back, sacrum, checks the tone and strength of the muscles of the lower back, lower extremities, and evaluates the sensitivity along the sciatic nerve using a special needle and brush. The doctor presses on certain points to identify pain.
The patient may be asked to do some physical exercise and asked if the pain gets worse during exercise. This helps to judge which nerve is affected:
- squat down and stand up;
- walk on tiptoes or on heels;
- alternately raise the right and left outstretched legs, lying on your back;
- lean forward, backward, to the sides (this helps to assess the mobility of the spine).
The doctor also evaluates the patient’s standing position and his gait.
To identify sciatic nerve irritation, your doctor will check for some specific symptoms:
- Neri's symptom.
It is checked with the patient in the supine position. The doctor places his hand under the back of the patient's head and bends his head, bringing his chin to his chest. A symptom is considered positive if it causes pain in the lower back. - Lasègue's symptom.
The patient lies on his back. The doctor takes the patient's straightened leg with his hands and bends it at the hip joint. The result is assessed depending on how far the leg was lifted and how much pain it caused:
- I degree:
pain occurs only when the leg is raised to 60 degrees, it is not very strong and goes away quickly. In this case, there is a slight protective tension in the muscles of the back and abdomen. - II degree:
moderate pain that occurs when raising the leg to 45 degrees. At the same time, the protective tension of the abdominal and back muscles is clearly visible. - III degree:
severe pain and sharp muscle tension occurs when the doctor raises the leg to 30 degrees.
- Modified Lasègue symptom.
The patient lies on his stomach, his legs hanging off the couch. When bending the leg at the hip joint and lowering it down, pain occurs in the lower back. - Vengerov's sign.
They check the same way as Lasegue's symptom, but the patient's attention needs to be diverted. The fact that the symptom is positive is indicated by the tension of the abdominal muscles when raising the leg. - Bekhterev's symptom
. When Lasegue's symptom is tested on the “healthy” leg, pain occurs in the “sick” leg. - Landing symptom
. The patient is asked to sit in a supine position with legs straight. He can't do it, because of the pain he has to bend his legs. - Sicard's sign
. The patient, who is lying on his back, is asked to strongly bend the foot at the ankle joint towards the sole. The symptom is positive if pain occurs along the back of the leg, along the sciatic nerve. - Gowers-Sicard sign
. Pain in the area of the sciatic nerve occurs when the foot is flexed in the opposite direction, in the dorsal direction. - Turin's symptom
. The patient experiences severe pain along the back of the leg when dorsiflexing the big toe. - Marching test
. The doctor asks the patient to march in place and at the same time feels the muscles of the lower back. You can feel their intense tension.
Instrumental research methods
In some cases, diagnosis of the causes of a pinched sciatic nerve is limited only to a doctor’s examination. Additional diagnostic methods are not always needed. After examining the patient, the doctor can prescribe conservative treatment and further monitor his condition. If the pain does not go away and intensifies, movement and sensitivity disorders appear, you need to conduct an examination.
There are some symptoms that are called "red flags". If they are detected, this indicates that the patient may have a serious pathology, and, at a minimum, an x-ray should be immediately performed. Sometimes it is worth starting immediately with a CT scan and MRI.
Key red flags:
- The pain is very strong, disturbing not only during movements and physical activity, but also at rest. Sometimes the pain intensifies at night and prevents sleep. This is how metastases of malignant tumors in the spine can manifest themselves.
- Decreased or loss of sensitivity in the genital area and anus.
- Dysfunction of the pelvic organs, loss of control over urination and defecation.
- Lower paraparesis - weakening of the leg muscles, impaired movement and decreased reflexes.
- Fever is an increase in body temperature over 38 degrees.
- Decreased immunity, which is indicated by frequent, chronic, severe infections.
- Symptoms that first appear in a person over 50 years of age: at this age, the likelihood of developing malignant tumors and serious chronic diseases increases.
- Unreasonable weight loss, despite the fact that the patient eats well, does not go on a diet, and does not exhaust himself with physical work and high stress in sports.
X-ray of the spinal column
Radiography is the simplest, fastest, inexpensive and accessible method for diagnosing many spinal diseases. It is not as informative as computed tomography or MRI, but it allows you to quickly identify or exclude gross changes in the vertebrae.
Pathologies that can be identified using radiography and which may be associated with pinched sciatic nerve:
- Fractures and displacements of the vertebrae.
- Spinal stenosis is a narrowing of the spinal canal, which can lead to pinching of the spinal cord and roots.
- The intervertebral discs themselves are practically invisible on x-rays, but indirect signs of their damage can be detected, for example, a decrease in the distance between adjacent vertebrae.
- Osteophytes are bone growths on the vertebrae.
- Spondylolisthesis is an anterior displacement of the overlying vertebra relative to the underlying one.
- Osteoporosis, a condition in which bone loss and decreased density occurs, usually occurs in older people.
- Malignant tumors, metastases in the spine.
- Congenital anomalies of the spinal column.
- Infectious processes in the vertebrae.
The x-ray usually lasts about 5 minutes. Modern digital devices make it possible to obtain clear images in which many structures are clearly visualized.
The study does not require special preparation. Women who are pregnant or trying to conceive should tell their doctor, as x-rays are contraindicated during pregnancy.
Pictures are taken in a lying or standing position, in different projections, in front, profile, at certain angles. The doctor selects projections that provide the most informative images.
Ultrasound of the spine
In some cases, patients with symptoms of a pinched sciatic nerve are shown an ultrasound examination of the spinal column. This is also a simple, affordable, but, unlike radiography, a completely safe diagnostic method, since it does not use X-ray radiation. Ultrasound can show soft tissue abnormalities that are not visible on x-rays.
Ultrasound of the spine helps to identify:
- pathological processes in tissues caused by age-related changes;
- changes in the spinal canal;
- lesions of the intervertebral discs (and their degree can also be assessed using ultrasound);
- protrusion and herniation of intervertebral discs;
- osteochondrosis;
- osteoarthritis – degenerative changes in the intervertebral joints;
- developmental anomalies of the spinal column.
While X-rays are contraindicated during pregnancy, ultrasound can be performed even on expectant mothers, as it will not harm the embryo or fetus. With the help of modern ultrasound machines, many pathologies can be detected even in the early stages.
CT scan
Computed tomography is a more accurate and informative diagnostic method compared to radiography. This method allows you to create images with layer-by-layer “slices” of certain areas of the body, three-dimensional images. Since CT machines are now available in many clinics, many doctors often prefer it as the first diagnostic method rather than radiography.
The main advantages of computed tomography in the diagnosis of pinched sciatic nerve and spinal pathologies:
- This is a non-invasive, painless and safe method. However, it is worth remembering that, like during radiography, X-ray radiation is used during CT, so the study is contraindicated during pregnancy.
- Computed tomography can clearly visualize many bone and soft tissue pathologies. It is best suited for examining bones and other dense structures.
- Unlike MRI, CT is less sensitive to patient movement and can be performed on people with pacemakers.
- Under the guidance of computed tomography, biopsy (if a tumor is detected) and other invasive procedures requiring navigation can be performed.
Computed tomography is more effective in detecting intervertebral protrusions and hernias compared to radiography. Sometimes, for a more accurate diagnosis, CT myelography is used using radiopaque solutions.
For spinal stenosis, vertebral fractures, infectious processes, and degenerative diseases, CT can provide the doctor with a lot of valuable information, performed alone or in combination with MRI.
MRI
Magnetic resonance imaging, like computed tomography, produces slice-by-slice and three-dimensional images, but uses a strong magnetic field instead of X-rays. Thus, it is a safer diagnostic method. For example, there is no evidence that an MRI scan on a pregnant woman can cause any harm to the unborn baby. However, during pregnancy this study is prescribed with caution and only in cases where it cannot be avoided. MRI is especially undesirable in the first trimester.
MRI is best at visualizing soft tissue, but it can also diagnose bone pathologies. Using this diagnostic method, you can obtain a lot of valuable information about the condition of the spinal cord, its roots and the sciatic nerve. Magnetic resonance imaging helps in planning surgical interventions. Compared to computed tomography, it is better at visualizing tumors, abscesses and other soft tissue formations.
To obtain clearer images, the patient may be given an intravenous gadolinium solution. It is much less likely to cause allergic reactions compared to iodine preparations, which are used for contrast during radiography and CT.
But MRI also has some limitations. Due to the strong magnetic field, it cannot be performed if there are any metal implants or foreign bodies in the patient's body. MRI machines are mainly designed for patients weighing no more than 150 kg. During the study, the person is in a confined space and must lie still, so difficulties arise for people suffering from claustrophobia, mentally ill people in a state of excitement.
Electromyography
Electromyography is a study during which the electrical activity of muscles, nerves, and neuromuscular transmission of impulses is checked. This diagnostic method is prescribed when pinching of the sciatic nerve is accompanied by impaired sensitivity or movement, manifested by the following symptoms:
- Numbness.
- Paresthesia is an unpleasant sensation in the form of tingling, “crawling goosebumps.”
- Muscle pain, spasms.
- Weakness in certain muscle groups, weakened reflexes.
During electromyography, special electrodes are used - they record electrical impulses in tissues. Needle electrodes are inserted directly into the muscles being tested. They are used to study the electrical activity of muscles at rest and under tension. Skin electrodes are placed along the nerve and record passing nerve impulses.
Despite the fact that electroneuromyography can be painful, it is a safe diagnostic method, it does not lead to complications and allows the doctor to obtain important data, assess the cause of deterioration in sensitivity and movements, and the degree of damage to nerve structures.
Densitometry
Densitometry is an advanced form of radiography that measures bone density. The procedure is primarily indicated for older people and is needed in order to figure out whether problems with the musculoskeletal system that lead to pinching of the sciatic nerve are caused by osteoporosis.
Densitometry is a simple test that does not require special preparation. It is similar to a regular x-ray, but uses lower doses of x-rays. Before the procedure, you should not take calcium supplements for at least 24 hours, as this may distort the results.
Bone density is measured at the hip and lumbar spine. The device emits a beam of low-intensity X-rays with two energy peaks. One peak is absorbed by soft tissues, and the second by bone. If you subtract what is absorbed by soft tissue from the total, you get your actual bone mineral density. Densitometry can also be performed in CT and MRI modes. It allows you to detect changes in bone density by 2-5% and detect osteoporosis in the early stages.
Examination by a specialist in soft manual techniques
Diagnosis of pinched sciatic nerve in osteopathy and other areas where soft manual techniques are used has its own specifics. Here, the main diagnostic tool is the doctor’s hands, which, as a result of special training and many years of practice, acquire a special increased sensitivity.
The approaches to understanding the mechanisms of disease development among osteopathic doctors are somewhat different from those adopted in neurology, orthopedics, and neurosurgery. They are based on some key principles:
- The human body is structured and functions as a single integrated system.
- In this system everything is interconnected. Malfunction of one “gear” leads to failures in the entire system. It is important to look for deep cause-and-effect relationships.
- The original cause of the problem may not be located at all where the pathological process developed and the symptoms arose. A classic example: flat feet and problems with the joints of the legs lead to a misalignment of the pelvis and sacrum, because of this, in turn, the lumbar spine suffers, followed by the thoracic and cervical spine, and ultimately this, in combination with other factors, can even cause headaches. It is necessary to identify and eliminate all links in this pathological chain.
- The task of a specialist in soft manual techniques is not to eliminate symptoms or even rid a person of a specific disease, but to generally restore health, the ability to self-recovery and self-healing. Hence the specificity of diagnosis.
During osteopathic diagnostics, the doctor works with the patient at a deep level, detecting the smallest deviations that even modern high-precision diagnostic equipment is unable to detect.
The Bobyr Clinic uses the author’s technique – defanotherapy – which can be classified as a new generation of soft manual techniques. During the first session, the doctor also performs manual diagnostics. The main task of such a specialist is to detect areas of pathological stress that lead to disruption of the correct position and function of the spinal column, difficulty in blood flow and lymph outflow, pinching of nerve roots and trunks, as a result, pain and other symptoms.
During defanotherapy sessions, these problems are corrected using special techniques, and at the end they conduct something like psychotraining and give instructions on the correct position of the spinal column. This helps consolidate the effect and prevent future exacerbations.
If you are worried about lower back pain, lumbago, sciatica, come see a doctor at the Bobyr Clinic.
A specialist will examine you, establish an accurate diagnosis and create an optimal treatment program. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Ultrasound of joints, periarticular tissues and tendons
Ultrasound examination (ultrasound) is an effective method for visual diagnosis of joint diseases. In our clinic you can undergo an ultrasound of all joints, including the temporomandibular joint, knee, hip, shoulder, elbow, wrist, ankle, small joints of the hands and feet. We also perform ultrasound examinations of tendons, muscles, blood vessels and other organs. Ultrasound examination of joints, tendons and muscles is performed by a rheumatologist with a specialization in ultrasound diagnostics or an ultrasound diagnostics doctor.
Preparation for ultrasound of joints. Ultrasound examination of joints does not require special preparation. We recommend that you take with you to the clinic the results of previously performed tests, X-ray results, MRI, if any, and medical reports. These data may be useful for a more accurate interpretation of ultrasound results and for comparing the picture of the current condition of the joint with the results of previously performed studies.
Why do doctors often prescribe an ultrasound of a pair of joints when only one joint hurts? The structure of the joints has some individual characteristics for each person. With an ultrasound of a pair of joints, you can compare the ultrasound characteristics of healthy and diseased joints, thus obtaining more information. This makes it possible to compare joints and evaluate articular and periarticular tissues, adjusted for individual norms.
Ultrasound of joints or x-ray? The main advantage of ultrasound over x-ray examination is the ability to see soft tissues, blood vessels, menisci, articular discs, and surrounding tissues. It is these tissues, not bones, that are most often the source of pain in the joint. Ultrasound allows you to determine signs of inflammation in the joint, ligaments and surrounding tissues (swelling, leakage of fluid into the joint) and then evaluate the effectiveness of treatment by comparing the activity of inflammation in the process of selecting a treatment regimen.
Main indications for ultrasound examination of joints:
- Joint pain, swelling, impaired joint mobility
- Sweating fluid into the joint
- Nerve entrapment by deformed joints and periarticular tissues
- Joint injury
- Arthrosis, arthritis, osteoarthritis
- Dysplasia is a disorder of joint development
Comprehensive study of peripheral nerves of the lower limb
Diseases of the peripheral nervous system, or neuropathy, among adults and children account for about 50% of all diseases, i.e. they rank first in prevalence among other diseases and are found in the practice of doctors of any specialty.
More than 60-65% of the entire group of neuropathies are diseases of the peripheral nerves of the lower extremities. Clinically, they can manifest themselves with a wide variety of clinical symptoms, among which the most common are numbness of individual areas, an increase to mild or significant pain or a sharp decrease (to the point of complete absence) of sensitivity in one or both legs, muscle cramps, dry skin, a feeling of “itching” stop, “freezing” of the feet, disruption of the muscles of the feet, legs and thighs, changes in gait and loss of sense of support.
Price for the service
| Comprehensive study of peripheral nerves of the lower limb | 2500 ₽ |
Frequent causes of pathology of the peripheral nerves of the lower extremities may be:
- Their damage is of various types:
- simple everyday bruises and injuries in places where nerves are located superficially;
- multiple microtraumatization and nerve compression:
- with frequently repeated stereotypical movements;
- with prolonged fixation of the legs in a forced position;
- vibration occupational injuries.
- significant fractures of the pelvic bones, femur, tibia, with traumatic compression or rupture of nerve trunks, muscles and ligamentous-tendon apparatus or after treatment;
To diagnose all of the listed pathologies of the peripheral nerves of the upper extremities, in our center we offer a set of studies, including ENMG (electroneuromyography) and ultrasound examination of the sciatic, femoral, tibial and peroneal nerves along their entire length (from the pelvis to the phalanges of the fingers, including the tibial nerve in the tarsal canal).
Electroneuromyography (2 types: needle and superficial) is a study in which, using electrical impulses, the degree of conduction disturbance is assessed for each nerve examined (median, femoral, tibial, peroneal), and is determined as the level of local conduction disturbance (block at the level of the shoulder, elbow, forearm and hand), and damage at the level of the spinal segment and suprasegmental structures (brain).
A study is being carried out using the Neuro MVP electroneuromyograph . The study includes:
- Neurological examination;
- Hardware assessment of the function of sensory and motor fibers of the nerves being studied;
- Clarification of the degree and level of damage, the amount of muscle tissue involved in the process.
Preparation for the study - clean body surface.
Contraindications based on age and condition: no.
The second study included in the complex is an ultrasound examination of the femoral, sciatic, tibial, and common peroneal nerves along their entire length . The study is being conducted on an expert-class Toshiba Xario digital ultrasound system.
The study includes:
- Visualization of the studied nerves along their entire length, with determination of the level, nature of damage to the nerve trunk, causes of damage, structural disorders, changes in diameter at different levels;
- Visualization of adjacent structures, incl. in the bone canals - bone deformations of the bones of the shoulder, forearm and hand, ligamentous-tendon apparatus, free fluid, bursitis, para-articular cysts, formations that can cause compression;
- Assessment of the degree of limitation of muscle and ligamentous-tendon activity using functional tests of the affected area.
Preparation for the study - no.
Contraindications based on age and condition: no.
Thus, this complex is aimed at a comprehensive assessment of the state of the study of the peripheral nerves of the lower limb, with determination of the level and nature of the lesion, the causes of compression, the extent of dysfunction of the structures innervated by them, and the high efficiency, safety and good tolerability of the methods allows use in adults and children of any age .
Ultrasound of the abdominal organs
An ultrasound of the abdominal organs (pancreas, liver, gallbladder, stomach and spleen) is performed if the development of any disease of the internal organs of the gastrointestinal tract is suspected and the causes of digestive problems, flatulence, diarrhea and constipation, and abdominal pain are established. Most abdominal diseases can be diagnosed or confirmed using ultrasound. Thus, using ultrasound, liver diseases, stones and inflammation of the gallbladder, biliary dyskinesia, pancreatitis, changes in the size of the spleen, etc. are diagnosed.
Abdominal ultrasound requires some preparation.

Ultrasound examination of the abdominal organs. Ultrasound of the pancreas, liver, spleen, gall bladder.
Preparation for abdominal ultrasound Three days before an ultrasound examination of the gastrointestinal tract, we recommend following a diet that reduces gas formation in the intestines. Meals should be in small portions, 4-5 times a day every three to four hours. Limit fluid intake to the consumption of water and weak tea in a volume of about 1.5 liters per day (adjusted for weight and age). The last meal is in the evening (light dinner). Ultrasound of the abdominal organs is performed not only in the morning (on an empty stomach), but also after 15:00. If an ultrasound examination is carried out after 15:00, breakfast is allowed at 8-11 in the morning, after which food and water intake is excluded. We recommend that you take with you to the clinic the results of previously performed tests, the results of a previously performed ultrasound of the abdominal organs, if one was performed, and medical reports. These data may be useful for more accurate interpretation of ultrasound results.
Products recommended for diet before abdominal ultrasound:
- Cereal porridges: buckwheat, barley, flaxseed, water-based oats
- Poultry or beef
- Lean fish – boiled, baked, steamed
- One soft-boiled egg a day
- Reduced fat cheese
Foods excluded from the diet before an ultrasound:
- Raw fruits and vegetables
- Legumes (beans, lentils, peas)
- Dairy
- Fatty meats and fish
- Sweets
- Bread and other baked goods
- Carbonated drinks, strong coffee and juices
- Alcohol
Main indications for ultrasound of the abdominal organs
- Painful sensations in the abdominal area
- Nausea
- Belching
- Increased gas formation
- Increase in size or change in shape of abdominal organs
- Suspicion of tumor neoplasms in the abdominal cavity
- Diagnostics and ultrasound – monitoring the course of diseases of the abdominal organs
Ultrasound diagnosis of femoral and sciatic neuropathy in neurological practice

Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
Introduction
Some of the most common types of pathologies of the nervous system are damage to peripheral nerves and tunnel neuropathies. The incidence of soft tissue injuries involving peripheral nerves, according to various authors, is 25-65% of all cases of injury, and the incidence of tunnel neuropathies is 30-40% of all diseases of the peripheral nervous system [1, 2]. The choice of the most rational methods for diagnosing damage and diseases of the peripheral nerves of the extremities is currently a difficult problem. Existing instrumental diagnostic methods either do not provide images of the nerve trunk (electromyography) or are labor-intensive, requiring complex, expensive equipment (magnetic resonance imaging - MPT). According to a number of foreign authors [3, 4], ultrasound scanning can be quite successfully used in the diagnosis of damage and diseases of peripheral nerves.
Electrophysiological methods, such as electromyography and neuromyography, are traditionally recognized as the “gold standard” for identifying pathology of the peripheral nervous system. However, it should be noted that the information obtained during the above examinations does not provide an idea of the state of the surrounding tissues, does not indicate the nature and cause of damage to the nerve trunk, and does not always accurately reflect the localization of changes. At the same time, it is this information that helps determine the tactics of conservative or surgical treatment. Ultrasound examination (ultrasound) of the peripheral nervous system was first used to diagnose diseases of the nerve trunks in the late 90s of the last century [5], and due to its undeniable advantages over other diagnostic methods, it developed rapidly.
However, despite the publications available in our country on this problem, it should be recognized that the possibilities of ultrasound diagnostics in the assessment of peripheral nerves in chronic pain in the lower extremities remain poorly studied [6].
The purpose of the work was to evaluate the capabilities of ultrasound of the sciatic and femoral nerves in the syndrome of chronic pain in the lower extremities.
Material and methods
This study is based on an analysis of the ultrasound results of 27 patients (18 women, 9 men) aged 30 to 65 years (mean age 47.2 ± 2.4 years) who suffered from chronic pain of the lower extremities.
All patients underwent a comprehensive clinical and instrumental examination, which included a thorough, scrupulous analysis of complaints and medical history, examination by a neurologist, rheumatologist, urologist and/or gynecologist, ultrasound of the femoral and sciatic nerves.
Patients complained of pain with all the features of neuropathic pain, which was often accompanied by the presence of concomitant phenomena such as paresthesia, dysesthesia, allodynia, hyperpathia, hyperesthesia and hypoesthesia. Patients characterized the pain as burning, shooting, stabbing, like an “electric shock”, burning, freezing, piercing with increasing intensity in the gluteal, groin and popliteal areas, limiting the range of movement of the leg. Along with changes in sensitivity, autonomic disorders in the corresponding area were often detected - changes in skin color (hyperemia or cyanosis), impaired tissue trophism, sweating, swelling. As a result, patients had disturbed sleep and had depressive and anxiety disorders. The average duration of pain and limitation of movement ranged from 1 to 3 months.
In terms of diagnostic search to identify possible causes of pain in the pelvic region, 17 patients underwent radiography of the hip joints (coxarthrosis was noted in 16 (94%) patients), and MRI of the lumbosacral spine was performed in 9 patients (degenerative symptoms were detected in 7 (78%) patients). -dystrophic processes). In 15 cases, an ultrasound scan of the pelvic organs was performed, and pathology was detected in 14, including uterine fibroids in 3, signs of external endometriosis in 4, which could be the cause of pain in the buttock and thigh, radiating to the foot, the severity of which depended on phases of the menstrual cycle [7]. 4 men showed signs of chronic prostatitis in combination with benign prostatic hyperplasia of varying degrees.
Ultrasound was performed using modern ultrasound machines with linear sensors with a frequency of 5-13 MHz. During the study, the thickness, structure, and echogenicity of the nerve were assessed. To determine the echogenicity of the nerve, it was compared with the healthy contralateral side and with the adjacent muscles.
It is known that the femoral nerve begins with three branches from the II-IV lumbar spinal nerves, which form a single trunk, descending down between the psoas major and iliacus muscles, and then along the lateral edge of the first (Fig. 1). There are several areas in which the anatomical and topographical features of the femoral nerve predispose to an increased risk of its compression or injury - in the area of the iliopsoas muscle, under the inguinal ligament, in the area of Gunther's canal and at its exit.
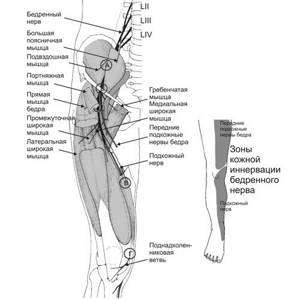
Rice. 1.
Anatomy of the femoral nerve, zone of innervation and the place of its most frequent damage ().
Depending on the level of damage, the clinical manifestations of femoral neuropathy vary significantly.
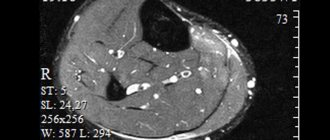
Ultrasound of the femoral nerve was performed with the patient in the supine position. The femoral nerve was visualized in the groin area lateral to the vascular bundle from the level of the inguinal ligament to the upper third of the thigh (Fig. 2, 3). The study was carried out in the transverse and longitudinal scanning planes (Fig. 2, 4).

Rice. 2.
B-mode. Study of the right femoral nerve in the transverse scanning plane at the level of the groin region: BN - femoral nerve, BA - femoral artery.
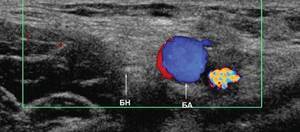
Rice. 3.
Color flow mode. Study of the right femoral nerve in the transverse scanning plane at the level of the groin region: BN - femoral nerve, BA - femoral artery.
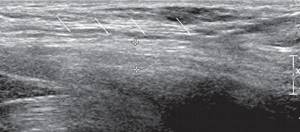
Rice. 4.
B-mode. Examination of the right femoral nerve in the longitudinal scanning plane at the level of the groin region and the upper third of the thigh: arrows - femoral nerve.
The sciatic nerve is the largest peripheral nerve in the human body and exits the pelvic cavity through the greater sciatic foramen under the piriformis muscle (Figure 5). In the area of the gluteal fold, the sciatic nerve is located close to the fascia lata of the thigh, moves laterally and then lies under the long head of the biceps femoris muscle, located between it and the adductor magnus muscle. Depending on the level (height) of the lesion [8], the following types of sciatic nerve neuropathy are possible: very high level, piriformis syndrome (at the level of the infrapiriformis foramen), at the level of the thigh (above the division into the tibial and common peroneal nerves). The topical differential diagnosis of sciatic nerve syndrome often has to be made with discogenic compression radiculopathy LV-SII.
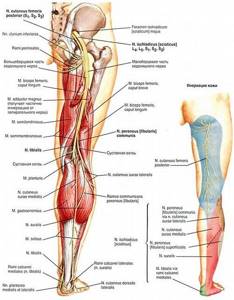
Rice. 5.
Anatomy of the sciatic nerve and innervation zone ().
Ultrasound of the sciatic nerve was performed with the patient lying on his stomach. The sciatic nerve was visualized distal to the ischial tuberosity in the space under the tendons of the semimembranosus and semitendinosus muscles and the long head of the biceps from the gluteal region to the site of division into the tibial and common peroneal nerves. The study was carried out in the transverse and longitudinal scanning plane (Fig. 6, 7).

Rice. 6.
B-mode. Examination of the left sciatic nerve in the transverse scanning plane in the upper third of the posterior surface of the thigh: SN - sciatic nerve.
Rice. 7.
B-mode. Examination of the left sciatic nerve in the longitudinal scanning plane in the upper third of the posterior surface of the thigh: arrows - sciatic nerve.
results
According to ultrasound data, signs of neuropathy were detected in 24 (88.9%) patients. The distribution of identified neuropathies by location and gender of patients based on ultrasound results is presented in Table 1.
Table 1
. Distribution of patients according to the nature of the identified neuropathies.
| Localization of neuropathy | Women | Men | Total | ||||
| abs. | % | abs. | % | abs. | % | ||
| Femoral nerve | Right | 5 | 31,25 | 2 | 25,00 | 7 | 29,20 |
| Left | 4 | 25,00 | 2 | 25,00 | 6 | 25,00 | |
| Sciatic nerve | Right | 2 | 12,50 | 3 | 37,50 | 5 | 20,80 |
| Left | 5 | 31,25 | 1 | 12,50 | 6 | 25,00 | |
| Total | 16 | 100,00 | 8 | 100,00 | 24 | 100,00 | |
In women, damage to the femoral nerve predominated on the right (31.2%), and the sciatic nerve on the left (31.2%); in men, lesions of the sciatic nerve on the right were more often observed, which is consistent with literature data [2].
Normally, the thickness of the femoral nerve at the level of the hip joint in men and women is 0.31 ± 0.08 cm, the thickness of the sciatic nerve in the upper and middle third of the posterior surface of the thigh is 0.4 ± 0.05 cm.
As can be seen from the data in Table 2, with neuropathy there was a uniform increase in the thickness of the nerves: femoral - on average up to 0.56 ± 0.09 cm in women and 0.62 ± 0.20 cm in men; sciatic - on average up to 0.62 ± 0.06 cm in women and 0.66 ± 0.04 cm in men. Local thickening (suspicious of neuromas, schwannomas) or thinning (suspicious of trauma) of the nerve trunks was not detected in our study. In 50% of cases, the echogenicity of the nerve trunks decreased, in 37.5% it was not changed, and in 12.5% it was increased. When comparing the thickness values of the femoral and sciatic nerves obtained during the examination of healthy men and women, as well as when examining the right and left lower extremities, bilateral and gender differences in the parameters turned out to be insignificant.
table 2
. Ultrasound characteristics of neuropathies in gray scale.
| Index | Femoral nerve | Sciatic nerve | ||
| women | men | women | men | |
| Average nerve thickness, cm | 0,56 ± 0,09 (0,47-0,65) | 0,62 ± 0,20 (0,50-0,70) | 0,62 ± 0,06 (0,56-0,68) | 0,66 ± 0,04 (0,62-0,70) |
| Echogenicity, cases | ||||
| decreased normal increased | 5 3 1 | 2 2 0 | 3 3 1 | 2 1 1 |
All patients underwent pathogenetic therapy (muscle relaxants, non-steroidal anti-inflammatory drugs (NSAIDs), B vitamins, anticonvulsants, antidepressants, reflexology - acupuncture, laser puncture), as a result of which 22 showed improvement. During control ultrasound in patients with clinical improvement, a decrease in the thickness of the nerves was noted: femoral - on average to 0.39 ± 0.04 cm in women and 0.40 ± 0.04 cm in men; sciatic - on average up to 0.43 ± 0.02 cm in women and 0.45 ± 0.03 cm in men.
Discussion
Femoral and sciatic neuropathies are fairly common mononeuropathies of the lower extremities [9-11]. Symptoms of femoral neuropathy and other neuropathies are often mistakenly regarded as manifestations of vertebrogenic pathology. According to some studies, in approximately 9% of patients referred to the clinic with a diagnosis of radiculopathy, the cause of pain, sensory and motor disturbances in the lower extremities was actually traumatic and compression-ischemic neuropathies, a significant part of which (more than 10%) were various types of femoral neuropathy.
Diagnosis of lesions of the femoral nerve is primarily based on a thorough neurological examination and analysis of the distribution of sensory and/or motor disorders, identifying their correspondence to the area of innervation of the femoral nerve or its individual branches. At the same time, the topic of damage to the femoral nerve is determined, which, along with anamnestic data, allows us to suggest the etiology of the disease. In practice, femoral neuropathy most often has to be differentiated from vertebrogenic radiculopathies L2-L4. X-ray of the joints of the lower extremities is not of great importance for diagnosing the condition of the femoral and sciatic nerves due to the impossibility of their image. MRI allows you to clearly assess the condition of the corresponding part of the spine and suspect the presence of neuropathy, but does not provide images of the nerves along their length.
Incorrect diagnosis leads to partially or completely inadequate therapy, which, naturally, adversely affects the course of the disease and contributes to its chronicity. Meanwhile, the vast majority of cases of femoral neuropathy, subject to timely initiation and adequacy of treatment measures, are potentially curable. Elimination of the cause of damage to the femoral nerve and early pathogenetic therapy can avoid disabling outcomes, including intractable complex pain syndromes of the pelvic girdle and paresis of the anterior group of the thigh muscle with persistent impairment of walking function.
Pathological tension of the piriformis muscle due to compression of the L1 or S1 root, as well as due to injury, unsuccessful injection, prolonged lying on the back and side (during prolonged operations), posterior muscle compartment syndrome of the thigh can be a manifestation of sciatic nerve neuropathy [8]. The sciatic nerve may be compressed by a tumor or hematoma in the pelvic area, or an aneurysm of the iliac artery.
Therefore, the collaboration of neurologists, urologists, gynecologists, rheumatologists, and ultrasound doctors is so important for a more accurate and detailed differential diagnosis of neuropathies of the femoral and sciatic nerves.
The use of methods for radiological diagnosis of peripheral nerves of the lower limb is limited by the technical capabilities of the equipment and the anatomical features of the location of the nerves [6, 12, 13].
The decisive advantage of ultrasound of peripheral nerves is non-invasiveness, absence of radiation exposure to the patient, real-time examination, as well as minimal economic costs for the examination. Ultrasound allows not only to visualize the sciatic and femoral nerve along its entire length, but also to assess its location, thickness and structure, which in turn helps the neurologist to choose and promptly begin adequate treatment.
Conclusion
Thus, the use in the practice of a neurologist of the ultrasound method of studying nerves allows optimizing the differential diagnostic search for the causes of pain in the lower extremities, as well as minimizing the number of studies performed on a patient with neurological symptoms of peripheral origin, avoiding unnecessary manipulations and studies, reducing radiation exposure to the patient, reduce the cost of its examination and thereby increase the diagnostic efficiency of the studies.
Literature
- Popelyansky Ya.Yu. Orthopedic neurology (vertebroneurology). M.: MEDpress-inform, 2003.
- Popelyansky Ya.Yu. Diseases of the peripheral nervous system. M.: MEDpress-inform, 2005.
- Bianchi S., Martinoli C. Ultrasound of the Musculoskeletal System. Springer-Verlag Berlin Heidelberg New York 2007.
- Peer S., Bodner G. High-resolution ultrasound of the peripheral nervous system. Springer-Verlag Berlin Heidelberg 2008.
- Eskin N.A. Ultrasound diagnostics in traumatology and orthopedics // Ed. Mironova S.P. M.: Publishing house "Social and Political Thought", 2009.
- Saltykova V.G. Ultrasound examination technique and normal echographic picture of the sciatic nerve // Ultrasound and functional diagnostics. 2009. N 6. P. 75-81.
- Shtulman D.R., Levin O.S. Neurology: A Practitioner's Handbook. 5th ed., add. and processed M.: MEDpressinform, 2007. pp. 91-95.
- Samoilov V.I. Syndromological diagnosis of diseases of the nervous system. Volume 1, 2nd ed. St. Petersburg, “SpetsLit”, 2001.
- Khabirov F.A. Guide to clinical spinal neurology. Kazan: Medicine, 2006.
- Elman L., McCluskey L. Occupational and Sport Related Traumatic Neuropathy // The Neurologist. 2004. V. 10. P. 82-96.
- Durrant DH, True JM, Blum JW Myelopathy radiculopathy, and peripheral entrapment syndromes. CRC Press, 2002.
- Jacobson JA Fundamentals of musculoskeletal ultrasound, second edition 2013, 2007 by Saunders, an imprint of Elsevier Inc.
- McNally Eugene. Ultrasound studies of the musculoskeletal system: A practical guide // Transl. from English Khitrova A.N. / Ed. Nazarenko G.I., Geroeva I.B. M.: Vidar M Publishing House, 2007.
Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.