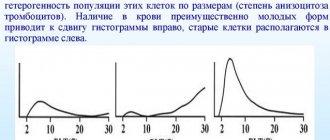
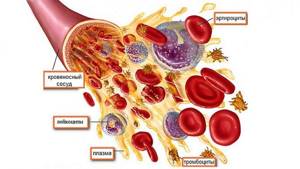
Thrombocrit is the proportion of whole blood volume that is taken up by platelets (blood platelets).
Thrombocrit in the blood (platelet crit, PCT or pct) is an analogue of hematocrit (HCT), however, if the determination of hematocrit is still to some extent, albeit approximately, possible after spontaneous sedimentation of erythrocytes, then with thrombocrit this is not possible.
Outside the bloodstream, platelets, finding themselves on a foreign surface (for example, in a container intended for blood), receive pseudopodia, significantly increase in size (up to 10 times), then stick together and form aggregates.
This feature of platelets makes their examination problematic, as well as their storage for transfusion (it is necessary to maintain a state of rotation), therefore, in the case of thrombocrit, an automatic analyzer turns out to be indispensable.
Thrombocrit is not widely used.
Why do a thrombocrit test?
Why determine thrombocrit:
- Determining the patient's tendency to increased blood clots or bleeding.
- Thrombocrit can be used to assess the risk of possible complications when choosing preventive treatment.
Any physician should consider the platelet count in the study of his patient's blood clotting.
Typically, platelets are not included in the general indicators, and their analysis is carried out only at the request of doctors. This fact is due to the complexities of thrombocrit analysis technology.
The fact is that platelets have a special property: when moving into a “foreign” space, they grow almost tenfold due to the formation of pseudopodia (false legs). After this, the platelets stick together into aggregates - small particles.

This indicator correlates with the MPV indicator - this is the average volume of measured platelets: the higher the MPV indicator, the higher the thrombocrit (PCT), and accordingly, a decrease has the same effect on both indicators.
GRA in blood test: normal values
Only a doctor can correctly decipher the result of the study. This is due to the fact that based on an increase or decrease in the number of any cells, it cannot be guaranteed that there is a pathology. If the development of the disease is suspected, it is necessary to conduct a comprehensive diagnosis. With the help of analysis, it is only possible to suspect the course of the pathological process.
It is important to understand that granulocytes are cells that must be present in the body of every person. Normal indicators directly depend on a person’s age:
- 12 months – 31%;
- up to 10 years – 51-53%;
- 10-16 years – 53-57%;
- 16-21 years old – 59%.
In newly born children, the granulocyte level should be 35%. In adult women and men, the normal rate is 47-72%. Some laboratories use other units of measurement. In adults, the norm of granulocytes is 1.2-6.8 x 109 (in 1 liter of blood).
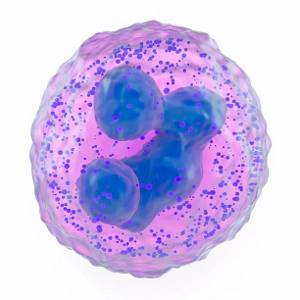
It is important to remember that granulocytes are a group of cells that includes several functional units
When decoding the study, it is necessary to pay attention to their indicators
GRA norm in blood test:
- Basophils. In children under 12 months, their level should be at least 0.4% and no more than 0.9%. In adolescents and adults, the normal rate is 0.6-1%.
- Eosinophils. The level of these cells directly depends on the degree of functioning of the adrenal glands. The norm is 120-350 (in 1 ml of blood). In the morning their level can be increased by 15%, at night (in the first half) - up to 30%.
- Neutrophils. These cells are divided into rod and segmented. The number of the former should not exceed 6%. The norm for segmented neutrophils is 40-70%.
As a rule, if granulocytes are increased or decreased, this means that a pathological process is developing in the body. However, sometimes deviations from the norm can occur for physiological reasons. In women, granulocytes are elevated before menstrual bleeding, in the third trimester of pregnancy and during the delivery process. In both sexes, deviations from the norm to a greater extent may be a consequence of overeating and high-intensity physical activity.
The presence of immature granulocytes in the blood is not a pathology. This is explained by the fact that the life cycle of granular leukocytes is only a few days. In other words, the change to young cells occurs very quickly, the number of the latter ranges from 1 to 5%.
What is the normal thrombocrit level?
In a general blood test, thrombocrit characterizes the content of platelet mass in whole blood, informing about an unacceptable increase or decrease in platelets in the patient.
If the thrombocrit is in the range from 0.15 to 0.4, then this means that it is normal (different sources indicate other normal values: 0.11 - 0.28, 0.12 - 0.38, 0.12 -0.36...).
Science does not distinguish between the norm of this indicator in an adult and an infant (that is, if the thrombocrit indicator is elevated in a child, this is not due solely to his age).

The platelet level indicators decrease or increase proportionally in accordance with the age of the patient, so there is no need to look for any differences in children.
Another thing is the physiological fluctuations of platelets:
- Seasonal and daily fluctuations can change the number of platelets by up to 10% (depression in the spring and at night) - the PCT (thrombocrit) indicator may be below normal or at the lower limit of normal.
- Menstruation can reduce PCT in women by 50%; PCT will also be reduced during pregnancy (this phenomenon is associated with the body’s protection from thrombosis).

- Platelets are also affected by physical activity: thrombocrit may increase (the value of the indicator can increase by 2 times).
Combination of CRP with changes in ESR
Erythrocyte sedimentation rate is one of the oldest laboratory diagnostic methods. Red blood cells from healthy people settle to the bottom of the tube more slowly than red blood cells from pregnant women or people with illnesses. Acceleration of ESR indicates the possibility of a pathological process in the body.
The test is nonspecific and does not indicate any specific disease. ESR increases during inflammation, infections, and malignant processes. Sometimes this indicator remains normal despite the disease. It also happens the other way around - ESR increases in a healthy person.
CRP increases under the same conditions - inflammation, infection, malignant process. Therefore, both of these indicators are usually elevated at the same time. Advantages of determining DRR:
- C-reactive protein rises earlier than ESR - this makes it possible to quickly identify the pathological process;
- PSA is a more sensitive test, showing even minor inflammation;
- CRP levels are not affected by the state of the red blood cells, and ESR in anemia may falsely indicate inflammation.
There are several exception diseases in which reactive protein does not increase in the blood. In this case, only the ESR increases. These diseases are systemic lupus erythematosus and ulcerative colitis. In the diagnosis of these diseases, the combination of high ESR and normal CRP is important.
When does thrombocrit increase?
The reasons for the increase in thrombocrit levels are associated with the reaction to pathology, stimulation of the platelet germ of hematopoiesis.
Most often, PCT values are elevated when:
- Iron deficiency anemia,
- After splenectomy (this is an operation to remove the spleen), an increase in PCT can persist for up to 2 months,
- Blood diseases that are associated with stimulation of the myeloid lineage (essential thrombocythemia, chronic myeloid leukemia, thrombocytopenic purpura, polycythemia),
- Inflammatory diseases of various etiologies (including fungal infections, bacteria),
- Tuberculosis,
- Hyperfunction of the thyroid gland,
- Viral attack (measles, flu, chicken pox in a child),
- Diabetes mellitus
- Laboratory blood tests
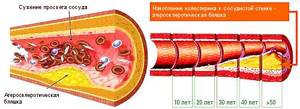
- Atherosclerosis of blood vessels,
- Osteomyelitis,
- Ulcerative colitis,
- Rheumatic attack,
- Fractures of tubular bones,
- In smokers - with nicotine intoxication,
- During a large-scale operation,
- Tissue necrosis (acute pancreatitis).
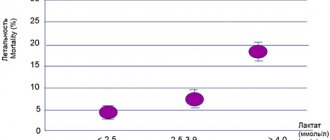
If an increase in this indicator is detected, the patient is at risk of developing:
- Thrombotic stroke (impaired blood supply to the brain).
- Acute coronary thrombosis with a probability of outcome in myocardial infarction.

The possibility of increased thrombosis should be taken into account when:
- Inpatient treatment,
- Prolonged bed rest,
- Upcoming surgery.
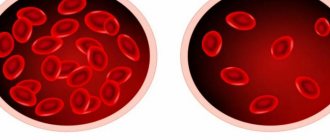
Low platelet count
The reason for low PLT in the analysis may be:
- decreased production of platelets in the bone marrow due to diseases of the blood, thyroid gland, or liver. Also, a decrease in the indicator may be observed due to the effect on the body of a viral infection or intoxication;
- rapid destruction of platelets, which may be associated with the following diseases/conditions: thrombocytopenic purpura, infectious, autoimmune or oncological diseases, blood transfusion or the use of certain drugs (antihistamines, sulfonamides);
- disturbance of the distribution of blood platelets in malaria, tuberculosis or viral hepatitis.

. The following symptoms may indicate that PLT is low:
- severe bleeding that develops after surgical procedures or tooth extraction;
- subcutaneous hemorrhages of various sizes. Initially, they may look like small dots, but later merge into large spots and bruises. They can occur independently or after minor damage to the skin;
- rashes on the skin that have different colors; depending on the time of appearance, they can be brown, blue, red, green or yellow;
- prolonged and very intense bleeding during menstruation;
- nosebleeds that appear spontaneously;
- development of uterine, gastric, hemorrhoidal or pulmonary bleeding;
- enlarged spleen;
- hemorrhages in the retina or brain;
- pain in the joints.
Why does thrombocrit decrease?
If the thrombocrit indicator is low, this indicates:
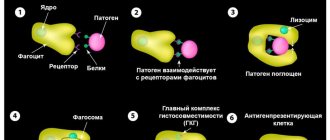
- Increased destruction
- Inhibition of platelet formation by effects on megakaryoblasts (precursor cells).
Most often, low thrombocrit is due to the following reasons:
- myelodysplastic syndrome,
- Anemia (megaloblastic and aplastic),
- Insufficient nutrition of folic acid, when its content is maintained below the required level for a month or more,
- Allergic diseases,
- Lupus erythematosus, as well as other collagenoses,
- Consequences of a course of chemotherapy,
- Blood tumors (hemoblastosis, leukemia),
- Exposure to toxic substances
- Penetrating radiation
- Negative effects of medications (antibiotics, cytostatics, corticosteroids, diuretics),
- Chronic renal and liver failure,
- Viral infections.
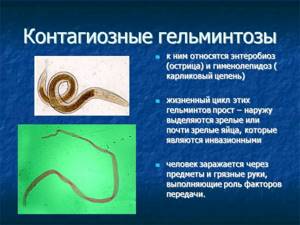
It is found during fetal asphyxia and in low-weight newborns. In older people, a connection between low thrombocrit and exposure to helminthiasis (parasitic infection) has been proven.
A dangerous consequence for the patient’s life can be his tendency to bleed, since any, even minor injuries can cause large blood loss. The most severe manifestation may be hemorrhage in the brain and other organs.
Reasons for lowering the PCT
A drop in the indicator also indicates pathological processes. Which ones exactly?
Megaloblastic anemia
Develops with a lack of vitamins B12, 9. Accompanied by impaired hematopoiesis. It switches to abnormal tracks: instead of mature formed cells, underdeveloped forms move into the channel.
They are unable to perform useful functions. Accordingly, the number of ready platelets is much less. A lower than normal thrombocrit also means that other forms of anemia are present. Read more about megaloblastic here.
Treatment. Impact dose of vitamins. Then you need to find out which disease was the main culprit of the problem. And fight him already.
Allergy
Intense immune response. False. Allergies are always accompanied by the destruction of red blood cells and the platelets themselves, which leads to a decrease in PCT in the analysis.
Attention:
The stronger the reaction, the more dangerous the consequences, including Quincke's edema and asphyxia (suffocation).
Treatment. Antihistamines. In more complex cases, glucocorticoids like Prednisolone or more powerful analogues are used. The question remains with the specialist.
Radiation sickness
Exposure to radiation. In peacetime it is almost impossible to meet her. Mostly patients receiving radiotherapy suffer. Especially if the required dosage is exceeded.
Worm infestations
Regardless of type and location. Treatment is carried out using specialized drugs. Which ones exactly are determined by the parasitologist. After researching the type of culprit organism. The effect occurs almost immediately. The indicators return to normal after a week. Plus or minus.
Malignant tumors
Any localization. Basically, we are talking about the bone marrow itself, as well as the thyroid and pancreas. Less often about the liver. Treatment is strictly surgical. The goal is to remove the abnormal formation completely. Then, if necessary, they resort to radiation and chemotherapy.
Poisoning
Acute intoxication with metal salts, non-metal vapors. Mercury, arsenic, and lead are especially dangerous. They provoke platelet death and clotting disorders. The greater the concentration of the toxic component, the more serious the consequences for the body.
Sometimes a decrease in thrombocrit is the result of natural factors. For example, PCT levels fall during pregnancy and breastfeeding (lactation). Deviations are possible due to hormonal fluctuations. A specialist should study the issue. At a minimum, a hematologist.
Manifestations of changes in thrombocrit levels
It is mandatory for the attending physician to prescribe a blood test for thrombocrit if there is a suspicion of the above diseases.
You should be aware of symptoms that may be associated with a decrease or increase in platelet count.
The patient has:
- General weakness
- Feeling worse
- Fingers and toes turn blue,
- Headache,
- Bruises form on the body,
- Painful sensations in the fingertips,
- Impaired vision
- Nosebleeds,
- Skin itching
- Blood in stool and urine,
- Women experience heavy periods.
Additional examinations if thrombocrit changes
To diagnose the disease, it is important to determine the cause of changes in thrombocrit levels. And a general blood test may not be sufficient for this.
Checked:
- Blood collection
- Bleeding time
- Clotting factors
- Prothrombin index, fibrinogen,
- Liver tests
- Protein composition,
- blood sugar
- Residual nitrogen, creatinine,
- Iron,
- Analysis of urine,
- If necessary, hormonal composition can be checked.
The doctor prescribes to the patient:
- Hardware studies using radiography and ultrasound.
- To check the patency of blood vessels, Doppler examination is indicated.
- If certain symptoms are detected, magnetic resonance imaging of the brain is prescribed.
- If there is a suspicion of a blood disease, a bone marrow puncture is prescribed.
- The correctness of the hematopoiesis process is checked.
Prevention in case of changes in thrombocrit values
If the thrombocrit is elevated, the doctor prescribes:
- Antiplatelet agents.
- Anticoagulants.
Their intake is necessary to reduce the risk of vascular thrombosis.
The duration of the course and dosage are determined by the attending physician. You cannot increase the dose or stop taking it on your own.
You should consult your doctor about the advisability of taking hormonal birth control and the need for diuretics.
The patient is recommended:
- Stop smoking.
- Avoid alcoholic beverages.
- Drink clean filtered water in an amount of at least two liters/day.
- The daily diet should include:
- Onion,
- Garlic,
- fish,
- Lemons,
- Tomatoes,
- Vegetable linseed oil,
- Fruits and berries,
- Meat,
- Beef
- Buckwheat,
- Liver,
- Dairy products,
- Seafood.
Not recommended:
- Bananas,
- Lentil porridge,
- Walnuts,
- Pomegranates and mangoes,
- Drinks with chokeberry.
If your thrombocrit level decreases, you should include in your diet:
- Vegetables and fruits,
- Be sure to eat fish or meat dishes every day,
- Fresh juices with viburnum, cranberries, sea buckthorn.
It is not recommended to consume products containing acetic acid and preservatives. Homemade preparations are also harmful to the body. You will have to exclude all kinds of allergens (citrus fruits, honey, eggs, chocolate).
To maintain normal thrombocrit, the patient is recommended to:
- Reduce the likelihood of minor injuries.
- Limit physical activity.
- Organize sufficient sleep and rest.
- Refuse vaccinations.
The specific need for a course of treatment when thrombocrit changes is determined by the doctor. If the listed symptoms are detected, you should not self-medicate. Common folk remedies are more likely to harm than help.
Having spent time selecting the “best” treatment method, the patient loses the opportunity to use the minimum doses of necessary drugs, which worsens the prognosis.