Hypothyroidism
is a pathological condition caused by a long-term lack of thyroid hormones. With compensatory therapy, the symptom goes away, but in chronic, congenital and complicated forms it can lead to serious consequences. The extreme degree of manifestation of the pathology in adults is myxedema (swelling of organs and tissues), in children - cretinism (delayed physical and mental development).
The danger of the disease lies in minor, slowly developing clinical manifestations. The symptoms are vague, which does not allow the patient to timely replace the changes occurring in his body. The condition resembles various pathologies and diseases, so many doctors do not pay due attention to the complaints of patients. They are not sent for a test that determines the level of thyroid hormones in the blood.
Symptoms of hypothyroidism
- Weakness and fatigue immediately after waking up.
- Slowness, sleepiness during the day.
- Increased fatigue, decreased performance.
- Memory deterioration, difficulty learning new information.
- Swelling of the face, fingers and toes.
- Dry skin, brittle nails, hair loss.
- Deepening of the voice.
- Decreased immunity, frequent infectious diseases.
From the gastrointestinal tract, disruption of the thyroid gland is manifested by frequent constipation. Paresthesia of the hands and feet and cold intolerance may occur. Women experience menstrual cycle disorders: from menorrhagia (heavy menstruation) to amenorrhea (its complete absence).
Over time, a persistent lack of hormones leads to personality changes and depression. In some cases, psychosis (myxedematous madness) may develop. The severity of hypothyroidism symptoms depends on the degree of hormone deficiency and the individual characteristics of the body.
In children, thyroid dysfunction causes:
- physiological jaundice;
- constipation;
- swelling of the mucous membranes;
- poor weight gain;
- bradycardia (irregular heart rhythm);
- hypothermia (low body temperature).
Hypothyroidism in the first year of life leads to delays in physical and mental development. The congenital form is characterized by a large tongue and narrow palpebral fissures. The fontanelle closes later than in other children, and teething is also delayed.
Classification
Hypothyroidism can be congenital or acquired, including after surgery on the thyroid gland and resection (removal of most of the organ).
Pathogenetically, the syndrome is divided into:
- Primary - developed against the background of a decrease or increase in secretory function (thyroidogenic).
- Secondary - arising due to dysfunction of the pituitary gland (pituitary).
- Tertiary - caused by neuroendocrine disorders, absence or deficiency of thyroliberin due to damage to the hypothalamus (hypothalamic).
- Tissue - caused by peripheral defects in the action and metabolism of thyroid hormones (transport, peripheral).
Primary hypothyroidism is the most common (in 93% of cases). The rarest form of the syndrome is tissue. Its development can be caused by periods of hunger, anorexia, surgery and long-term use of certain medications.
According to the severity of the pathological condition, hypothyroidism is divided into several stages:
- Subclinical or latent (increased levels of the teriotropic hormone TSH, with normal levels of thyroxine T4).
- Manifest stage (TSH level is increased, T4 level is decreased).
- Complicated hypothyroidism (severe form of the syndrome) Leads to heart failure, cretinism, effusions in the serous cavities, pituitary adenoma. Without therapeutic treatment, it leads to myxedematous coma.
A coma state is an extreme stage of hypothyroidism that occurs in the absence of treatment or as a result of improper therapy. Caused by inhibition of tissue respiration, kidney and adrenal function. In 80% of cases it leads to death.
Hypothyroidism is relatively common, affecting approximately 2-3% of the general population, and is caused by a decrease in the blood levels of one or both thyroid hormones.
Clinically, hypothyroidism is manifested by the following symptoms
- dry skin,
- increase in body weight,
- loss of appetite,
- drowsiness,
- lethargy,
- intolerance to cold,
- puffiness of the face,
- bradycardia.
In the vast majority of cases (90-95%), hypothyroidism is caused by a pathological process in the thyroid gland. Serum free T4 and TSH are the best combination of tests to diagnose hypothyroidism. In hypothyroidism, the basal TSH level is increased due to primary damage to the thyroid gland (primary hypothyroidism) and decreased due to primary failure of the pituitary gland (secondary hypothyroidism) or hypothalamus (tertiary hypothyroidism).
- In primary hypothyroidism, the basal level of free T4 is often reduced, and low values of T3 and T4 are often recorded. The T4 level may decrease by 2 or more times; the decrease in T3 is less pronounced or absent.
- Secondary hypothyroidism is characterized by a low level of TSH against the background of reduced concentrations of free T4, total T4, and T3.
- In tertiary hypothyroidism, the level of TSH, free T4, T4, T3 in the blood is often reduced. The TRH level, in contrast to secondary hypothyroidism, is reduced.
Using TRG, it is possible to differentiate between various clinical forms of hypothyroidism. For hypothyroidism, there may be 3 possible answers to the TRH test (see below):
- Abnormal increase in TSH level in primary hypothyroidism;
- Complete lack of response in secondary hypothyroidism;
- Delayed and incomplete response in tertiary hypothyroidism.
TRH test - after intravenous administration of thyroxine-releasing hormone (thyroliberin) in healthy individuals, the TSH level increases by 300-1000% within 20-30 minutes. If hyperthyroidism is suspected with a normal basal TSH concentration in the blood, a negative response to TRH administration confirms the diagnosis of hyperthyroidism, while a positive response excludes it.
Algorithm for diagnosing hypothyroidism and evaluating research results
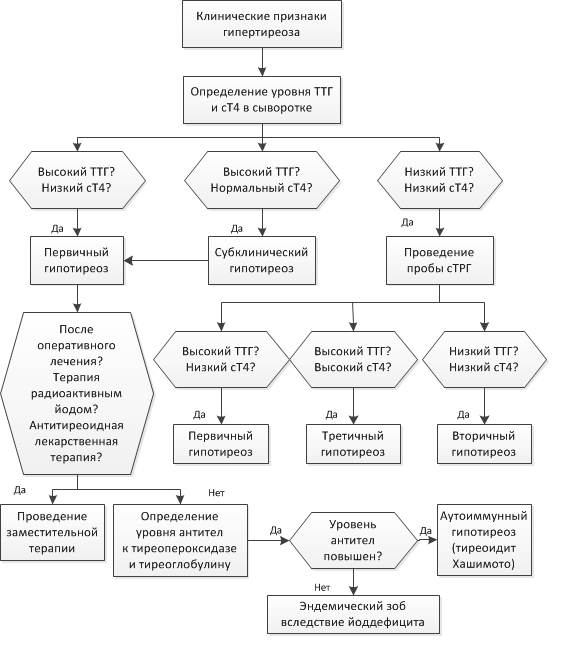
An increase in the level of TSH in the blood is (with rare exceptions!) the earliest laboratory sign of thyroid failure. An increase in TSH levels portends an exponential decrease in free T4: when free T4 decreases by 2 times, TSH secretion increases 100 times! In this regard, an increase in TSH against the background of normal levels of free T3 and T4 is called subclinical hypothyroidism. There are 3 degrees (stages) of the development of subclinical hypothyroidism with various clinical and hormonal manifestations:
- I degree – minimal thyroid insufficiency. The TSH level is within the reference values (2-5 mIU/l) or slightly elevated (but less than 6 mIU/l) and a hyperergic reaction of TSH to TRH stimulation is noted.
- II degree is similar to I, but the increase in TSH progresses and lies in the range of 6-12 mIU/l, the prognosis for the clinical manifestation of hypothyroidism increases significantly.
- III degree - TSH values in the blood above 12 mIU/l, an erased clinical picture of hypothyroidism, as well as a high risk of developing overt hypothyroidism, usually over the next 10-20 years.
The level of TSH and antibodies to thyroid peroxidase in the blood serum is an indicator for assessing the prognosis of the manifestation of hypothyroidism. It has been proven that TSH levels in the range of 2-4.2 mIU/l in combination with subclinical levels of antibodies to thyroid peroxidase in the blood serum are critical parameters for the progression of decreased thyroid function. The presence of an increase in only TSH or only antibodies determines a lower, but significantly increased risk of pathology (5-8 and 25-44 times, respectively).
Laboratory criteria for assessing the effectiveness of treatment of primary hypothyroidism Therapy is considered effective when the levels of TSH and free T4 are normalized. Dynamic control over the level of these markers allows you to approach the selection of drug doses individually. The TSH level, as a rule, normalizes slowly, especially with long-term hypothyroidism, so if the patient’s condition has improved and the level of free T4 is within normal limits, then there is no need to increase the dose of the thyroid drug just to achieve a normal TSH level. After selecting the optimal dose of the drug, annual TSH monitoring is necessary. With age, the need for thyroid hormones decreases, and the dose of L-T4 is reduced in accordance with the level of TSH in the blood. It must be remembered that the half-life of T4 is long, as a result of which the level of TSH in the blood should be determined no earlier than 4 weeks after changing the dose of L-T4. Experts from the US National Academy of Clinical Biochemistry believe that, from a practical point of view, minimal thyroid deficiency, as a stage of hypothyroidism, should be taken into account when prescribing replacement therapy. When selecting treatment, it is recommended to maintain the TSH level in the blood in the range from 0.5 to 1.5 mIU/l.
Reasons for development
In adults, with rare exceptions, acquired hypothyroidism is diagnosed. The main reasons for the development are:
- tumors of the hypothalamic-pituitary region;
- surgical intervention;
- radiation exposure.
Long-term insufficient intake of iodine from food increases the risk of the syndrome. Irregular, unbalanced diet, rare consumption of seafood.
Congenital hypothyroidism is caused by pathology of the thyroid gland. This includes hypoplasia, i.e. reduced volume of the gland with unchanged tissue, partial (aplasia) or complete absence (agenesis) of the thyroid gland or its isthmus. Over time, the mass of glandular tissue continues to decrease, and the production of hormones decreases. As a result, the pathology leads to serious illnesses and critically life-threatening conditions.

A lack of thyroid hormones during pregnancy is especially dangerous. According to medical statistics in Russia, 5% of pregnant women have reduced activity of the thyroid gland. This condition can negatively affect the development of the fetus. Hormones T3 and T4 are involved in all processes of maturation, development and growth of cells, tissues, and organs. Without correcting the condition, the risk of placental abruption, premature birth and delayed development of the child increases.
Medical testing for thyroid diseases
The thyroid gland is involved in regulating metabolism. The gland produces hormones that are responsible for the process of energy use. Almost all cells and organs are under the influence of thyroid hormones. An imbalance of thyroid hormones leads to disruptions in the functioning of most systems and organs. Thyroid hormones
The thyroid gland uses iodine, obtained mainly from food, to produce hormones. The most important hormones are thyroxine (T4) and triiodothyronine (T3), which account for 99.9% and 0.1% of thyroid hormones in the blood, respectively. When released from the gland, the T4 hormone is converted into the T3 hormone, an active hormone that affects cell metabolism. At the peripheral level, it is the T3 hormone that has the main physiological effects.
The activity of the thyroid gland is controlled by the pituitary gland. The pituitary gland influences the activity of the gland through thyroid-stimulating hormone (TSH). When the thyroid gland reduces the production of its hormones, the pituitary gland produces additional TSH in an attempt to stimulate the organ. In cases where the production of hormones is increased, the pituitary gland suppresses the production of TSH, stimulation of the gland occurs to a lesser extent. Thanks to this system of regulation of the organ's functioning, called a “negative feedback loop,” the level of thyroid hormones is kept within a certain range of values.
Failure of an organ can occur at any level: the thyroid gland, pituitary gland or peripheral tissues, leading to the development of hyper- and hypothyroid conditions.
When thyroid hormones are produced in excess, hyperthyroidism develops, and when there is a deficiency, hypothyroidism develops. In 95% of cases, the pathology is present in the organ itself, the remaining 5% are due to diseases of the hypothalamic-pituitary system.
Medical diagnosis of hyperthyroidism
Hyperthyroidism is associated with a condition where the body suffers from high levels of T3 and T4 hormones. This condition is also called thyrotoxicosis. The most common cause of hyperthyroidism is the autoimmune disease Graves' disease. With this disease, the body produces special antibodies to the thyroid tissue, which cause the thyroid gland to produce hormones in excess quantities.
Hyperthyroidism can be caused by toxic nodular or multinodular goiter, which are growths of glandular tissue capable of producing hormones. In addition, excessive iodine consumption and uncontrolled use of iodine-containing drugs also leads to hyperthyroid conditions.
Symptoms of hyperthyroidism:
- fatigue and muscle weakness;
- hand tremors;
- mood swings;
- nervousness or restlessness;
- fast heartbeat;
- dry skin;
- sleep problems;
- weight loss;
- increased frequency of bowel movements.
Medical Diagnosis of Hypothyroidism
Hypothyroidism is associated with an underactive thyroid gland. There are two main causes of the disease.
The first is the result of previous or current inflammation in the thyroid tissue. The inflammatory process leads to damage to a large percentage of organ cells, which become unable to produce sufficient amounts of hormones. The most common cause of thyroid failure is autoimmune thyroiditis, also called Hashimoto's thyroiditis.
The second main reason falls into the category of “therapeutic procedures”. Treatment for many thyroid conditions requires surgical removal of part or all of the organ. If the total mass of thyroid cells left in the body is not enough to meet the body's needs, hypothyroidism develops. Such operations are performed for thyroid cancer.
Symptoms of hypothyroidism:
- fatigue;
- increased sensitivity to cold;
- constipation;
- dry skin;
- weight gain;
- plump face;
- hoarseness of voice;
- muscle weakness and pain;
- increased blood cholesterol levels;
- pain, stiffness, or swelling in the joints;
- irregular menstrual periods that are difficult;
- Thin hair;
- slow pulse;
- depression;
- weakened memory.
Depending on the severity of the thyroid hormone deficiency and the length of time during which the body was deprived of the required amount, the list of symptoms and their severity will vary. Some patients with hypothyroidism have no symptoms or are so mild that they go unnoticed. There are often cases when symptoms of the disease, for example, fatigue or weight gain, are mistakenly associated with age-related changes and therefore hypothyroidism remains undiagnosed for a long time. Diagnosis of thyroid diseases
To diagnose the functions of the thyroid gland, laboratory and instrumental diagnostic methods are used. The doctor orders one or more blood tests to confirm the diagnosis. Screening laboratory tests include blood tests for thyroid-stimulating hormone (TSH), T4, T3, and thyroid antibody tests.
Blood tests to check thyroid function
1) TSH test
TSH is a hormone produced in the pituitary gland that tells the thyroid gland how much T4 and T3 to synthesize.
A high TSH level often means there is organ failure. The thyroid gland does not produce enough hormone, but the pituitary gland continues to synthesize and secrete TSH.
When hypothyroidism occurs, there is usually a lack of the hormones T3 and T4 in the blood, which can be directly measured. However, at the onset of the disease, the level of these hormones may still be normal. Thus, the main tool for detecting hypothyroidism is measuring thyroid-stimulating hormone levels.
Low TSH levels indicate that the thyroid gland is overactive and produces too much hormone, so the pituitary gland inhibits TSH synthesis.
If the TSH test results are not normal, you will need at least one more test to help find the cause of the problem.
2) T4 test
A high level of T4 in the blood may indicate the presence of hyperthyroidism, while a low level may indicate hypothyroidism.
In some cases, high or low T4 levels are not related to thyroid problems. During pregnancy or while taking oral contraceptives, the level of thyroid hormones will be higher. Taking corticosteroids helps reduce T4 concentrations. Medicines and some conditions change the amount of blood proteins that “bind” and transport the hormone.
Bound T4 is stored in the blood until needed. “Free” T4 is not bound to carrier proteins and is available to target tissues. Therefore, many doctors prefer to measure free T4.
3) Test T3
In cases where hyperthyroidism is suspected and the T4 value is within the normal concentration range, the T3 level must be determined. Sometimes T4 is normal but T3 is high, so it is important to measure the levels of the two hormones at the same time. Like the T4 hormone, it is possible to determine two fractions of T3: total and free. Free T3 has the main biological effect and is therefore of greater interest in diagnosing hyperthyroid conditions.
4) Thyroid antibody tests
Testing thyroid antibodies can help diagnose autoimmune thyroid disorders such as Graves' disease, the most common cause of hyperthyroidism, and Hashimoto's disease, the most common cause of hypothyroidism. Thyroid antibodies are formed when the immune system mistakenly attacks the thyroid gland. There are two main types of antibodies that are determined in the laboratory: antibodies to thyroid peroxidase and antibodies to thyroglobulin.
Treatment
An endocrinologist treats diseases of the thyroid gland. The prognosis of the disease is quite successful, especially when organ dysfunction is detected in the early stages. The results of treatment largely depend on the causes of the disease.
Risk factors
- Women during pregnancy.
- Women over 60 years of age.
- Persons who have relatives with thyroid diseases.
- Patients after thyroid surgery.
- Having autoimmune diseases (rheumatoid arthritis, Libman's disease, type 1 diabetes).
- Patients who have been treated with radioactive iodine, antithyroid drugs, or irradiation of the neck or chest area.
- Living in areas with increased background radiation.
The syndrome can occur in any person, but the likelihood of its development increases with age. Iodine deficiency also has a negative effect. This trace element is necessary for the production of thyroid hormones. According to WHO, about 85% of Russians live in areas with iodine deficiency. The element is lacking in the soil and, as a result, in grown vegetables and fruits.
Causes of hypothyroidism
Primary hypothyroidism
- Chronic autoimmune thyroiditis
- Iatrogenic hypothyroidism: thyroidectomy, radiation therapy
- Iodine deficiency or excess
- Some drugs - amiodarone, interferon-alpha, interleukin-2, perchlorate, tyrosine kinase inhibitors
- Infiltrative diseases – fibrous thyroiditis, hemochromatosis, sarcoidosis
- Transient hypothyroidism
- Thyroiditis
- Subacute granulomatous thyroiditis
- Postpartum thyroiditis
- Partial thyroidectomy: hypothyroidism develops after removal of the thyroid gland
- Consequences of treatment of Graves' disease with radioactive iodine
- Withdrawal of thyroid hormone treatment in euthyroid patients
Secondary or central hypothyroidism
- TSH deficiency
- TRH deficiency
Complications
If you ignore the disease, avoid treatment or do not receive it in full, this can lead to the following disorders:
- Damage to the nervous system, expressed in muscle weakness, pain in the limbs. Violation can lead to the development of carpal tunnel syndrome, gait and speech disorders.
- Suppression of kidney function, which means slower fluid removal, which leads to swelling.
- Heart rhythm disturbances and subsequent heart failure. An accumulation of fluid in the pericardium that compresses the heart, preventing it from making adequate heartbeats.
- Infertility in men and women. Hypothyroidism causes miscarriages, premature births and preeclampsia, a dangerous condition during pregnancy characterized by high blood pressure.
A life-threatening complication of hypothyroidism is hypothyroid coma. It is rare, primarily in the age category of citizens who have not been treated or received insufficiently qualified care. Clinical symptoms increase gradually. First, drowsiness is noted, bradycardia occurs, body temperature drops to +34 C. The patient is disoriented, is in a comatose state, does not respond to external stimuli, and may lose consciousness. Patients in hypothyroid coma require emergency care because they may die from cardiac tamponade, respiratory failure, and heart failure.
Correct and timely treatment will help to avoid complications of hypothyroidism. To do this, it is necessary to diagnose thyroid dysfunction as early as possible.
Diagnosis of hypothyroidism
To identify disorders of the thyroid gland, it is enough to undergo three tests:
- Analysis for total and free triiodothyronine (T3).
- Analysis for total and free thyroxine (T4).
- Analysis of the level of thyroid-stimulating hormone (TSH).
Normally, the T3 level ranges from 3.1 to 6.8 pmol/l, and the reference values for T4 are 10.8 - 28.3 pmol/l. Hormone levels decrease in proportion to the severity of the disease. To confirm hypothyroidism, it is necessary to re-determine hormone levels after 2 to 3 months, because in some cases, elevated values may be transient.
Additionally, the following may be prescribed: a general and biochemical blood test, an analysis of serum cholesterol levels, a test for thyroxine-binding proteins, antibodies to thyroglobulin and thyroid peroxidase. The presence of antibodies is a sign of an autoimmune pathology.
In some cases, ultrasound diagnostics of the thyroid gland can be performed. An instrumental study is prescribed for patients at risk, since it can reveal characteristic changes before the appearance of antibodies.
Screening for hypothyroidism should be carried out when planning pregnancy and in pregnant women in each trimester. Patients with a family history, in connection with professional activities, after head injuries, stroke, radiation. These individuals are 29% more likely to develop the syndrome than the average Russian.
Hypothyroidism
Hypothyroidism is a disease of the endocrine system characterized by a lack of thyroid hormones. These hormones regulate metabolism, affect the emotional background, and the body’s resistance to stress and stress.
A lack of thyroid hormones can lead to serious health problems: disrupt the functioning of the heart and kidneys, cause obesity, reduce immunity, and lead to infertility. Hypothyroidism most often manifests itself in adulthood, mainly in women. Slow development of the process is the main reason for late detection of the disease. Patients rarely attach importance to such initial symptoms as lethargy, apathy or forgetfulness, attributing them to overwork and lack of vitamins.
Despite the fact that laboratory diagnosis of hypothyroidism is not difficult, most patients consult a doctor already at the stage of development of complications that require additional treatment. A severe form of hypothyroidism is called myxedema. It can be avoided by taking synthetic hormonal drugs in a timely manner. Their dose is selected by an endocrinologist based on laboratory tests.
Synonyms Russian
Gall's disease, hypothyroidism, myxedema.
English synonyms
Hypothyroidism, Myxedema.
Symptoms
Clinical manifestations of hypothyroidism largely depend on the severity of hormonal deficiency and are quite varied. The process develops slowly and takes several years. If left untreated, the condition may worsen. In severe, advanced cases, a coma develops (myxedema coma).
Hypothyroidism is manifested by the following symptoms:
- lethargy and apathy;
- muscle weakness and muscle pain;
- stiffness and pain in the joints;
- pale, dry skin;
- swelling;
- brittle nails and hair;
- increased cholesterol levels;
- unexplained weight gain;
- increased sensitivity to cold, chilliness.
General information about the disease
The thyroid gland is one of the most important glands of the endocrine system. It is located on the front surface of the neck and consists of two lobes that, in the form of butterfly wings, cover the trachea. The hormones produced by the thyroid gland, thyroxine (tetraiodothyronine, or T4) and triiodothyronine (T3), are involved in the regulation of almost all metabolic processes in the body. Iodine is required for their formation.
Insufficient iodine intake from food is one of the main causes of hypothyroidism. This is common in countries where seafood consumption is low.
Other reasons include:
- autoimmune thyroid diseases (Hashimoto's autoimmune thyroiditis);
- previous operations on the thyroid gland;
- radiation therapy;
- taking certain medications that have a toxic effect on the thyroid gland.
Rarer causes include:
- congenital underdevelopment of the thyroid gland and pituitary gland;
- severe toxicosis and hypoxia in pregnant women.
To establish the cause of thyroid hormone deficiency, an endocrinologist needs to conduct a thorough examination.
Thyroid hormones are involved in the regulation of fat and carbohydrate metabolism, thereby affecting body weight, providing thermoregulation of the body and even affecting heart rate. A deficiency or excess of thyroid hormones can significantly change a person’s appearance, behavior and emotional background.
The third thyroid hormone, calcitonin, regulates calcium levels in the blood.
Thyroxine and triiodothyronine are synthesized by the thyroid gland under the influence of thyroid-stimulating hormone from the pituitary gland, which is located at the base of the brain and is the main regulator of the thyroid gland. The signal for the production of thyroid-stimulating hormone is a decrease in the levels of T3 and T4 in the blood. In this way, the chemical relationship between the endocrine glands is carried out. Disruption of this relationship can lead to insufficient thyroid function and secondary hypothyroidism.
There is also tertiary hypothyroidism. It occurs when the hypothalamus, the center of endocrine regulation of the entire organism, located in the brain, does not work properly.
Who is at risk?
- Women over 50 years old.
- Persons living in areas with iodine deficiency.
- Residents of areas with increased background radiation, as well as those exposed to radionuclide contamination.
- Persons suffering from autoimmune diseases or having close relatives with this pathology.
- Previously operated on due to pathology of the thyroid gland.
- Have been treated with radioactive iodine or have undergone radiation therapy to the neck area.
Diagnostics
Diagnosis of hypothyroidism is quite simple and involves determining the level of thyroid hormones. Significant difficulties can arise in identifying the causes of hypothyroidism, especially its second and third types.
General clinical studies
- Complete blood count (without leukocyte formula and ESR). Impaired absorption of iron is one of the manifestations of hypothyroidism. A general blood test may show a low hemoglobin level with a normal or reduced number of red blood cells (anemia).
- A biochemical blood test reflects the consequences of disorders of water-salt and fat metabolism. With severe hypothyroidism, sodium levels may decrease, creatinine levels may increase, and, in some cases, liver enzymes.
Tests confirming low thyroid hormone levels
- Thyroid-stimulating hormone (TSH) is a pituitary hormone. Its elevated level may indicate decreased thyroid function. The results are taken into account under the condition of normal pituitary function. If low levels of TSH and thyroid hormones are simultaneously detected in the blood, secondary hypothyroidism can be suspected.
- Total and free triiodothyronine (T3). A reduced level of free T3 in the blood is important.
- Total and free thyroxine (T4). The level of this hormone is also reduced in hypothyroidism.
- Thyroxine-binding proteins (t-uptake). This test is designed to identify proteins that transport thyroid hormones to organs and tissues. The percentage of free and bound transport proteins can be determined by laboratory testing. In hypothyroidism, it is shifted towards free (not associated with the hormone) proteins.
- Serum cholesterol. Hypothyroidism is characterized by an increased concentration of cholesterol.
To exclude the autoimmune nature of hypothyroidism, tests are performed for:
- ATTG – antibodies to thyroglobulin, a protein that is the basis for the production of thyroid hormones;
- ATTPO – antibodies to thyroid peroxidase, a protein found only in thyroid cells; The level of these antibodies may be increased in autoimmune diseases.
Additional Research
The scope of additional examination is determined by the attending physician in each specific case.
- Ultrasound examination of the thyroid gland allows you to assess the size and structure of the gland and identify focal formations in it.
- A radioisotope study shows the ability of the gland to accumulate iodine, the size of the gland, and the presence of space-occupying lesions.
- Puncture biopsy - study of the cellular composition, in case of nodular lesions - exclusion of a malignant nature.
- Electrocardiogram. In the later stages of hypothyroidism, there are changes on the ECG.
- Chest X-ray reveals an increase in heart size.
Treatment
Treatment for hypothyroidism involves taking medications containing synthetic thyroid hormones. The endocrinologist selects the required dose based on the level of hormones in the blood. If the autoimmune nature of hypothyroidism is confirmed, the underlying disease is treated.
Prevention
The basis for preventing hypothyroidism is replenishing iodine deficiency in the body: eating iodized salt and seafood.
Recommended tests
- Antibodies to TSH receptors (anti-pTTH)
- Antithyroglobulin antibodies (antiTG)
- Antibodies to thyroid peroxidase (anti-TPO)
- Serum calcitonin
- Thyroglobulin
- Thyroid-stimulating hormone (TSH)
- Free thyroxine (free T4)
- Total thyroxine (T4)
- Total triiodothyronine (T3)
- Free triiodothyronine (free T3)
- Cholesterol – high density lipoprotein (HDL)
- Cholesterol – low density lipoproteins (LDL)
- Total cholesterol
Treatment
Complex replacement therapy is carried out. Its goal is to raise and maintain normal levels of thyroid hormones. As a rule, treatment begins with incomplete replacement doses, gradually increasing them until the target level is reached. Cardioprotectors are also prescribed in case of disruption of the cardiovascular system, cardiac glycosides, to normalize the functioning of the reproductive function - sex hormones, and other medications based on symptoms.

When prescribing medications, the doctor relies on medications already taken by the patient.
It must be remembered that hypothyroidism is not a disease that can be cured. This is a condition that you can live with, and if you use the appropriate medications, you can live quite comfortably. Hormone therapy is considered the most effective method. The medications are taken daily. The dosage is calculated individually, and regular intake and preventive medical examination helps to lead a full life.
Recommendations from an endocrinologist at the Rassvet clinic for patients with hypothyroidism
When selecting the dose of replacement therapy: strictly follow the recommendations of your endocrinologist regarding the dosage of the drug used, the timing of dose changes and the timing of tests. The accuracy and speed of selection of therapy depends on this.
When the optimal dose is selected (this is indicated by the normalization of TSH levels), know that TSH monitoring must be carried out annually, and if it deviates from the norm, visit an endocrinologist to discuss the optimal dose adjustment.
If before this period (1 year) you suddenly feel changes in your condition, the appearance of symptoms of deficiency or excess of thyroid hormones (hypothyroidism or thyrotoxicosis), contact your endocrinologist earlier for an earlier determination of hormone levels. Such situations sometimes happen.
You are not contraindicated from using iodized salt in the household, but iodine preparations are not a “stimulant” for the thyroid gland that will make it work better or eliminate hypothyroidism.
If you have hypothyroidism and are planning a pregnancy, there are a few very important things to keep in mind
:
- Even before conception, you need to make sure that your TSH level is normal during replacement therapy
- immediately upon pregnancy, the dose of thyroxine is increased by 30–50% (usually prescribed by a doctor)
- an indicator of the sufficiency of the thyroxine dose is the level of TSH and free T4 at 8–12 weeks of pregnancy
- An endocrinologist should monitor your condition throughout your pregnancy.
- The presence of hypothyroidism and its replacement therapy does not eliminate the need to take iodine supplements, which the unborn child needs to produce its own thyroid hormones.
Prevention
No preventive measures have been developed for this pathology. Serious consequences can be avoided with early diagnosis, so do not ignore visits to the endocrinologist. The Ministry of Health of the Russian Federation recommends being examined once every three years until the age of 45, and then once a year. It is necessary to perform an ultrasound of the thyroid gland and take a blood test for the content of thyroid-stimulating hormone and thyroxine.
You can reduce the likelihood of developing hypothyroidism by eating a balanced diet and taking additional iodine-containing medications. The diet should include seafood, especially seaweed and shrimp, fish, buckwheat, and persimmon.
Forms and complications of hypothyroidism
Firstly, hypothyroidism can be primary (due to damage to the thyroid gland itself) and secondary (due to disruption of its regulation by the pituitary gland). But secondary hypothyroidism is incidentally rare, and most patients with hypothyroidism suffer from the primary form of the disease.
Secondly, primary hypothyroidism is divided into manifest (overt) and subclinical.
In the first case, the thyroid gland works so poorly that there is a clear decrease in the level of its hormones in the blood, and this condition is usually accompanied by various symptoms.
In subclinical hypothyroidism, the production of thyroid hormones by the thyroid gland is somewhat impaired, but it still copes with its work. Therefore, the level in the blood of the thyroid gland's own hormones (thyroxine (T4) and triiodothyronine (T3)) is within normal limits, but the level of the hormone TSH (with the help of which the pituitary gland forces the gland to work) is increased (exactly so!). Since a person's general well-being is influenced by T3 and T4, but not by TSH, this condition has no clinical symptoms, hence the name subclinical.
Complications of hypothyroidism are not usually identified, but severe hypothyroidism without treatment can cause irreversible heart damage and, due to the accelerated development of atherosclerosis, lead to heart attack, stroke and other vascular lesions.
Advantages of laboratory diagnostics at JSC SZTsDM
- Prompt testing for thyroid hormones without queues.
- Modern equipment in each laboratory.
- Qualified and friendly staff.
- Quick availability of results, which can be obtained in several ways: in person or by email.
Laboratory terminals have a convenient location and are located within transport accessibility. Present in cities such as St. Petersburg and the Leningrad region, Veliky Novgorod and the Novgorod region, Kaliningrad, Pskov.
Treatment of hypothyroidism in adults and children
Treatment for hypothyroidism is quite simple. However, it is necessary to undergo it by first contacting a specialist.
Just as the thyroid gland normally produces this hormone constantly and daily, with replacement therapy this is done on a constant basis, but the hormone is not produced in the thyroid gland, but is bought at the pharmacy.
But, since the normal intensity of hormone production by the thyroid gland is quite constant, the dose of the drug for replacement therapy is selected quite easily, and treatment is not burdensome for the patient. The drug is taken in a selected dose once a day, on an empty stomach.
The sufficiency of the drug dose is determined by the TSH level, and after selecting the dose, this analysis is performed once a year.
Treatment of hypothyroidism in special situations
It should be taken into account that for subclinical hypothyroidism, treatment is not necessary. At this stage, hypothyroidism may spontaneously disappear after some time, so hormone levels are usually monitored after 3 to 6 months instead of medication.
During pregnancy, hypothyroidism is more dangerous, primarily for the unborn child. Therefore, it requires active detection (at 8–12 weeks of pregnancy, it is recommended to determine the level of free T4 and TSH in the blood).
If detected, hypothyroidism (even subclinical) requires immediate replacement therapy.
Hypothyroidism may be a temporary condition during pregnancy, and the need for ongoing replacement therapy may not always continue after delivery.
Features of the treatment of hypothyroidism at the Rassvet clinic
Hypothyroidism today is not a condition for which any new, revolutionary treatment methods are being developed. However, replacement therapy can also be carried out in different ways.
The peculiarity of the Rassvet clinic is its qualified endocrinologists who make the right decisions in accordance with modern expert recommendations, and do not prescribe unnecessary tests (such as repeated measurements of the level of antibodies to the thyroid gland, which do not affect the choice of treatment).
We also do not prescribe ultrasound of the thyroid gland “just in case” when there is no indication for this study. Such unnecessary tests and instrumental studies often greatly increase the cost of treatment by an endocrinologist.