The optimal method of treating cholelithiasis
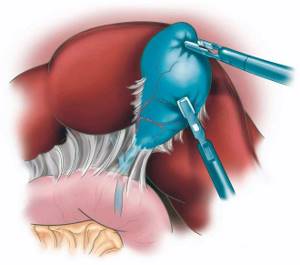
Today, the gold standard is laparoscopic cholecystectomy.
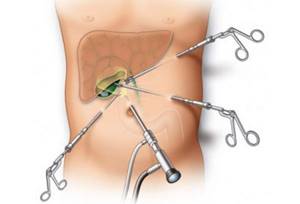
It is performed through three or four small incisions (punctures) using a special video camera and instruments. There is an option to perform it through one slightly larger incision in the navel area, without an incision at all (through the stomach), and even with the help of a robot, but they are not widely used (the advantages are not obvious, and the cost is higher). In the vast majority of cases, the length of stay in the clinic is two days: hospitalization on the day of surgery, discharge the next day after control of tests, ultrasound. Of course, the decision to discharge is always joint; if the patient feels better about staying under observation longer, we will always support him.
During the week after surgery, we usually recommend a gentle regimen, despite feeling quite well. The first two to three days may cause aching pain in the shoulder; this is associated with residual gas in the abdominal cavity and occurs after any laparoscopic surgery.
Features of the operation
This procedure is highly effective and at the same time low traumatic to the tissues of the pelvis and peritoneum. In recent years, this type of surgical intervention in the peritoneal cavity has become the most popular and frequently used, and the price has become more affordable. The procedure is indicated for gallstone disease, as it has a minimum of complications and allows recovery in a short time.

The surgical operation is carried out using special equipment (laparoscope) and instruments (trocars). A laparoscope is a tube with a camera at the end and equipped with a small flashlight. The equipment is inserted into the abdominal cavity through a small hole on the anterior wall of the peritoneum. The camera transmits the image to the monitor for the doctor performing the manipulation. Thanks to microscopic equipment, a specialist sees what is happening inside the human body without making a large abdominal incision with a scalpel.
Food poisoning is a pathological condition that can manifest itself with many symptoms. Among them, increased body temperature, or fever, is of considerable importance. Read more in the article: “can there be a temperature due to poisoning.”

Diet after cholecystectomy
The question is very debatable, in fact. In my opinion, rumors about the need for a strict diet are greatly exaggerated.
There is no reservoir function of the gallbladder; bile in its original form constantly enters the duodenum. In this regard, you need to eat more often (constantly), in small portions and limit fats (the bile located in the duodenum at any given time should be “enough” to emulsify fats). If you break the diet, nothing particularly terrible will happen, but the patient will understand it (it will be painful and diarrhea).
About complications of cholecystectomy
All complications can be divided into two types: those occurring immediately during or shortly after surgery; and remote (the notorious postcholecystectomy syndrome).
Most of the complications that arise during or immediately after surgery, fortunately, are “minor” and do not threaten life and health. These are hematomas, seromas, inflammation - in total about 5%, most often they do not require any special treatment, not to mention repeated operations.
There are, by and large, four serious complications during surgery - bleeding, injury to the bile ducts, pulmonary embolism and residual choledocholithiasis.
Despite the proven technique of laparoscopic cholecystectomy, it is not yet possible to completely eliminate them, even in clinics where extensive experience in performing these operations has been accumulated.
Bleeding
Bleeding is understandable - it can occur during any operation. With planned cholecystectomy, the risk is minimal.
Damage to the bile ducts
A nightmare for any surgeon. According to literature data, the frequency is 0.15–0.36% and depends on many factors: planned or emergency surgery (it is clear that planned risks are much lower), the severity of inflammatory and cicatricial changes in the gallbladder area, constitutional and anatomical features... There are a number of anomalies (relationships of anatomical structures in the gallbladder area), which sometimes baffle even a very experienced surgeon. The basic rule here is “if you're not sure, don't overtake,” in the sense that we must be absolutely confident in understanding the anatomy of a particular patient. Always. Every time. Even in the most “banal” cases.
Of course, the experience of the surgeon and the quality of the equipment are of great importance. There are a number of techniques that can minimize the risk of complications - the critical view of safety technique (for me and many colleagues it is mandatory during every operation), intraoperative cholangiography, and even the use of fluorescent laparoscopy (ICG). I think the technical features are not very interesting for “non-surgeons”, but nevertheless)
The next complication is pulmonary embolism
Fortunately, it is quite rare with laparoscopic cholecystectomy and proper prevention, although it is still impossible to prevent it 100%. Many factors influence, including the time of the operation, the amount of blood loss, the state of the coagulation system, the presence of varicose veins, age... All this is taken into account, the risks are determined and the optimal prevention option is selected.
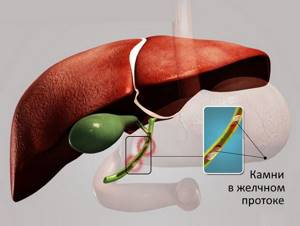
“Forgotten” stones in the bile duct or residual choledocholithiasis
A separate big topic for conversation like “If you remove the gallbladder, stones will continue to form in the ducts.” It has already been written many times - this is a very rare story, except in a situation like persistent cholangitis or cystic fibrosis. The vast majority of stones in the ducts after removal of the gallbladder were there at the time of removal, but did not manifest themselves in any way. Until recently, we did not have a safe way to diagnose asymptomatic choledocholithiasis. In recent years we have been actively using MRI (it is safe and informative). I think this will greatly reduce the number of “forgotten stones”.
Long-term consequences of gallbladder removal or postcholecystectomy syndrome (PCES)
I must say that there are quite a lot of myths and horror stories about this. I will try to express my point of view, based on my own experience and analysis of world literature.
As the name suggests, postcholecystectomy syndrome refers to any problems in the gastrointestinal tract after removal of the gallbladder.
Let me remind you that “after” does not always mean “as a result.” In most cases, these problems have nothing to do with the operation itself; often, upon careful analysis, it turns out that the patient had them before the operation. This once again emphasizes the need for careful clinical assessment and an individualized approach when deciding whether to remove the gallbladder. In my opinion, it is an insufficiently attentive assessment of the symptoms and the desire to remove the gallbladder at any cost that leads to the appearance of most comments like “They removed it - it only got worse,” etc.
Most often for the so-called. “PHES” take irritable bowel syndrome, gastroesophageal reflux, peptic ulcer disease and chronic pancreatitis. Muscle or neurogenic pain also cannot be written off. Why is the diagnosis of PCES made? Doctors are people too, and people tend to follow the path of least resistance.. “Does it hurt? Has the gallbladder been removed? Of course it’s PHES!” Identifying the true cause is not so easy, in fact.
If we do not take into account the previously described complications during the operation, the real long-term consequences of cholecystectomy include two problems: postoperative diarrhea and dysfunction of the sphincter of Oddi.
Approximate food menu
It should be noted that the menu described below can be used no earlier than 2 months after the operation. Until this point, restrictions on food consumption must be stricter. It is also necessary to take into account that the diet after excision of the gallbladder should be long-term; it is only possible to alternate between dishes that are allowed for consumption and those made according to special recipes.
8:00 - first breakfast:
- a piece of day-old white bread with apple jam - 120 g;
- buckwheat - 160 gr.;
- weakly brewed tea - 300 gr.
11:00 - second breakfast:
- carrot-apple juice with pulp - 300 g;
- cottage cheese - 170 gr.
14:00 - lunch:
- boiled chicken - 160 gr.;
- potato soup with vegetable broth (without hot herbs and spices, you can add a few bay leaves to the soup after cooking) - 260–320 g;
- bread - 160 gr.;
- as a side dish, zucchini puree - 130 g;
- weakly brewed tea - 300 gr.
17:00 - afternoon snack:
- bread - 120 gr.;
- mashed potatoes - 220 gr.;
- jelly - 220 gr.;
- biscuits - up to 5 pieces.
20:00 - dinner:
- kefir - 300 gr.;
- baked apples - 2 pieces;
- casserole or curd pudding - 220 gr.
Twice a week in the diet, for lunch, meat dishes should be replaced with boiled fish. The amount of food consumed can be varied within certain limits, taking into account a person’s weight, his daily physical activity and lifestyle. Also, you should not take various protein products at one time (for example, dairy and meat or dairy and fish) - this can lead to increased gas formation in the intestines and bloating.

Postoperative diarrhea
Opinions about the reasons for its appearance vary; most experts assign the leading role to the absence of the reservoir function of the gallbladder. With insufficient reabsorption of constantly incoming bile, it enters the large intestine in larger quantities than usual, which provokes diarrhea. It must be said that with cholelithiasis, the function of the bladder is already impaired, and some patients complain of diarrhea even before surgery.

There are very different data on the frequency of this symptom, from 1 to 35%. Most studies say 10-15%. In my practice it is much lower, but the reliability of personal observations is known to be low. In addition to following a diet (it is very important to eat a little several times a day), bile acid sequestrants (cholestyramine) will help cope with diarrhea; sometimes it is necessary to prescribe loperamide. In the vast majority of cases, diarrhea goes away quite quickly.
There is an opinion, confirmed by experimental studies, that with the sphincter apparatus preserved, the common bile duct partially compensates for the reservoir function of the gallbladder for several months.
Requirements for preparing for the procedure
A surgical intervention of this nature requires special preparation of the patient.
2 weeks before the date of surgery, you must pass a whole list of tests:
- general blood analysis;
- coagulogram;
- blood biochemistry;
- analysis to determine the Rh factor and blood group;
- for women - a smear on the vaginal flora;
- PCR for HIV, syphilis, hepatitis A, B, C.
In addition, the doctor who will perform the operation will definitely require electrocardiography results.
All tests should be within normal limits. If any indicators are abnormal, the operation cannot be performed until the patient undergoes a course of treatment. If repeated tests show normal values, then the patient can be allowed to proceed to the next stages of preparation.
A person should inform the doctor about all chronic diseases he has, especially diseases of the respiratory organs, endocrine and digestive systems. Taking any medications 2-3 weeks before the scheduled surgery must be agreed with the surgeon. 10 days before the appointed date, stop using vitamin E, anticoagulants, and Aspirin.
On the day before surgery, after 18:00 it is forbidden to eat, and after 22:00 - to drink liquid. For 3-4 days before the procedure, you should avoid fatty, fried, hot and spicy foods, smoked meats and pickles. Before going to bed, you need to do a cleansing enema, and repeat the procedure in the morning.
The operation is performed strictly on an empty stomach, so eating breakfast or drinking liquids in the morning is prohibited.
Before the procedure begins, the surgeon tells the patient in general terms how laparoscopy will proceed and how long the operation will last. On average, removing stones takes from 40 minutes to an hour, removing a bladder takes 1.5-2 hours.