Fine needle aspiration biopsy (FNA) of the thyroid gland is a minimally invasive procedure during which cells are collected for differential diagnosis. The results of the study make it possible to identify an inflammatory process in tissues and confirm the malignant or benign nature of thyroid neoplasms (they are called “nodules”).
The sensitivity of the technique exceeds 99.6%. The manipulation is performed under ultrasound control, which ensures high precision of aspiration (suction) of biological material.
Important: if you have been diagnosed with a thyroid nodule, you do not need to draw conclusions on your own and try to recover from the advice of friends and those found on the Internet. Only a specialist can diagnose the disease and recommend the correct therapy.
A TAB of a thyroid nodule in Moscow can be done for you at the Family Doctor network of clinics. You can make an appointment with a specialist through a mobile application, the patient’s personal account on the website or by phone.
Detailed description of the study
Thyroid nodules (TG) are a widespread pathology. Every year it is diagnosed in approximately 25% of residents of European countries and 20% of residents of the United States. As a rule, most of these formations are benign. These include:
- Hyperplastic colloid goiter - enlargement of the thyroid gland due to the formation of formations consisting of colloidal fluid;
- Thyroid cysts are hollow formations filled with liquid contents;
- Thyroiditis is inflammation of the thyroid tissue;
- Thyroid adenomas are round or oval nodes with a pronounced fibrous capsule.
There are several main reasons for the development of thyroid nodules:
- Iodine deficiency;
- Congenital pathologies of thyroid hormone production;
- Taking medications (amiodarone, lithium) that suppress the synthesis of thyroid hormones.
As a rule, thyroid nodules are asymptomatic. As they grow, patients note an enlargement of the gland itself, in which dense nodes or cysts are detected upon palpation.
There are different forms of thyroid cancer. Thyroid cancer (TC) occurs in less than 10% of cases. There are four main types of thyroid cancer:
- Papillary;
- Follicular;
- Medullary;
- Anaplastic.
Thyroid cancer in most cases also manifests itself as painless nodules. They are often discovered by chance during routine examinations by an endocrinologist or during a preventive ultrasound.
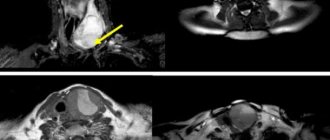
To differentiate malignant and benign thyroid formations, fine-needle aspiration biopsy under ultrasound control is used, followed by cytological examination of the resulting aspirate.
Cytological examination is prescribed in the following cases:
- The presence of a thyroid node or several nodes in patients with normal levels of thyroid hormones;
- Inconsistency between ultrasound examination data and clinical picture;
- Enlargement of the thyroid gland or other changes in the organ.
The material is taken using a special aspiration needle under ultrasound control; control is necessary for targeted extraction of material from the lesion and to eliminate possible errors.
At the National Cancer Institute in Bethesda (USA), a classification system for interpreting the results of FNA of the thyroid gland was developed. The classification included six points assessing the risk of malignancy of nodules.
- DCI - “Uninformative material”, in this case it is necessary to perform a repeat TAB, since the drug has disadvantages in the form of a small amount of material, its poor fixation and other signs that make diagnosis impossible.
- DCII - “Benign formation”, in this case we can talk about a low risk of malignancy. For such patients, clinical and ultrasound monitoring of nodular formations over time and tracking the size of the nodule are recommended.
- DCIII - “Follicular lesion of undetermined significance/atypia of undetermined significance.” The risk of malignancy of the formation is 10 – 30%. Such patients are recommended to undergo repeat FNA, molecular genetic testing or hemithyroidectomy (removal of the thyroid lobe with formation and subsequent pathological examination).
- DCIV - “Follicular neoplasia / suspected follicular neoplasia.” The risk of malignancy of the neoplasm is 25-40%. Such patients are recommended to undergo molecular genetic testing or hemithyroidectomy to clarify the results of the study.
- DCV - “Suspected malignancy”, in this case they speak of a high risk of malignancy (50-75%). This term is used when papillary, medullary, metastatic thyroid cancer or lymphoma is suspected. Upon receipt of such a cytological conclusion, it is recommended to conduct additional laboratory tests, which are prescribed by the attending physician. Surgical treatment (thyroidectomy) is also recommended.
- DCVI - Malignant neoplasm. The risk of malignancy is 97-99%. The presence of undeniable signs of cancer. A thyroidectomy or hemithyroidectomy is necessary.
To form a correct conclusion on the analyzed preparation, it must contain at least six groups of clearly visible cells of the epithelial component.
Cytological examination in the diagnosis of thyroid diseases is highly specific and allows you to accurately differentiate benign and malignant neoplasms, determine the stage of malignancy in order to plan further treatment and management of the patient.
How is TAPB performed?
The manipulation is practically no different from a conventional intramuscular injection: it is low-traumatic, low-painful, performed on an outpatient basis and does not require any special preparation. In rare cases, a biopsy may be performed under local anesthesia. The duration of the procedure is no more than 1-2 minutes.
Under the control of an ultrasound machine, the exact location of needle insertion is determined on the front surface of the neck. Then the skin is pierced with a thin needle and, under the control of the image on the device’s monitor, it is inserted directly into the tissue of the node. After this, several translational movements are made with the needle to maximize the filling of the canal with formation cells. Then the needle is removed, and the resulting puncture material is transferred to several glass slides and sent for cytological examination. Most often, the material is taken from 2-3 places in the node, which requires 1 to 3 punctures.
References
- Troshina, E.A., Sviridenko, N.Yu., Vanushko, V.E. and others. Federal clinical guidelines for the diagnosis and treatment of thyrotoxicosis with diffuse goiter (diffuse toxic goiter, Graves-Bazedow disease), nodular/multinodular goiter, 2014. - 25 p.
- Semkina, G.V., Abrosimov, A.Yu., Abdulkhabirova, F.M. and others. Comparative analysis of cytological reports and diagnostic categories of independent cytologists. Clinical and experimental thyroidology, 2013. - No. 3. — P.29-34.
- Singaporewalla, R., Hwee, J., Lang, T. et al. Clinico-pathological Correlation of Thyroid Nodule Ultrasound and Cytology Using the TIRADS and Bethesda Classifications, 2021. - Vol. 41(7). — P.1807-1811.
What is the way out?
One of the most promising ways out of the situation is partial removal of the thyroid tissue, namely the damaged lobe. In this case, the patient, firstly, gets rid of the need to take lifelong replacement therapy with thyroid hormones, and secondly, avoids the serious consequences that come with the operation of complete removal of the thyroid gland. However, it is worth understanding that this option does not apply to large tumors, as well as those neoplasms that could potentially be aggressive (the doctor decides this!).
Now therapists and surgeons who deal with the pathology of the thyroid gland are divided into two camps: those who believe that it is better to play it safe and, if even the smallest tumor is detected, remove the entire thyroid gland, and those who believe that the best solution is partial removal of the tissue gland, namely its damaged lobe. Unfortunately, this question still remains open. Doctors still cannot come to a common denominator on this issue. The problem is that there is no reliable objective evidence base on which doctors can rely as current clinical guidance. There are only a few studies that examine the issue from only one subjective side [21]. The optimal solution to this problem, in our opinion, would be to combine all existing articles with an objective and comprehensive look at this issue. However, such research only awaits us in the future.
Final chord
So, here we come to the last lines of our article. It might seem that we are completely against ultrasound of the thyroid gland, but this is not so. There is a risk group of patients who need to have an ultrasound of the thyroid gland (for example, a family member has thyroid cancer). It is also impossible to ignore the fact that ultrasound has greatly advanced doctors in the early diagnosis of aggressive, fast-acting forms of thyroid cancer. However, most endocrinologists, especially abroad, are against doing an ultrasound of the thyroid gland when there are no symptoms of the disease! Essential reading, in our opinion, is the work of Professor V.V. Fadeev. “Just in case...” [28].
In this article, a highly qualified doctor draws the reader’s attention to the fact that doctors often evaluate the results of laboratory and instrumental tests only on the basis of generally accepted norms. In case of non-compliance with this “norm”, the patient is considered sick. It is very important to understand that a person is an individual, and the norm for each person can vary depending on the characteristics of the body. Therefore, we must treat not the tests, not the disease, but the patient . The doctor needs to evaluate not only the numbers on the test sheet, but also the patient’s condition, as well as the quality of life that awaits the person after treatment. This is called clinical thinking, which, unfortunately, is often absent from doctors in an age when we want to blindly trust numbers, and a machine begins to think for a person.
You can familiarize yourself with these and other thoughts at the link we left [26].
So, our dear readers! Based on everything we've covered above, we'd like you to draw three main conclusions:
- Do not do an ultrasound of the thyroid gland “just in case”, without any symptoms! Not on the advice of a friend, not because they said so on TV, not even if the doctor told you so (only if he clearly explains why you need to do an ultrasound).
- If you have a nodule, there is a 90% chance that it is benign.
- If you fall into the remaining 10%, remember that most thyroid cancer responds well to treatment and has a favorable prognosis.
Have a nice day everyone, and take care of your thyroid glands and nerves. 

Preparation for the procedure
Fine-needle biopsy does not require special preparatory measures. During the procedure, the patient is conscious. But there are a number of rules that should be followed before taking biological material:
- inform the doctor about taking medications, allergies, poor blood clotting,
- fill out the necessary documents confirming consent to carry out such manipulation,
- undergo all necessary tests,
- Before the procedure, you should remove all jewelry and other objects that may interfere with the procedure.
To perform an open biopsy, you should avoid eating approximately 8 hours before the procedure.
Important advice from endocrine surgeons
“Determine calcitonin in the blood before performing TAB!”
Calcitonin is a tumor marker for the most malignant and dangerous tumor of the thyroid gland - medullary carcinoma. Even a slight increase in calcitonin is a reason for a biopsy of all detected nodes even less than 1 cm in size. In our institution, the doctor will certainly perform such a puncture if this indicator is elevated. It is necessary to donate blood ONLY in a specialized laboratory of the North-Western Endocrinology Center. No preparation is required for the test.
Thanks to this tactic, patients with medullary cancer ranging in size from 3 and 6 mm were operated on at our institution, and their lives were saved. In terms of the number of diagnosed medullary cancer in Eastern Europe and Russia, the North-Western Center for Endocrinology and Endocrine Surgery is the leader.
Early detection of this type of cancer and prompt surgical treatment is the only way to defeat the disease and give yourself a future life!