Pregnancy is a wonderful and quite exciting period. The expectant mother is worried about the baby’s health, because she cannot fully control what is happening, and the intervals between doctor’s examinations are long.
A woman experiences especially many worries during the period until the baby begins to actively push. At this time, a special device – a fetal doppler – will help you listen to the rhythm of the baby’s heartbeat.
Previously, such equipment was used exclusively in medical institutions for routine examinations of pregnant women.
Now there are portable dopplers designed for home use. But is there a need for every pregnant woman to purchase such a device and use it regularly? Does fetal doppler harm the baby? Let's try to understand these issues in more detail.
Monitoring the progress of pregnancy using Doppler
Doppler ultrasound helps monitor the level of blood flow in the uterus, umbilical cord and fetal vascular system.
Monitoring blood flow allows you to identify the presence of a possible threat to the development of the fetus and take timely measures.
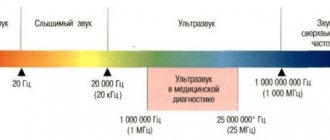
The specifics of the study are based on the Doppler effect, when ultrasound is reflected from moving elements and changes the frequency of oscillatory processes. The sounds sent by the device return at a different frequency, which appears as an image on the screen.
How is Doppler testing performed during pregnancy?
In general, as a process, this study for a pregnant woman is practically no different from a regular ultrasound; the doctor’s actions and sensations are the same. The procedure is carried out using a special ultrasound sensor of the device, which is equipped with appropriate software.
The pregnant woman lies on her back on the couch, and the doctor applies a small amount of a special gel to her stomach to improve contact between the sensor and the skin. After this, the necessary anatomical structures of the fetus are examined.
Doppler ultrasound does not require any special preparation and can be performed at any time.
In what cases is Doppler ultrasound prescribed for pregnant women?
The doctor insists on conducting this study in the following situations:
- Rhesus conflict between mother and fetus.
- The woman has a history of frozen pregnancy.
- If you suspect abnormal development of the placenta.
- Multiple pregnancy.
- Polyhydramnios and oligohydramnios are diagnosed.
- Sonography showed the presence of umbilical cord loops dangerously close to the fetal neck.
- To confirm or exclude the diagnosis of “heart malformation” and “brain malformation”.
- An external examination showed that the size of the fetus was significantly smaller than normal at a certain period.
- A pregnant woman suffers from diabetes, gestosis or autoimmune diseases.
- Kidney diseases.
- Hypertension.
- Sonography showed pathologies in the development of the umbilical cord.
- There is a history of spontaneous miscarriage.
- Cases of abdominal injuries during pregnancy.
- The CTG results are far from positive.
When should you undergo a Doppler test?
As a rule, Doppler measurements are performed only after the placenta is fully formed, that is, after the 18th week of pregnancy. According to Appendix No. 5 to the order of the Ministry of Health of Russia dated December 28, 2000 No. 457, Dopplerography of utero-fetoplacental blood flow is carried out at 20-24 weeks of pregnancy. A later order regulates ultrasound examination at gestational ages of 18-22 weeks, 27-32 weeks and 35-37 weeks. During these periods, blood flow readings taken by Doppler become reliable.
What do the data obtained mean?
In conclusion, the following indicators are indicated:
- The pulsatility index is determined by dividing the difference between the maximum and minimum velocity indicators by the average blood velocity for 1 complete cardiac cycle.
- The ratio of systole and diastole can be determined by dividing the highest speed of blood movement through the vessel at the moment of contraction of the heart (systole) by the final speed of blood movement through the vessel at the moment of relaxation of the heart (diastole).
- The resistance index is found by dividing the difference between the highest and lowest speeds of blood movement through the vessels by the maximum speed value.
Based on these three parameters, the degree of blood movement is assessed. Each vessel has its own digital norm, which depends on the stage of pregnancy.
During a normal pregnancy, the test results do not change. With the development of feto-placental insufficiency in the artery, vascular resistance increases, which leads to an increase in the resistance index and systolic-diastolic ratio.
Standard Doppler indicators during pregnancy
Below, for general information, are presented the norms of the main indicators that are used when forming a medical opinion. It is important to know that deviations from standards do not always indicate the presence of pathologies. The final diagnosis is made by the doctor based on the gestational age, the possible range of fluctuations in indicators and other features of Doppler measurements.
Standard indicators of systole-diastolic ratio (SDR)
| Gestation period by week | SDO in the uterine arteries | SDO in the umbilical cord arteries | SDO in the middle cerebral artery of the fetus | SDO of the fetal aorta |
| 20-24 | up to 2.5 | up to 4.4 | from 2.9 | up to 8.4 |
| 25-27 | up to 2.4 | up to 3.8 | from 2.7 | up to 8.2 |
| 28-33 | up to 2.3 | up to 3.2 | from 2.4 | up to 7.9 |
| 34-41 | up to 2.3 | up to 2.9 | from 2.2 | up to 7.4 |
Average resistance index (RI) indicators
| Gestation period by week | IR of the uterine arteries | IR of the umbilical cord arteries | Fetal aortic IR |
| 20 | 0,52 | 0,74 | 0,79 |
| 21 | 0,51 | 0,73 | |
| 22 | 0,5 | 0,72 | |
| 23 | 0,5 | 0,71 | |
| 24 | 0,5 | 0,7 | |
| 25 | 0,49 | 0,69 | |
| 26 | 0,49 | 0,68 | |
| 27 | 0,48 | 0,67 | |
| 28 | 0,48 | 0,66 | |
| 29 | 0,47 | 0,65 | |
| 30 | 0,46 | 0,64 | |
| 31 | 0,46 | 0,63 | |
| 32 | 0,45 | 0,62 | |
| 33 | 0,45 | 0,61 | |
| 34 | 0,45 | 0,6 | |
| 35 | 0,45 | 0,59 | 0,78 |
| 36 | 0,44 | 0,58 | |
| 37 | 0,44 | 0,57 | |
| 38 | 0,44 | 0,56 | |
| 39 | 0,43 | 0,55 | |
| 40 | 0,43 | 0,54 | |
| 41 | 0,43 | 0,53 |
Average pulsation index (PI) indicators
| Gestation period by week | PI of the uterine arteries | PI of the umbilical cord arteries | PI in the fetal middle cerebral artery | PI of the aorta |
| 20 | 1,54 | 1,45 | 1,83 | 1,79 |
| 21 | 1,47 | 1,35 | 1,87 | 1,79 |
| 22 | 1,41 | 1,35 | 1,91 | 1,79 |
| 23 | 1,35 | 1,25 | 1,93 | 1,8 |
| 24 | 1,3 | 1,12 | 1,96 | 1,8 |
| 25 | 1,25 | 1,15 | 1,97 | 1,81 |
| 26 | 1,2 | 1,01 | 1,98 | 1,81 |
| 27 | 1,16 | 1,01 | 1,99 | 1,82 |
| 28 | 1,12 | 1,05 | 1,99 | 1,83 |
| 29 | 1,08 | 1,03 | 1,99 | 1,82 |
| 30 | 1,05 | 0,95 | 1,98 | 1,81 |
| 31 | 1,02 | 0,85 | 1,97 | 1,81 |
| 32 | 0,99 | 0,84 | 1,95 | 1,8 |
| 33 | 0,97 | 0,84 | 1,93 | 1,8 |
| 34 | 0,95 | 0,83 | 1,9 | 1,79 |
| 35 | 0,94 | 0,81 | 1,86 | 1,79 |
| 36 | 0,92 | 0,81 | 1,82 | 1,79 |
| 37 | 0,92 | 0,81 | 1,78 | 1,92 |
| 38 | 0,91 | 0,74 | 1,73 | 1,93 |
| 39 | 0,91 | 0,74 | 1,67 | 1,94 |
| 40 | 0,91 | 0,74 | 1,61 | 1,94 |
| 41 | 0,92 | 0,74 | 1,55 | 1,95 |
Pathological changes determined using the Doppler method
- Gestosis of pregnancy, in which the main parameters are higher than normal: first, the resistance index and the systole-diastolic ratio in the uterine arteries increase, after which the indicators of the umbilical cord arteries change.
- The main parameters increase in the fetal aorta and umbilical cord artery in case of diabetes mellitus in a woman, Rh conflict between mother and fetus, and pregnancy being exceeded.
- In case of multiple pregnancy, when one of the fetuses differs from the other in size and body weight, the study will reveal an increase in the resistance index and systolic-diastolic ratio in the umbilical cord artery in the less developed fetus. If, according to the results of the study, one fetus is clearly developing worse, but the main indicators remain normal, then we are talking about transfusion syndrome.
The Doppler method not only detects the presence of pathology, but also determines the degree of its severity. If the changes are serious, then treatment may be prescribed or labor may be induced.
Is fetal doppler harmful or not?
In the age of development of medicine and product quality, we still wonder whether what we live with, what we eat and what we use is safe. This question becomes especially acute when we see two cherished lines on a pregnancy test.

From time to time we receive questions from customers: is fetal doppler safe? Is fetal doppler harmful? Is fetal doppler harmful for a baby? Is it harmful to use a fetal doppler? Is taking a fetal doppler on a daily basis harmful to the fetus? Is fetal doppler harmful? Are fetal dopplers harmful during pregnancy? Is home Doppler harmful? Is fetal doppler harmful to the fetus? Are home dopplers harmful to children? Is fetal doppler harmful? Is Doppler harmful for a child?
Therefore, let's look together - is using a fetal doppler harmful during pregnancy?
- Let's start with the fact that companies producing fetal dopplers are controlled by the American federal control system FDA. Therefore, Dopplers are manufactured taking into account European Union safety standards and restrictions on the safe percentage of ultrasound consumption.
- There is a significant difference between a standard ultrasound performed by a doctor and the use of fetal doppler.
During your appointment at the clinic, you will learn not only the fetal heart rate, but also many other unfamiliar terms. All of them show a complete picture of the course of pregnancy. These are the pulsatility index, resistance index, systolic-diastolic ratio and maximum systolic blood flow velocity. The umbilical, uterine, midcerebral aorta of the fetus, and venous sinus are also examined. This set of procedures is carried out only a few times during pregnancy, which can cause slight discomfort in the baby - but in modern medicine this is a necessary examination for the favorable development of the fetus.
In turn, when using a fetal portable doppler, you only determine the heart rate, which is not felt by the baby himself.
- The impact of ultrasound from a doctor lasts on average 20 minutes, fetal doppler is used for only 1-2 minutes.
- The power of a fetal doppler is significantly less than that of ultrasound devices and does not reach all possible risks.
- Thanks to the periodic use of fetal doppler, there is no unnecessary stress for the expectant mother, which has a positive effect on the harmonious development of the baby’s physical and mental health.
- The benefits of timely detection of abnormalities in the fetal heartbeat far outweigh any possible risks from using a portable Doppler.
- To date, no side effects have been identified from the use of fetal doppler.
Attention! Using a fetal doppler will not replace a full consultation with your doctor. Don't miss routine examinations and stay healthy!
Rules of application
Fetal Doppler can be used at home starting from the 12th week of pregnancy. More sensitive devices that can image the fetal heart in the early stages are expensive and are classified as specialized medical equipment.
Research technique:
- the woman lies on her back, on a flat horizontal surface, exposing her lower abdomen;
- A gel must be applied to the area of skin that will come into contact with the sensor, providing a clear signal;
- the sensor should be moved slowly, without sudden movements;
- in the first trimester, the external probe of the device should be placed directly above the pubis, since the fundus of the uterus is located quite low;
- in the second trimester - just below the navel, sometimes with a shift to the left or right;
- in the third trimester - above or below the navel, depending on the position of the child.
The duration of the study is 3-7 minutes. You should not repeat the procedure every day, much less several times a day.
Purchasing a fetal doppler and monitoring your baby's heartbeat at home is not a reason not to visit a medical specialist.
What pathology can be diagnosed using CTG?
What exactly can be said from the data obtained? A final diagnosis cannot be made based solely on this method. Because any pathology and pathological rhythm can be a temporary response of the fetus’s body to an external stimulus or an administered drug, or even the mother’s mood. Therefore, remember, based only on CTG, it will be wrong to make a diagnosis. This method is simple and allows you to quickly and inexpensively suspect any condition in the unborn baby.
The following pathologies can be suspected using cardiotocography:
*Twisting or pressing the umbilical cord. These conditions can lead to disruptions in the supply of oxygen from the mother's body. At first, the fetus can compensate for the lack of nutrients, but if blood flow in the umbilical cord is not restored, this can lead to a serious condition;
* Rhythm disturbances in a child. Irrhythmic heartbeat can occur in the presence of cardiac developmental anomalies, even minor ones, such as accessory chords;
* With fetal hypoxia. The fetus may compensate for a long time and not show a lack of nutrients and there will be slight signs of deviation on CTG;
* During childbirth, this method allows you to quickly assess the condition of the fetus and all the changes that occur;
* For maternal diseases that may affect the condition of the fetus. In such cases, registration is made every day if the woman is in the hospital.
After the recording has been made and the doctor has suspected abnormalities in the CTG during pregnancy, if possible, the woman should undergo an ultrasound and Doppler ultrasound. In some cases, it is possible to carry out treatment and record a CTG again.
If the diagnosis is confirmed by ultrasound, then treatment is performed. CTG is recorded every day, and if necessary, 2 times a day.
Types of devices
All CTG devices (fetal monitors, cardiotocographs) can be divided into two large groups.
The first type includes devices that record only the heartbeat on tape and do not decipher its result. In this case, the resulting tape is analyzed by a doctor. The analysis depends on what period of pregnancy it was recorded. Decoding during childbirth is different from deciphering during pregnancy. During pregnancy, as a rule, the Fisher assessment is performed.
The second group of CTG devices records and deciphers this curve. But in order to understand the answer, you need to be well versed in all indicators.
Is it necessary to use the device?
It’s worth saying right away that there is no direct need to buy a fetal doppler and use it for home monitoring of pregnancy. From the moment a woman is registered as pregnant, her condition is monitored by specialists. There are developed plans for visiting a doctor and conducting additional examinations, in particular, ultrasound. If pregnancy proceeds without deviations, then three ultrasound examinations are sufficient, during which a Doppler assessment of blood flow in the mother-placenta-fetus system is determined.

In the early stages, transvaginal ultrasound is used. During this examination, the fetal heartbeat can be heard as early as 3 weeks. Another diagnostic method at the initial stage of pregnancy is transabdominal ultrasound, but this procedure is prescribed no earlier than 5 weeks. Starting at 18 weeks, the doctor listens to the baby's heartbeat using an obstetric stethoscope.
But some women experience strong worries about their baby in the interval between doctor visits. The feeling of discomfort increases if there have been previous pregnancies with an unfavorable outcome. In this case, you can purchase a fetal doppler and use it to monitor the fetal heartbeat. Firstly, the expectant mother will simply be pleased to hear the little heart beating, and secondly, it will relieve her of stress.
Description of Doppler
Content:
- Description of Doppler
- Is it necessary to use the device?
- Rules of application
- When is the best time to conduct research?
- Should we panic?
Fetal Doppler is a special device whose main function is to process and transmit ultrasound waves received from the internal organs being examined. The frequency of the ultrasonic signal ranges from 2.0 to 3.0 MHz. As the frequency increases, the sensitivity of the device decreases. In early pregnancy, when the fetal heartbeat cannot be heard without the use of special equipment, fetal doppler can also be used.
The device transmits all received data on a digital display. Additionally, it is possible to listen to the baby's heartbeat using a portable speaker or headphones for this purpose. Most models of fetal dopplers are additionally equipped with a USB cable, with which you can connect the device to a PC and save a recording of the study.
The power source is a battery or a set of batteries. Additionally, the kit may include a special gel required for the research procedure (such gels are sold in pharmacies and stores selling medical equipment).