Scientific editor: M. Merkusheva, PSPbSMU named after. acad. Pavlova, medical practice. August, 2021
Synonyms: antibodies to rTSH, antibodies to TSH receptors, TSH receptor autoantibodies, TRAb.
Antibodies to thyroid-stimulating hormone receptors (ABs to rTSH, stimulating and blocking) are a group of autoantibodies that interact directly with TSH receptors on the thyroid gland. Thyroid-stimulating hormone (TSH), which regulates the functioning of the entire endocrine system, is produced by the pituitary gland. The higher the TSH concentration, the more active the thyroid gland produces thyroid hormones (T3 and T4), which are responsible for energy and oxygen metabolism in tissues, nervous processes, etc.
When receptors and TSH bind, the biological effect of the latter is enhanced, which leads to activation of thyroid cells. Stimulating antibodies interact with TSH receptors in a similar way.
As a result, the thyroid gland produces twice as much thyroid hormones (hyperfunction), and thyrotoxicosis develops - intoxication of the body with its own hormones. The progression of the pathological process causes damage to the gland (increase in size, change in structure, inflammation, etc.).
One of the most common conditions characterized by increased concentrations of antibodies to rTSH is diffuse toxic goiter or Graves' disease. This is an autoimmune disease that is accompanied by changes in the size of the thyroid gland and its dysfunction.
Blocking antibodies suppress thyroid function. In this case, TSH is deactivated, which leads to gland atrophy and hypothyroidism (deficiency of iodinated hormones).
Abs to rTSH, for the most part, belong to IgG immunoglobulins, can penetrate the placental barrier, and therefore are also a marker of transient thyroid dysfunction in newborns.
It is known that patients with thyrotoxicosis are more susceptible to osteoporosis. However, a high titer of antibodies to rTSH in pre- and postmenopausal women with hyperthyroidism and ophthalmopathy can act as a protective factor against bone destruction.
Indications for the test
The endocrinologist refers for analysis of antibodies to rTSH in the following cases:
- Diagnosis of diffuse goiter, as well as before prescribing or canceling hormonal maintenance therapy.
- Diagnosis of hyperthyroidism (overproduction of endocrine hormones), its differential diagnosis with other diseases of the thyroid gland (autonomous ectopia, in which congenital anomalies of the gland are noted).
- Determination of antibody concentrations in patients with thyrotoxicosis (suspected autoimmune disorders).
- Monitoring of patients with Graves' disease (monitoring the effectiveness of therapy and predicting relapses).
- To predict the development of transient thyroid dysfunction in newborns.
- When examining pregnant women with signs of hypothyroidism.
Prescribing a test for antibodies to TSH receptors is advisable when identifying symptoms:
- hyperthyroidism: feelings of interruptions in heart function;
- weight loss despite increased appetite;
- irritability, anxiety, tremor;
- weight gain, despite decreased appetite;
With successful treatment, the concentration of antibodies to rTSH decreases. The complete disappearance of antibodies indicates the onset of remission.
Analysis for antibodies to rTSH is a mandatory test in the 3rd trimester of pregnancy if the expectant mother has a history of thyroid pathologies.
Antibodies to thyroid-stimulating hormone receptors
Detection of autoantibodies to the thyroid-stimulating hormone receptor in blood serum, used to diagnose Graves' disease (Graves' disease), autoimmune thyroiditis, as well as transient dysfunction of the thyroid gland in newborns.
Research method
Chemiluminescent immunoassay.
Units
IU/L (international unit per liter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
Do not smoke for 30 minutes before donating blood.
General information about the study
TSH receptor antibodies are a heterogeneous group of autoantibodies that interact with the thyroid stimulating hormone (TSH) receptors of the thyroid gland. Based on their effect on thyroid function, anti-pTTH is divided into stimulating and blocking antibodies.
Stimulating anti-pTTHs greatly enhance thyroid function, leading to diffuse goiter and hyperthyroidism. Anti-pTTH blockers interfere with the action of TSH and lead to thyroid atrophy and hypothyroidism. Anti-rTSH are predominantly immunoglobulins of the IgG class and penetrate the placental barrier. Both variants can be detected simultaneously in the blood of the same patient. They are the direct cause of Graves' disease and autoimmune thyroiditis, as well as transient thyroid dysfunction in newborns. A test for antibodies to the TSH receptor is a diagnostic test that detects both stimulating and blocking antibodies in the blood.
What is the research used for?
- For differential diagnosis of hyper- and hypothyroidism syndrome.
- To monitor the treatment of relapse of Graves' disease and make its prognosis.
- To predict the development of transient thyroid dysfunction in newborns.
What do the results mean?
Reference values
| Result | |
| negative | |
| > 1.75 IU/l | positive |
Reasons for the positive result:
- Graves' disease (Graves's disease);
- autoimmune thyroiditis.
Reasons for negative results:
- absence of autoimmune thyroid diseases;
- disease control during treatment;
- incorrect blood collection for testing.
What can influence the result?
- The concentration of anti-rTSH decreases due to the use of thyrotoxic drugs.
Important Notes
- The result of the study should be interpreted taking into account additional clinical, laboratory and instrumental data.
- A negative result does not completely exclude the disease.
AT standards for rTSH in various laboratories
*It should be immediately noted that the difference in reference values is due to insufficient standardization and the use of different methods in laboratories.
The following reference values have been established for both women and men:
- Negative: 1.0 U/l
- Doubtful: 1.1-1.5 U/l
- Positive: 1.5 U/l
Reference values in the Invitro laboratory:
- less than 1.0 – negative;
- greater than or equal to 1.0 – positive
Standards in the Helix laboratory
- less than 1.75 IU/l - negative
- more than 1.75 IU/l - positive
Note:
the result of the study is assessed in conjunction with additional clinical, laboratory and instrumental tests. If a negative answer is received, the presence of the disease cannot be completely ruled out.
What can affect the result
The following factors may distort the results of the study:
- treatment with thyrotoxic drugs;
- non-compliance with the rules of preparation for analysis by the patient or doctor;
- taking iodine supplements, synthetic hormones, steroids, etc.;
- recent surgery or trauma to the thyroid gland.
Important! The interpretation of the results is always carried out comprehensively. It is impossible to make an accurate diagnosis based on only one analysis.
Antibodies to rTSH in pregnant women
Often, in expectant mothers, the level of thyroid-stimulating hormone is slightly reduced. To be on the safe side, the gynecologist may prescribe an antibody test. Since pregnant women are prohibited from undergoing thyroid scintigraphy (the main method for detecting diffuse goiter), an anti-rTSH antibody test may be an alternative.
If the antibody concentration remains normal with a low TSH, then Graves' disease and other autoimmune lesions can be excluded.
Additionally, an analysis can be prescribed in the last trimester of pregnancy if the woman has a history of damage to the thyroid gland (trauma, surgery, disease, etc.), surgical treatment of goiter, or radioactive iodine therapy. The test is also given to expectant mothers if they are receiving thyrotoxic drugs.
Note: Newborns born to mothers with Graves' disease have an increased chance of developing transient thyrotoxicosis syndrome. Antibodies are passed from the mother to the baby through the placenta. Normally, they are independently eliminated from the body, their level gradually decreases to reference values. But in 1% of cases, the child develops postpartum thyroiditis or neonatal hyperthyroidism.
A test for antibodies to TSH receptors can be prescribed and interpreted by an endocrinologist, immunologist, rheumatologist or gynecologist.
Materials and methods
Materials
- Among newly diagnosed Graves' disease patients treated at Seoul National University Hospital between March and December 2001, 93 premenopausal women (mean age 33 ± 9 years) were selected.
- Graves' disease was diagnosed based on symptoms and signs of hyperthyroidism: elevated levels of thyroxine (T4) and/or triiodothyronine (T3),
- decreased TSH level,
- increased uptake (>4.5%) of technetium-99m during scintiography.
- had no fractures
Classification of groups of “stimulating ATs” and “blocking ATs”
- All 93 patients were divided into 2 groups, according to their AT-rTSH type. Patients who had only AT-rTSH with thyroid-stimulating activity formed the group of “stimulating ATs” (n = 83).
- Patients whose clinical picture suggested the presence of both rTSH-ATs with stimulating activity and ATs with blocking activity were called the “blocking ATs” group (n = 10). These 10 patients from the blocking antibody group had spontaneous (idiopathic) hypothyroidism with persistent immunoglobulins inhibiting TSH binding (TBII) for 1-2 years after remission (
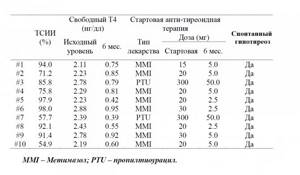
.
- 11 patients from the “stimulating AT” group, who had free T4 and TBII values corresponding to 10 patients from the “blocking AT” group, were further classified as the corresponding control group (n = 11).
Analysis of cAMP in normal thyroid epithelial cells
- To test the biological effects of blocking Abs, normal H. tori thyroid epithelial cells purchased from the Korean Cell Bank (Seoul, South Korea) and grown in RPMI medium containing 10% fetal bovine serum were
- were treated with whole serum from each patient from the “blocking Ab” group.
- recombinant bovine TSH (10 mU/ml, Sigma-Aldrich, St. Louis, MO, USA),
- TSHr-blocking human monoclonal antibodies K1-70 (100 ng/mL, RSR Ltd.).
Biochemistry
- Serum samples were obtained in the morning on an empty stomach and were immediately processed and frozen at −70°C until analysis was completed.
- Serum TSH levels were measured using an immunoradiometric assay.
- Free T4 and T3 levels were measured using radioimmunoassay.
- AT-rTSH levels were measured using the first generation TSII assay.
- Serum concentrations of calcium, phosphorus, total protein, and albumin were measured on a Hitachi 7600 chemistry autoanalyzer. Corrected calcium levels were calculated using the following formula: corrected Ca = 0.8 × (4.1—patient's albumin) + patient's Ca.
- Serum parathyroid hormone (PTH) levels were measured using a radioimmunometric assay and serum 25-hydroxy-cholecalciferol (25-OHD3) levels using ultrafast tandem liquid chromatography-mass spectrometry.
- Serum bone-specific alkaline phosphatase (CS-ALP) levels were measured by enzyme immunoassay (reference interval for premenopausal women: 11.6–29.6 U/L).
- Serum osteocalcin levels were measured using an immunoradiometric assay.
- Serum type I collagen C-terminal telopeptide (C-telopeptide) levels were measured using an electrochemiluminescent immunoassay (reference interval for premenopausal women: <0.573 ng/mL, Roche, Indianapolis, IN, USA).
Statistical analysis
Data are presented as means ± standard deviation (SD), and differences between groups were assessed using a student's t test. The partial correlation coefficient was calculated using SPSS 20.0 (“Statistical Package for the Social Sciences”). A P value < 0.05 was considered statistically significant.