Hormonal disorders of the thyroid gland are a sign of the development of serious pathologies in the body. According to statistics, such disruptions in the endocrine system occupy second place in the world after diabetes mellitus. Therefore, it is important to regularly visit an endocrinologist to monitor hormone levels and timely diagnosis of thyroid pathologies.
COST OF SOME ENDOCRINOLOGIST SERVICES IN OUR CLINIC IN ST. PETERSBURG
| Price for a detailed examination of thyroid hormones (8 tests) | 5020 rub. |
| Endocrinologist appointment | 1000 rub. |
| Ultrasound of the thyroid gland | 1000 rub. |
| Call free: 8-800-707-1560 *The clinic is licensed to provide these services | |
What hormones does the thyroid gland produce and why are they needed?
The content of the article
The thyroid gland is one of the most important organs of the endocrine system. This butterfly-shaped gland is located on the front of the neck, just below Adam's apple. It has two petals connected by a thin isthmus and, in response to the pituitary thyroid-stimulating hormone, produce their own hormones that perform the regulatory and coordinating function of human organs.
Thyroid hormones, called iodine-containing peptides, are triiodothyronine (T3) and thyroxine (T4). These hormones play an important role in human life and have a decisive influence on metabolism (metabolism), growth and development of the body of any person.
T3 and T4 are produced by the follicular cells of the thyroid gland in response to the pituitary hormone TSH. Their production requires two main components - iodine and the amino acid tyrosine, which usually enter the body with food and water, so it is important that they are present in sufficient quantities in the diet.
When synthesizing hormones, the thyroid cell (thyrocyte) produces a glycoprotein substance (thyroglobulin), which accumulates in the cavity of the thyroid follicle and serves as a kind of “reserve” for the rapid synthesis of hormones.
In addition to the hormones T3 and T4, the thyroid gland produces, along with C cells, another hormone known as calcitonin, which is involved in the regulation of calcium and phosphorus metabolism and bone development.
- The production of thyroid hormones is regulated by a mechanism that reduces the rate of production when circulating hormone concentrations are high, and increases it when the concentration of hormones in the blood decreases.
- Regulation is carried out by the hypothalamic-pituitary system through a negative feedback mechanism.
The pituitary gland synthesizes thyroid-stimulating hormone, which enhances the synthesis and release of T3 and T4 into the blood. The secretion of TSH, in turn, is regulated by the function of the hypothalamus, which produces thyrotropin-releasing hormone. In this way, a hormonal balance is maintained that is adequate to the body's needs.
Laboratory diagnosis of thyroid function
One of the key methods for diagnosing the functional state of the gland is a hormonal blood test.
The role of laboratory diagnostics cannot be overestimated, because the choice of treatment regimen and, ultimately, its success depend on the test results.
Standard list of hormonal studies:
- Thyroid Stimulating Hormone;
- Free Thyroxine;
- Free Triiodthyronine;
- Autoantibodies: Antibodies to thyroglobulin (Thyroglobulin autoantibodies);
- Antibodies to thyroid peroxidase (Thyroid peroxidase autoantibodies).
Let us briefly explain why these tests are prescribed:
TSH - by the content of this thyroid-stimulating hormone in the blood, one can judge the “functionality” of the thyroid gland. If the level of TSH in the blood is elevated, it means that the gland does not produce enough of its own hormones, and the pituitary gland tries to compensate for this by increasing the production of thyrotropin. And vice versa: if the TSH level is below normal, the thyroid gland produces excess hormones.
T3 - high levels of the hormone triiodothyronine in the blood can indicate a serious disease - hyperthyroidism. The earlier this disease is detected, the lower the risk of complications.
T4 - the level of the hormone thyroxine in the blood gives a clear picture when diagnosing hyperthyroidism and hypothyroidism.
AT-TPO - antibodies to thyroid peroxidase (an enzyme of thyroid cells). Through this analysis, it is possible to identify an autoimmune thyroid disease (a pathology in which the body perceives its own cells as hostile and fights against them).
AT-TG - antibodies to thyroglobulin (iodinated protein from which thyroid hormones (T4 and T3) are formed. This test is also extremely useful for identifying a number of autoimmune diseases of the thyroid gland (autoimmune thyroiditis, diffuse toxic goiter, Hashimoto's disease).
Any deviation of hormonal levels from the norm identified in the listed studies will be an absolute indication for the appointment of additional examinations, in particular an ultrasound examination of the thyroid gland.
To prescribe drug therapy or (if necessary) decide on the advisability of surgical treatment, a more detailed diagnosis of thyroid function is necessary.
In our clinic, for the convenience of patients (as well as saving their time and money), special screening programs have been developed for this profile:
The importance of thyroid hormones
Thyroid hormones play a fundamental role in the proper functioning of metabolism, growth and development:
- Metabolism.
Thyroid hormones increase both basal metabolism and metabolic activity of all tissues. Basal metabolism refers to the energy expenditure of a person at rest and wakefulness. For example, a person with elevated thyroid hormone levels will have increased energy intake. Thyroid hormones also affect glucose and lipid metabolism, increase protein synthesis, increase cardiac contractility, and increase heart rate. Thus, with hyperthyroidism, one of the main symptoms is tachycardia. - Height
. Thyroid hormones are essential for normal human growth, as evidenced by slow growth in cases of hormone deficiency. - Development.
A classic experiment in endocrinology was the demonstration that tadpoles deprived of thyroid hormones could not be transformed into frogs. This reinforces the fact that normal hormone levels play a fundamental role in fetal and newborn brain development.
How to find out the status of the thyroid gland?
There are two most informative and safe ways to study the condition of the thyroid gland in detail - an ultrasound examination and a blood test for hormones. Moreover, if ultrasound helps determine changes in the size of the gland, the presence of nodes or neoplasms in it, then a blood test provides most of the information about the cause of the disease and the nature of the dysfunction of the gland. Laboratory diagnostics allows you to determine the method of treating the disease and monitor the effectiveness of treatment (including gland cancer or its inflammation).
A blood test for thyroid hormones will also be useful for women when planning pregnancy for early detection of iodine deficiency and its elimination. In this way, the expectant mother can protect the child from serious complications caused by iodine deficiency during pregnancy.
A blood test for thyroid hormones and other indicators of its functioning help to detect the disease at an early stage, which is of particular importance if there are nodules in the thyroid gland or if there is a hereditary predisposition to its diseases.
Have you decided to check your thyroid gland? Don't put off this important decision until tomorrow. Check if there is a Lab4U online laboratory near you and order a blood test for hormones! Today you order an analysis with a 50% discount, take it at any convenient time and place and get the result the very next day!
Additional influence of hormones
Thyroid hormones have a profound effect on almost the entire body:
central nervous system
. A sufficient level of thyroid hormones in the last phase of development of the fetus and newborn is an important condition for the normal development of the central nervous system. Hormonal imbalance of the thyroid gland during this delicate period leads to cretinism or irreversible mental retardation. Early diagnosis and adequate replacement therapy in the third week of life can prevent serious and undeniable consequences.
In an adult, both a decrease and an increase in the concentration of thyroid hormones lead to changes in mental state. A decrease in thyroid hormone levels causes a person to feel lethargic, while an excess of hormones provokes anxiety and nervousness.
Sympathetic nervous system
. Thyroid hormones increase the number of specific receptors with which catecholamines (chemicals such as adrenaline that transmit nerve impulses at the level of sympathetic nerve endings) interact. It occurs mainly in the heart, skeletal muscle, adipose tissue and lymphocytes.
The cardiovascular system
. Thyroid hormones increase myocardial contractility, heart rate, and venous return to the heart, significantly improving cardiac function. They also promote vasodilation, which leads to increased blood flow to many organs.
Respiratory system
. Thyroid hormones influence the response of nerve centers to respiratory stimuli. In practice, they perform an irreplaceable function - an effective response of the lungs (variation of the frequency and amplitude of respiratory movements) to various factors (for example, oxygen deficiency). This also explains the hyperventilation and functional impairment of the respiratory muscles that occurs with hypothyroidism.
Skeletal apparatus
. The thyroid gland is fundamental to skeletal development and formation: insufficient production of thyroid hormones during fetal development and childhood causes stunted bone growth, which can lead to dwarfism. Hormone replacement therapy will ensure normal skeletal development, but only if the problem is diagnosed and treated before puberty.
Digestive system.
The movement of the smooth muscles of the stomach and intestines is facilitated by thyroid hormones, so in conditions of hyperthyroidism diarrhea is observed, and in situations of hormonal deficiency (hypothyroidism) constipation can occur. In the latter case, the activity of the digestive system as a whole decreases, and the metabolism slows down with subsequent weight gain.
Reproductive system
. Excess or deficiency of thyroid hormones can cause infertility and reproductive problems, especially in women. In women suffering from hypothyroidism, there is an increase in the production of prolactin (a hormone secreted by the pituitary gland). This can cause menstrual irregularities or even amenorrhea (complete absence of periods). In men, thyroid dysfunction can cause erection problems and, in extremely rare cases, infertility.
Apparatus for hematopoiesis.
Thyroid hormones influence the production of red blood cells (erythropoiesis), which originate in the bone marrow. In the case of hypothyroidism, anemia often occurs, while in the presence of increased hormonal activity, the production of red blood cells is stimulated due to increased oxygen demand in the tissues.
Thyroid cancer screening
A comprehensive examination aimed at identifying specific markers (hormones, immunoglobulins) for diagnosing malignant tumors of the thyroid gland, monitoring the effectiveness of treatment, as well as timely detection of cancer relapses in patients with a removed thyroid gland.
What biomaterial can be used for research?
Venous blood.
Research method
Chemiluminescent immunoassay: serum calcitonin;
Solid-phase chemiluminescent enzyme-linked immunosorbent assay: thyroglobulin, antibodies to thyroglobulin.
How to properly prepare for research?
- Do not eat for 12 hours before the test; you can drink clean still water.
- Avoid taking oral contraceptives for 30 days before the study.
- Avoid physical and emotional stress for 24 hours before the test.
- Do not smoke for 24 hours before the test.
General information about the study
The thyroid gland is the largest endocrine gland in the human body. The thyroid hormones thyroxine (T4) and triiodothyronine (T3) are synthesized from the amino acid tyrosine in the follicular cells of the gland. A necessary structural component of thyroid hormones is iodine.
The effects of thyroid hormones are varied. They ensure the maintenance of basic metabolism in most cells of the body, regulating their metabolic activity. A normal level of thyroid hormones is necessary for the functioning of all body systems without exception; in cases of dysfunction of the thyroid gland, pathological changes are systemic in nature. It is very important to remember that thyroid hormones are necessary for the formation of the fetal nervous system during intrauterine development.
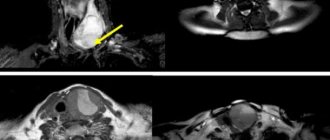
Thyroid cancer is a malignant nodular formation that develops from the follicular or parafollicular (C-cell) epithelium of the thyroid gland. There are follicular, papillary, medullary, anaplastic cancer and lymphoma of the thyroid gland, as well as its metastatic lesions. Clinically, thyroid cancer is manifested by difficulty swallowing, a feeling of constriction and pain in the throat, hoarseness, cough, weight loss, weakness and sweating. Diagnosis is carried out using ultrasound, MRI and thyroid scintigraphy. The main criterion is the detection of cancer cells in the material obtained from a gland biopsy.
An important stage in the diagnosis and treatment of thyroid diseases was the emergence of methods that make it possible to determine the concentration of thyroid hormones.
Calcitonin is a thyroid hormone synthesized in parafollicular cells, one of the main regulators of calcium-phosphorus metabolism. This is a tumor marker that allows you to confidently diagnose medullary cancer even in the early stages. The calcitonin test is extremely important in diagnosis, including the detection of multiple endocrine neoplasia syndrome (MEN-IIa, Sipple's disease), which can manifest as medullary carcinoma, adrenal medulla tumor (pheochromocytoma), or parathyroid hyperplasia and hyperparathyroidism.
Thyroglobulin (TG) is a prohormone of the thyroid gland, which is a marker of relapse of well-differentiated malignant neoplasms of the thyroid gland and is used to monitor the treatment of these diseases. This is a prohormone necessary for the further synthesis of thyroxine (T4) and triiodothyronine (T3). The thyroid gland is the only source of thyroglobulin in the body. The secretion of TG is controlled by thyroid-stimulating hormone. The half-life of TG in blood plasma is 3-4 days. Normally, only a small part of TG enters the bloodstream, about 10%. However, with malignant thyroid tumors, this situation changes dramatically - tumor cells release significant amounts of TG into the bloodstream. This effect is observed in all patients with metastases of differentiated thyroid cancer, regardless of the ability of the tumor to accumulate iodine. Therefore, in clinical endocrinology, TG is used as a marker of thyroid cancer.
Its production occurs in the cells of the normal thyroid gland, as well as in the cells of highly differentiated malignant neoplasms of this organ (papillary and follicular adenocarcinoma). Determining the concentration of thyroglobulin in the blood is used to monitor treatment and timely diagnose the recurrence of these thyroid tumors. The study is characterized by high specificity and sensitivity, but has some limitations. The presence of antibodies to thyroglobulin in the blood (found in 20% of patients with thyroid cancer) interferes with the reaction and can lead to a false negative result. Therefore, when performing a thyroglobulin test, the presence of antibodies to thyroglobulin in the blood is simultaneously assessed. In addition to specific antibodies, other (heterophilic) antibodies observed in cytomegalovirus infection, toxoplasmosis and infectious mononucleosis can also interfere with the reaction. A false negative result is possible with a very small tumor. Also, the result will be negative when testing the blood of a patient with a recurrent tumor that secretes defective thyroglobulin or does not produce this hormone.
It is important to understand that diagnosing relapse of thyroid cancer based on an increase in thyroglobulin levels is only possible for those patients who have previously had their thyroid gland removed.
Antithyroglobulin antibodies (ATTG) are specific immunoglobulins directed against the precursor of thyroid hormones. They are a specific marker of autoimmune thyroid diseases (Graves' disease, Hashimoto's thyroiditis). ATTG can block thyroglobulin, disrupting the normal synthesis of thyroid hormones and causing hypothyroidism, or, conversely, overstimulate the gland, causing its hyperfunction.
What is the research used for?
- For the diagnosis of medullary thyroid cancer;
- to detect multiple endocrine neoplasia syndrome (MEN-IIa, Sipple's disease), which can manifest as medullary cancer, adrenal medulla tumor (pheochromocytoma) or parathyroid hyperplasia and hyperparathyroidism;
- to find out whether there are metastases of medullary thyroid cancer;
- for indirect assessment of the size of medullary carcinoma;
- to evaluate the result of surgery to remove medullary thyroid cancer;
- to monitor treatment and timely detect relapse of papillary and follicular adenocarcinoma of the thyroid gland;
- for postoperative monitoring of patients with thyroid cancer to exclude relapse and metastases (together with thyroglobulin analysis).
When is the study scheduled?
- If medullary carcinoma is suspected (with nodular formations of the thyroid gland, an increase in its size, enlargement of regional lymph nodes);
- when diagnosed with pheochromocytoma, hyperparathyroidism to exclude multiple endocrine neoplasia syndrome (MEN IIa);
- before and after surgery to remove medullary carcinoma;
- if one of the patient’s relatives had medullary cancer;
- all patients 6-12 months after thyroidectomy;
- for patients with a high risk of relapse - regularly every 6 months; for patients with a low risk of relapse - regularly every 12 months.
What do the results mean?
The diagnosis of a tumor disease can only be established comprehensively - taking into account all complaints, signs, results of laboratory and instrumental studies. To make a diagnosis, a biopsy and histological examination of a sample from the affected organ is mandatory.
Calcitonin
Reference values: women: 0 - 6.4 pg/ml; men: 0 - 9.52 pg/ml.
- Any situation where a patient has a high level of calcitonin, regardless of the degree of its increase compared to the norm, requires an in-depth examination with the participation of specialists with sufficient experience in diagnosing and treating medullary thyroid cancer.
- If a calcitonin level exceeds 100 pg/ml, the probability of the patient having medullary cancer is almost 100%.
Thyroglobulin
Reference values: 1.4 - 78 ng/ml.
- A blood test for thyroglobulin becomes reliable 3 months after surgical treatment and 6 months after radioactive iodine therapy
- An increase in antibodies to thyroglobulin neutralizes the diagnostic value of the test for thyroglobulin - with high antibodies it will always be at low values, since antibody molecules will bind protein molecules and “mask” them from detection.
- A blood test for thyroglobulin, taken while taking thyroxine and at the same time having a low level of the hormone TSH in the blood, may be a sign of relapse of thyroid cancer, but in 20-25% of cases, relapses of thyroid cancer will not lead to an increase in thyroglobulin if the TSH level is low. Nevertheless, a blood test for thyroglobulin taken while taking thyroxine has diagnostic value and should be used in clinical practice.
- A blood test for thyroglobulin, taken after stopping thyroxine for 3 weeks, is the most accurate indicator of tumor relapse (a prerequisite for using this test in practice is the absence of elevated antibodies to thyroglobulin in the blood).
- In many cases, it is not the level of thyroglobulin in the blood that is of greater importance, but the dynamics of its change. If it is moderately elevated and falls over time, this is much better than if its level gradually increases.
Antibodies to thyroglobulin
Reference values: 0 - 115 IU/ml.
More details about the meaning of the results:
Detailed interpretation of test results: [08-027] Serum calcitonin
Detailed explanation of the analysis results: [08-051] Thyroglobulin
Detailed explanation of the analysis results: [13-087] Antibodies to thyroglobulin (antiTG)
What can influence the result?
- The presence in the serum of specific antibodies to thyroglobulin, as well as heterophilic antibodies (with cytomegalovirus infection, infectious mononucleosis and toxoplasmosis) can lead to a false negative result;
- oral contraceptives can increase the level of ATTG in the blood;
- the production of antibodies may be limited to lymphocytes within the thyroid gland, which will lead to negative results with inflammatory changes in the structure of the thyroid gland;
- the absence of antibodies to TG in patients with autoimmune thyroiditis is due either to the presence of bound thyroglobulin-antibody complexes in the blood, or to the formation of antibodies to another antigen.
Important Notes
- The result of the analysis should be evaluated together with data from additional laboratory and instrumental studies.
Who orders the study?
Endocrinologist, oncologist, therapist, surgeon, general practitioner, pediatrician.
Also recommended
- Complete blood count (without leukocyte formula and ESR)
- Erythrocyte sedimentation rate (ESR)
- Thyroid-stimulating hormone (TSH)
- Free thyroxine (free T4)
- Free triiodothyronine (free T3)
- Carcinoembryonic antigen (CEA)
- Prolactin
- Thyroid function
- Total metanephrine and total normetanephrine in urine
Literature
- Gimm O, Heyn V, Krause U, Sekulla C, Ukkat J, Dralle H. Prognostic significance of disseminated tumor cells in the connective tissue of patients with medullary thyroid carcinoma. World J Surg. 2006 May;30(5):847-52.
- Pacini F, Castagna MG, Cipri C, Schlumberger Medullary thyroid carcinoma. 2010 Aug;22(6):475-85. doi: 10.1016/j.clon.2010.05.002.
Hormonal imbalances
There are several diseases associated with the level of thyroid hormones:
- hyperthyroidism – increased levels of hormones. They affect biochemical processes in the body;
- Hypothyroidism is a condition caused by an underactive thyroid gland. The gland is unable to synthesize the amount of hormones T3 and T4 adequate to the needs of the body, and this determines a decrease in all metabolic processes;
- a disease associated with anatomical changes in the thyroid gland, in which the level of hormones is normal.
Indicators used to determine the condition of the thyroid gland
The activity and correct functioning of the gland is determined not only by free and bound fractions and.
The hormone that regulates thyroid function is pituitary thyroid-stimulating hormone (TSH). The production of this hormone changes under the influence of the concentration of T3 and T4 in the blood. When the concentration of hormones is low, the production of TSH increases, and it, in turn, stimulates the formation and release of T3 and T4 into the blood. It turns out that there is a kind of circular regulation of the gland. Therefore, a low TSH level may indicate increased thyroid function, and a high TSH level may indicate decreased thyroid function.
Two more informative indicators are the determination of the level of antibodies to thyroid peroxidase (antibodies to TPO) and thyroglobulin (antibodies to TG). Thyroglobulin is a protein from which hormones are formed in the thyroid gland. Thyroid peroxidase is a very important enzyme, without which the formation of thyroid hormones is impossible. Antibodies to them appear in the blood when gland cells are damaged for a specific reason, for example, gland cancer or autoimmune inflammation.
Therefore, determining the function of the thyroid gland using a blood test is the most accessible and effective method for diagnosing and preventing diseases of this organ.
Sign up for testing
Hypothyroidism
Deficiency of thyroid hormones causes the following symptoms, which are the reason for an urgent visit to an endocrinologist:
- Depression and fatigue, especially when waking up and resting, loss of memory, concentration and learning ability, drowsiness, apathy, disinterest, decreased speed of thought and speech, alternating with nervousness and hyperactivity;
- Dry and pale skin, hair loss and dryness, thinning of the outer eyebrows, brittle nails with grooves, constipation, poor digestion, low body temperature, poor sweating in the heat;
- High risk of infection, weakened immune defense and predisposition to cancer;
- Decreased insulin sensitivity, metabolic syndrome, slow heartbeat, increased cholesterol and diastolic pressure, atherosclerosis, increased risk of death from heart disease (heart failure, coronary artery disease, arrhythmias);
- Night muscle cramps, myalgia, pain and stiffness (especially in the morning), headache, menstrual irregularities, uterine bleeding, infertility, tendency to terminate pregnancy, decreased tendon reflexes, enlarged thyroid gland (endemic goiter).
Reduced thyroid function will have consequences in many other hormonal areas. In particular, hypothyroidism creates a stressful situation that stimulates the adrenal glands, contributing to its development towards decompensation. “Adrenal fatigue” and hypothyroidism are often related (in 80% of cases) and aggravate each other.
The most common causes of hypothyroidism are autoimmune diseases (Hashimoto's thyroiditis), iodine deficiency, and problems with the hypothalamus and pituitary gland (the rarest hypothesis).
Hypothyroidism is an irreversible pathology. This means that the thyroid gland cannot resume its regular functioning. For this reason, the therapy taken is defined as “replacement”, in the sense that it is intended to replace hormones that the thyroid gland can no longer produce.
Hyperthyroidism
An overactive thyroid gland causes predominantly opposite symptoms:
- endemic goiter - the thyroid gland has increased in size;
- hair began to fall out rapidly and nails began to break;
- bulging eyes appeared;
- sudden outbursts of aggression, nervousness, anxiety;
- irritability gives way to tearfulness;
- tremors in the hands;
- increased sweating;
- rapid weight loss;
- causeless fatigue and weakness, insomnia;
- increased body temperature (at low temperatures a person is not cold);
- increased heart rate (tachycardia);
- suffers from diarrhea;
- dystrophic changes in the liver (with a long course of the disease);
- in severe cases, women experience uterine bleeding, and men experience changes in the testicles and prostate gland, decreased libido.
One of the most common causes of the disease is Graves' disease, an autoimmune disease that causes the body to produce autoantibodies that activate the secretion of thyroid hormones. Also, overactivity of the gland can be caused by Hashimoto's thyroiditis, toxic, taking certain medications or supplements with a high iodine content, etc.
Hyperthyroidism can usually be diagnosed and treated in a clinic without the need for hospitalization. Various types of treatment are possible: pharmacological, surgical, with radioactive iodine and, in the case of toxic adenoma, by alcoholization. The doctor prescribes the most appropriate therapy depending on the specific pathology.
Check-up “thyroid gland”
Thyroid
– a vital endocrine organ. The main regulator of basal metabolism. Therefore, even for healthy people, once every 2-3 years it is useful to check how this organ functions. Well, those who already suffer from one of the thyroid diseases need to be examined at least once a year. Since, if a deviation in the functioning of the gland is detected in time, the situation can be corrected with medications, without surgery or other invasive manipulations. Preventive measures are indicated for absolutely everyone, regardless of age and gender.
The thyroid gland controls metabolism and is responsible for:
- Breathing and thermoregulation.
- Heart rate.
- Mental condition.
- Muscle strength and weight.
- Blood cholesterol level, etc.
Thyroid diseases
- one of the most common in the modern world. And in terms of frequency of occurrence among endocrine pathologies, they are in second place after diabetes mellitus.
Diseases of the thyroid gland in the early stages are often asymptomatic or occur with mild symptoms. The presence of violations can only be determined using laboratory diagnostics.
You should definitely get examined if you experience symptoms such as
causeless loss or sudden weight gain, heart failure, constant depression, decreased body defenses, hair loss, brittle nails, skin problems.
The thyroid gland produces, accumulates and releases thyroid hormones into the blood - triiodothyronine (T3) and thyroxine (T4), which regulate metabolic, energy and heat exchange processes in the body.
T4
- This is an iodine-containing hormone of the thyroid gland - thyroxine. Thyroxine (T4) makes up about 90% of the total amount of hormones secreted by the thyroid gland. In the blood, T4 is found free (only 0.1%), and the main part is bound to globulin proteins. It is the free fraction of the T4 hormone that is the most biologically active.
The concentration of the hormone T4 in the blood serum changes throughout the day and reaches its maximum at 8.00 -12.00. The lowest levels occur late at night. Also, fluctuations in thyroxine depend on the season of the year. It turned out that in the autumn-winter period the level of the hormone increases and reaches maximum values, after which it decreases.
Antibodies to thyroid peroxidase (Anti-TPO)
– specific immunoglobulins. The thyroid enzyme thyroid peroxidase plays a key role in the formation of thyroid hormones. Thyroid peroxidase is involved in the formation of the active form of iodine, without which the formation of thyroid hormones T4 and T3 is impossible. The appearance of antibodies to this enzyme in the blood disrupts its normal function, resulting in a decrease in the production of the corresponding hormones.
This analysis is aimed at determining specific antibodies to thyroid tissue in the blood serum. These antibodies are formed when the human immune system mistakenly recognizes thyroid tissue as a foreign biological substance, and this can lead to thyroiditis, damage to the thyroid tissue and various disorders of its function.
Anti-TPO is a specific marker for autoimmune thyroid diseases.
Thyroid-stimulating hormone (TSH)
- the main regulator of thyroid function, synthesized by the pituitary gland, a gland located in the brain. Its main function is to maintain a constant concentration of thyroid hormones - thyroid hormones. When their levels in the blood decrease, the hypothalamus releases a hormone that stimulates the secretion of TSH by the pituitary gland.
Pituitary dysfunction can cause thyroid-stimulating hormone levels to rise or fall. When its concentration increases, thyroid hormones are released into the blood in excess quantities, causing hyperthyroidism. At the same time, there is an increase in heart rate, weight loss, and anxiety. A life-threatening condition is thyrotoxic crisis - a severe form of the disease.
As the concentration of TSH decreases, the production of thyroid hormones also decreases and symptoms of hypothyroidism develop; patients with this diagnosis complain of fatigue, weakness, depression, and menstrual irregularities in women; increased sensitivity to cold, dry skin, constipation.
An analysis of TSH levels is a basic test for assessing the functioning of the thyroid gland in hypothyroidism and hyperthyroidism.
It is recommended to donate blood in the morning between 8 and 11 am. Blood is drawn on an empty stomach, after 6–8 hours of fasting. It is allowed to drink water without gas and sugar. On the eve of the examination, food overload should be avoided.
When monitoring the dynamics of the indicator, it is recommended to donate blood at the same time of day.
Recent effects on the thyroid gland, including surgery, radiation therapy, drug therapy (including taking thyroid hormones, iodine-containing drugs), may affect the test result. One week before the test, you must stop taking thyroid hormones. 2-3 days before the procedure, do not take medications containing iodine. The conditions and time of the study are determined by the attending physician. If the test results indicate an endocrine disease and the thyroid gland is enlarged, additional laboratory and instrumental (ultrasound) examination is necessary under the supervision of the attending physician.
Hormone analysis
A blood test for thyroid hormones is necessary if the above symptoms are present. Blood is taken from the ulnar vein on an empty stomach in the morning. Before this, you need to be at rest for half an hour.
Preparation for analysis implies compliance with the following rules:
- stop smoking, drinking alcohol and psychostimulants (caffeine) one day before;
- for 2-3 days, exclude fried, hot, spicy and other heavy foods from the diet;
- avoid physical and emotional stress for 12 hours;
- stop taking medications that affect the level of thyroid hormones one month before;
- 3-4 days in advance, exclude iodine-containing foods (seaweed, fish, iodized salt) from the diet.
A complete and detailed biochemical study includes assessment of the following indicators:
| Index | Norm |
| Thyroid-stimulating hormone (TSH) | 0.4 – 4.0 mU/l |
| Triiodothyronine T3 free | 2.6 – 5.7 pmol/l |
| T3 general | 1.3 – 2.7 nmol/l |
| Thyroxine T4 free | 9.0 – 22.0 pmol/l |
| T4 general | 58 – 161 nmol/l |
| Antibodies to thyroglobulin (AT-TG) | 0 – 18 U/l |
| Antibodies to thyroid peroxidase (AT-TPO) | No more than 5.6 U/l |
| Calcitonin | In men: 0 – 2.46 pmol/l. In women: 0 – 1.46 pmol/l. |
The normal level of hormones is largely determined by the intensity of physical activity, emotional state and time of year. For certain categories of people, hormone levels may also differ.
These include:
- people over 50 years old;
- teenagers;
- children under 12 years of age;
- children of “turning-point” age;
- pregnant women.
The doctor may prescribe the determination of only some of these indicators. So, to treat the thyroid gland, it is enough to determine only two indicators - free T4 and TSH. During pregnancy, 4 indicators are determined - TSH, free T3, free T4 and AT-TPO. Due to the laboriousness and high cost of the procedure for determining each indicator, it is recommended to study only those indicators, changes in which may be the cause of the corresponding symptoms.
Profile No. 13, Examination of the thyroid gland - extended
Home / For clients / Comprehensive studies / The set of tests included in the package collectively costs 5% - 15% less than each test separately. / Profile No. 13, Examination of the thyroid gland - extended
Article rating: 4.48 (88)
Currently, thyroid diseases are among the most common in the world. In the UK, more than 1% of the UK population receives thyroid hormones. The high prevalence of thyroid diseases puts them on a par with diseases such as diabetes and diseases of the cardiovascular system. According to some reports, the prevalence of thyroid diseases is even higher than currently known. This is due to the frequent asymptomatic course of many of her diseases.
Thyroid gland (TG)
- a small organ weighing about 20 g, located on the front surface of the neck. Together with other glands, it produces biologically active substances - hormones. Throughout life, hormones play a critical role in almost every process that occurs in our body. All glands of the endocrine system closely interact with each other, which explains the fact that even with a slight shift in the function of one organ, changes occur throughout the body.
Hormones, released into the bloodstream by endocrine glands, act on tissues and organs of the body, which are often located at a considerable distance from the place of their formation. Endocrine glands are located in various parts of the body. Thus, the pituitary gland is part of the brain, the thyroid and parathyroid glands are located in the neck, the thymus is in the upper chest, the adrenal glands and pancreas are in the retroperitoneum, and the sex glands, or gonads, are in the pelvic cavity.
These glands produce and release more than 50 hormones into the blood. The hypothalamic-pituitary system plays the main role for the entire endocrine system.
A large number of diseases of the endocrine glands are known. However, almost all of them can be grouped into three large groups. So (1), the activity of the gland may decrease, which is accompanied by a decrease in the level of hormones in the blood. In the case of thyroid diseases, we are talking about hypothyroidism (“hypo” means decreased), that is, a decrease in the level of thyroid hormones. On the other hand (2), gland activity and hormone levels may increase. In diseases of the thyroid gland, we are talking about thyrotoxicosis - a persistent pathological increase in the function of the thyroid gland. And finally, many endocrine diseases and most thyroid diseases (3) occur without changes in the function of the endocrine glands.
Most hormones have receptors on the cells of their “target organs”. In this case, the specificity of the action of hormones is explained by their high affinity for the receptor. Most hormones fit into their receptors like a “key to a lock.”
The activity of the endocrine glands is regulated depending on the needs of the body. This is also carried out using receptors found on many cells. They detect small changes in the levels of various substances in the blood and transmit a signal to the endocrine glands. Those, in turn, change their activity so that the level of the original substance returns to normal. When this normal value is reached, the activity of the endocrine gland also returns to its previous level. According to this principle, the body regulates the levels of various substances throughout life.
The thyroid gland secretes two important hormones: thyroxine (T4) and triiodothyronine (T3), which regulate metabolism, the functioning of the cardiovascular system, gastrointestinal tract, mental and sexual activity.
The function of the thyroid gland is under the control of the hypothalamic-pituitary system. The hypothalamus synthesizes a substance that regulates the activity of the thyroid gland - thyrotropin-releasing hormone (TRH). This hormone, entering the pituitary gland, leads to the production of thyroid-stimulating hormone (TSH), which stimulates the activity of the thyroid gland and the formation of T4 and T3. Of these, the main hormone is T4. Reaching its “target organs”, it turns into T3, which directly affects the cell.
In the blood, most of the thyroid hormones are bound to the carrier protein and are inactive, while only a small free fraction of hormones is active and performs its functions. Some medications, including contraceptives, can affect the level of carrier protein in the blood, etc. on the level of hormones associated with it. In the past, this has skewed the results of hormonal studies when determining total hormone levels. Currently, as a rule, only the amount of free hormones in the blood is determined.
Another type of cell found in the thyroid gland produces and releases another hormone into the blood - calcitonin. It is involved in the regulation of calcium levels in the body, which is the main material for building bones, as well as a necessary substance for conducting impulses in nerve and muscle tissue.
Despite the small size of the thyroid gland, the hormones produced in it are involved in almost all processes of the body. Its main function is to maintain normal metabolism (metabolism) in the cells of the body. Thyroid hormones stimulate metabolism in almost all cells and regulate almost every process in the body - breathing, eating, sleep, movement, as well as processes in internal organs - from the heartbeat to the functioning of the reproductive system.
Thyroid hormones are necessary for normal mental and physical development. Along with growth hormone produced in the pituitary gland, they are responsible for the normal development of skeletal bones.
A lack of thyroid hormones in childhood leads to cessation of growth, and their deficiency during pregnancy leads to underdevelopment of the brain of the unborn child.
In healthy people, the thyroid gland also takes part in controlling body weight. With increased food consumption, its activity increases, the formation of T3 increases, which leads to an increase in the metabolic rate in the body. On the contrary, with malnutrition, thyroid activity decreases, leading to a slowdown in metabolism.
Thyroid hormones take part in the regulation of water-salt balance, in the formation of certain vitamins (for example, the formation of vitamin A in the liver), as well as in the function of other hormones in the body. For example, without thyroid hormones the effect of growth hormone on the brain is impossible.
The role of the thyroid gland in the normal development of the mammary glands in women has been proven. The thyroid gland plays an important role in the functioning of the body's immune system. Its hormones stimulate immune system cells called T cells, which the body uses to fight infection. It is assumed that changes in thyroid function play an important role in the aging of the body.
A package of laboratory tests that allows you to judge the condition of the thyroid gland.
- Thyroid-stimulating hormone (TSH)
- Free thyroxine (free T4)
- Free triiodothyronine (free T3)
- Antibodies to thyroid peroxidase (AT-TPO)
- Antibodies to thyroglobulin (AT-TG)
Profile cost
– 2052 rub.
Execution time: 1-2 days
Preparing for analysis
Note:
Blood sampling for testing is paid additionally. The cost of taking blood is 110 rubles.
© 2013 - 2021 copyright holder LLC "TIAS LOTUS"
History and philosophy of the company Personal data processing policy For citizens with disabilities Preparation for analyzes Phone numbers of higher-level organizations State guarantee program Payment methods Help for the Federal Tax Service Contacts Our partners
Gemohelp mobile application
8-800-100-08-05
Call if you have any questions
By using the website www.gemohelp.ru, you agree to the use of cookies
I confirm
More details
Select city:
- Arzamas
- Balakhna
- Bogorodsk
- Bor
- Vacha
- Vyksa
- Dzerzhinsk
- Trans-Volga region
- Kstovo
- Kulebaki
- Lukoyanov
- Lyskovo
- Moore
- Navashino
- Nizhny Novgorod
- Pavlovo
- Sarov
- Semenov
- Sosnovskoe
- Cheboksary
- Chkalovsk
Confirm
What does a change in hormone levels indicate?
Based on the results of the analysis, the endocrinologist determines the diagnosis or condition of the body.
| Violation | T3, T4 | TSH |
| Primary hypothyroidism | Decreased or normal | High |
| Secondary hypothyroidism | Short | High |
| Hyperthyroidism | Elevated | Reduced |
| Both dysfunctions can be a sign of certain malfunctions in the body. For example, an increased level of thyroxine is observed with obesity and diffuse goiter, and a decreased level is observed with fasting, during pregnancy and taking certain medications. | ||
| Hormone | Promotion | Demotion |
| TSH | hypothyroidism; adrenal insufficiency; psycho-emotional arousal; tumor; severe non-thyroid pathology; a consequence of taking morphine and other drugs. | primary hyperthyroidism; thyrotoxicosis |
| T4 free | hyperthyroidism; obesity; somatic and mental disorders; dysfunction of the adrenal glands. | III trimester of pregnancy; hypothyroidism; starvation; high physical activity. |
| T4 general | obesity; acute form of hepatitis; inactive phase of HIV; porphyria; hyperbilirubinemia; during pregnancy. | starvation; kidney diseases; gastrointestinal diseases; many somatic pathologies. |
| T3 general | excessive thyroid function; hepatitis; pregnancy; AIDS; porphyria. | hypothyroidism; starvation; hemolysis; diseases of the gastrointestinal tract, kidneys and liver. |
Additional indicators:
- TG. An increased level of the hormone is a sign of non-toxic, endemic, multinodular or diffuse goiter, thyroid cancer, thyroiditis;
- AT-TPO. Exceeding the norm indicates the development of a malignant tumor;
- Calcitonin. It is one of the basic tumor markers and indicates the presence of a malignant process.
- AT-TG. An excess of the normal value may indicate Graves' disease, thyroiditis, idiopathic myxedema, pernicious anemia, thyroid carcinoma (cancer) or other autoimmune and chromosomal pathologies.
Prevention
In order to prevent thyroid diseases associated with hormonal imbalance, or eliminate minor disruptions, it is necessary to ensure that the body receives a sufficient amount of tyrosine and iodine from food.
The main iodine-containing products are sunflower oil, iodized salt, kelp seaweed, crabs, fish (oceanic), shrimp, squid, etc. Tyrosine is found in eggs, milk, peanuts, peas, and beans. Maintaining hormonal balance is the key to a healthy thyroid gland. And all you need for this is a complete and balanced diet. Also, do not forget about regular visits to the endocrinologist. Checking once every 3 months is sufficient.
If you find an error, please select a piece of text and press Ctrl+Enter