A postoperative bandage is a product that helps a person rehabilitate after surgery in the abdominal area. The corset will reduce the recovery process. Doctors recommend wearing a bandage after bypass surgery, spinal surgery and cesarean section. The corset helps relieve stress from the injured area and speed up recovery.
The abdominal bandage after surgery is a wide belt made of special elastic materials. The bandage performs the functions of the anterior abdominal wall of a person if the wall itself is damaged, as in the case of a hernia or postoperative suture.
How does a post-operative bandage help?
The product fits snugly to the body and supports the internal organs in a healthy position. This prevents them from moving, reduces swelling and prevents the appearance of hematomas. The bandage after cesarean section protects postoperative sutures and ensures their rapid scarring. Certain product models prevent the occurrence of hernias and prevent infection of sutures.
With the help of a bandage, the elasticity of the skin is restored. And the load will be distributed evenly across the back, thereby eliminating discomfort and pain in this area while walking. The skin is also quickly restored and the chance of the formation of hernias, swelling, and hematomas in the abdominal area is reduced.
In what cases will you encounter contraindications to wearing an abdominal bandage?
- In the case of a special type of seam (for example, longitudinal);
- In case of inflammation of the seam;
- In case of edema caused by disruption of the cardiovascular system;
- In case of a tendency to swelling caused by improper functioning of the kidneys;
- In case of diseases of the gastrointestinal tract;
- In case of dermatitis, eczema, neurodermatitis and other violations of the integrity of the skin (ulcers, abscesses, bedsores);
- In case of varicose veins (if we are talking about a leg model).
Attention! The degree of need for a postoperative belt is determined by the attending physician. Do not aggravate the situation by self-medication and follow the instructions.
Types of postoperative bandages
Today there are many types of postoperative bandages. They differ in the type of product in the likeness of which they were made.
Bandage belt
This model is divided into soft and hard versions. Experts recommend using the first one to fix and protect surgical sutures. A soft bandage belt is recommended to be worn after liposuction to hold the hernial sac in case of umbilical, periumbilical hernias and hernias of the white line of the abdomen, childbirth.
A medium-hard bandage belt can be worn as a preventive measure. They use special plastic plates to support the spine, for which some manufacturers classify them as corsets. The big advantage is that plastic plates accept the natural bend of a person, thereby supporting and distributing the load. Doctors prescribe it during the rehabilitation period after injuries, for lumbago, myositis, osteochondrosis, osteoarthrosis, lumbar spondylosis, osteoarthritis and diseases of the spinal ligaments.
The plates of the rigid bandage-belt are made of metal and are suitable for cases where activity and tension are dangerous for well-being. Corsets with metal ribs are prescribed primarily by the attending physician.
Bandage panties
Such models are used after all types of operations on the abdominal organs, including cesarean section for:
- Prevention of hernia formation
- After liposuction and laparoscopy
- Prevention of downward displacement of abdominal organs
- In the postpartum period to create the necessary compression, ensuring restoration of the original shape
Terms of use
The method of applying the bandage and the duration of its use depends on the recommendations given by the attending physician. As a rule, after abdominal surgery, the bandage is worn from 2 weeks to 3 months. During this time, the tone of the peritoneal muscles has time to restore and the correct formation of the scar occurs.
General recommendations for using the bandage:
- The bandage should be worn over cotton underwear without seams. If the accessory must be worn directly on the body, in order to maintain the proper level of hygiene, it is necessary to have at least two replaceable bandages.
- Wearing a bandage all the time is not recommended. Experts advise taking a break from the accessory during the day.
- It is not recommended to wear the bandage while sleeping.
In any case, recommendations for the correct use of bandages may differ in each specific case and should be prescribed by the attending physician.
How to put on a bandage correctly?
The bandage is put on so that the narrow part of the product is below the abdomen, and the wide part is on the lower back and helps to maintain the back in a healthy position.
For the first time, it is better to put on the bandage while lying down, raising your hips - in this position, the abdominal organs will be able to take the correct position.
How to put on a bandage:
- Place the product on the bed
- Lie on the bandage with your back, raising your hips for a few minutes
- Lower your hips
- Lie down for a few minutes
- Fasten the bandage so that your palm fits between it and your stomach.
After getting out of bed, you will feel that your stomach has become lighter and your back has stopped hurting. Wearing a bandage will make it easier to walk, move and lead an active life.
Contraindications
Despite all the benefits that come from using bandages after abdominal surgery, there are a number of contraindications in which using accessories can be hazardous to health.
Thus, bandages are not recommended for patients who:
- presence of open wounds on the body;
- suppuration on the seam;
- rashes on the body at the point of contact with the bandage;
- reaction in the form of rashes on the body at the point of contact with the tissue.
Which bandage is best after a caesarean section?
An excellent option for choosing a postoperative bandage after a cesarean section would be a bandage belt and a bandage pant. Such models reduce the load and speed up the rehabilitation process. In addition to relieving nagging pain during movement, the bandage is also indicated for other purposes. It is prescribed to:
- fix the abdominal muscles and thereby keep the internal organs in the correct position
- reduce the risk of hernia
- remove excess stress on the back muscles
- prevent divergence or stretching of postoperative sutures.
In addition to the type and size, when buying a bandage you should pay attention to such characteristics as:
- material – it is advisable to choose natural fabrics that are pleasant to the skin
- design – to minimize unnecessary friction and injuries, instead of lacing, snaps and buttons on the corset, you can choose a Velcro bandage.
How long to wear a bandage after a caesarean section?
The period of wearing a bandage after a cesarean section is about two weeks. But in rare cases, the period can be extended to three months.
- You should not wear the product constantly. The maximum total amount of time per day is 6 hours.
- Doctors recommend removing the bandage every 2 hours
- The bandage must be removed at night
- It is recommended to wear the bandage over cotton and seamless clothing.
When should the gallbladder be removed?
1. Acute cholecystitis . If bacteria enter the gallbladder through the bile ducts or along with the bloodstream, inflammation occurs, which is called cholecystitis. Since inflammation of the gallbladder poses a risk of liver damage and blood poisoning, acute cholecystitis is treated surgically. 2. Gallstone disease . Stagnation of bile in the gallbladder, excess weight and hormonal changes during pregnancy provoke bile stagnation. Settled at the bottom of the gallbladder, bilirubin crystals, calcium salts and cholesterol form gallstones. To avoid “obstructive jaundice” due to stone blockage of the mouth of the bile duct, in case of cholelithiasis, the gallbladder is removed.
Where to buy a postoperative bandage?
The online pharmacy 24farmacia offers different options for bandages for treatment and prevention. To order, add the product you like to your cart and place your order online. Or call 8 (391) 2911 555.
Delivery is carried out to the Provincial Pharmacies network or to the door of your home. Courier delivery is carried out on weekdays from 10:00 to 23:00 and on weekends from 10:00 to 24:00 only in the city of Krasnoyarsk. The order can be paid online or at the place of receipt of the order using a bank card.
How is cholecystectomy performed?
There are different techniques for performing cholecystectomy, each of which has its own advantages and disadvantages and is optimal in certain cases.
Laparoscopic cholecystectomy
Currently, gallbladder removal is most often performed laparoscopically. Typically, the operation is performed through 3-4 punctures in the abdominal wall; in some cases, more may be required. One of the punctures is made in the navel area, through which a laparoscope is inserted - an instrument with a video camera and a light source. An insufflator is also connected to the laparoscope, through which the abdominal cavity is filled with carbon dioxide. This is necessary to provide the surgeon with a good view and space for manipulation.
Special surgical instruments are inserted through the remaining punctures. They are used to carefully isolate the cystic duct and artery, clamp them with clips and cross them. After the gallbladder is isolated, it is removed through one of the punctures.
When the operation is completed, the instruments are removed and stitches are placed on the punctures.
Operation through one puncture
In recent years, an improved method of laparoscopic removal of the gallbladder - single-port cholecystectomy - has been actively developing. In this case, only one puncture is made in the navel area. A laparoport is installed into it, through which several instruments can be inserted at once. Such interventions are optimal for uncomplicated chronic calculous cholecystitis. Their main advantage is an excellent cosmetic effect and the absence of a noticeable scar.
Open cholecystectomy
In an open cholecystectomy, the surgeon makes a vertical incision in the middle of the abdomen (midline laparotomy) or an oblique incision under the right lower costal arch. The gallbladder is isolated, ligated (or clipped) and divided in the same way as during laparoscopic surgery.
As noted above, in some cases open surgery is the best option, because during it the surgeon can fully examine the gallbladder and neighboring organs, as well as conduct intraoperative studies:
- probing the bile ducts and measuring their width;
- cholangiography;
- choledochotomy (opening of the bile ducts) and endoscopic examination;
- ultrasonography.
Minimally invasive open cholecystectomy
In some cases, it is possible to perform a minimally invasive operation, limiting yourself to a small incision 3–5 cm long in the right hypochondrium. This intervention has many of the advantages of open cholecystectomy, but is accompanied by less tissue trauma and shorter hospitalization and recovery periods.
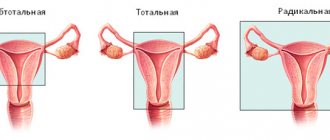
Extended radical cholecystectomy
This is the most complex operation used for malignant tumors. If only the gallbladder is removed during cancer, then the risk of relapse is high. The minimum scope of the operation involves removing the gallbladder, several centimeters of adjacent liver tissue, and all nearby lymph nodes.
In some cases, the following may be removed: part of the liver, common bile duct, pancreas, additional groups of lymph nodes, duodenum and other organs affected by a malignant tumor.
We will call you back, leave your phone number
Message sent!
expect a call, we will contact you shortly
conclusions
1. The study indicates the activation of angiogenesis in ovarian tissue in patients with AU, expressed in a significant increase in the size and area of vessels, as well as in an increase in the expression of VEGF and its receptors both in the endothelium and in granulosa-luteal cells. The identified features of ovarian angiogenesis complement our understanding of the development of hemorrhage into the ovarian tissue in AU.
2. The study of systemic angiogenesis after the end of a complex of rehabilitation therapy showed that the level of VEGF significantly decreased in the blood serum of patients receiving Longidaza for the prevention of adhesions. Since activation of angiogenesis plays an important role in the formation of adhesions, an increase in the concentration of VEGF in patients who were not prescribed the drug Longidaza can be considered as an unfavorable prognostic factor for the risk of developing adhesions.
3. The clinical effectiveness of Longidaza as part of complex rehabilitation therapy is confirmed by data on a more favorable course of the postoperative period and rapid normalization of the ultrasound picture, the results of hysterosalpingography, laparoscopy and the pregnancy rate compared with those in patients who did not receive the enzyme drug.
4. The results obtained convince us of the validity of including the drug Longidaza, which is characterized by a prolonged antifibrotic effect and a pronounced anti-inflammatory and anti-edematous effect, into the complex of rehabilitation measures after endosurgical treatment of ovarian cancer.