Review
The bacterium Escherichia coli (E. coli), which produces Shiga toxin, is often found in the intestines of humans and warm-blooded animals.
Most strains of E. coli are harmless. However, some strains, such as enterohemorrhagic E. coli (STEC), can cause severe foodborne illness. This bacterium is transmitted to humans primarily through consumption of contaminated foods, such as raw or undercooked ground meats, raw milk, and contaminated raw vegetables and sprouts. STEC produces toxins known as Shiga toxins, so named because of their similarity to toxins produced by Shigella dysenteriae. The number of STEC bacteria can increase at temperatures between 7°C and 50°C (optimal temperature 37°C). Some STEC bacteria can grow in acidic foods with a pH as low as 4.4, as well as in foods with a minimum water activity (aw) of 0.95.
Bacteria are killed when food is thoroughly cooked until all parts of the food reach a temperature of 70°C or higher. The STEC serotype of most public health concern is E. Coli O157:H7; however, other serotypes are often the causative agents of sporadic cases and outbreaks.
Symptoms
Symptoms of illnesses caused by STEC bacteria include abdominal cramps and diarrhea, which in some cases may progress to bloody diarrhea (hemorrhagic colitis). Fever and vomiting are also possible. The incubation period lasts from 3 to 8 days, with an average duration of 3-4 days. Most patients recover within 10 days, but in a small number of patients (especially young children and older adults), the infection can lead to life-threatening disease called hemolytic uremic syndrome (HUS). HUS is characterized by acute kidney failure, hemolytic anemia, and thrombocytopenia (low platelet levels in the blood).
People suffering from bloody diarrhea or severe abdominal cramps should seek medical attention. Antibiotics are not part of the treatment for patients with STEC disease and may increase the risk of developing HUS.
It is estimated that HUS may develop in 10% of patients with STEC infection, and the case fatality rate is 3 to 5%. Worldwide, HUS is the most common cause of acute renal failure in young children. It can lead to neurological complications (such as convulsions, stroke and coma) in 25% of patients and chronic kidney disease, usually mild, in about 50% of surviving patients.
Diagnostics
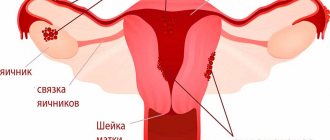
The therapeutic intervention regimen is determined after receiving the results of a smear taken from the cervix. In order for the examination result to be accurate, it is important to comply with the following conditions:
- one day before the examination, exclude sexual intercourse;
- stop using vaginal tablets and suppositories for 2-3 days;
- On the day of the smear test, carry out the hygienic procedure without using soap or any cosmetic chemicals.
A smear for Escherichia is considered positive when E. coli is detected in the cervical canal, provided that a trend towards a decrease in the number of lactobacilli is detected.
Sources and transmission of infection
The information available on STEC relates mainly to the O157:H7 serotype, since from a biochemical point of view it can be easily differentiated from other E. coli strains. The reservoir of this pathogenic microorganism is mainly cattle. In addition, other ruminants (such as sheep, goats and deer) are considered significant reservoirs, and other infected mammals (such as pigs, horses, rabbits, dogs, cats) and birds (such as chickens and turkeys) are also found to be infected.
E. coli O157:H7 is transmitted to humans primarily through consumption of contaminated foods, such as raw or undercooked ground meats and raw milk. Fecal contamination of water and other food products, as well as cross-contamination during food preparation (through beef and other meat products, contaminated work surfaces and kitchen utensils) can also lead to infection. Examples of foods implicated in outbreaks of E. coli O157:H7 include undercooked hamburgers, smoked salami, unpasteurized fresh apple juice, yogurt, and cheese made from raw milk.
An increasing number of outbreaks are associated with the consumption of fruits and vegetables (including sprouts, spinach, lettuce, cabbage and lettuce), which may be contaminated through contact with feces from domestic or wild animals at some stage in their cultivation or processing. STEC bacteria are also found in bodies of water (such as ponds and rivers), wells, and livestock water troughs. They can remain viable for several months in manure and sediment at the bottom of drinking troughs. Transmission of infection through both contaminated drinking water and water for recreational use has also been reported.
Close contacts of people are one of the main routes of transmission of infection (oral-fecal route of infection). Asymptomatic carriers have been reported, that is, individuals who do not show clinical symptoms of the disease but are capable of infecting other people. The shedding period for STEC bacteria in adults is approximately one week or less, but in children the period may be longer. Visiting farms and other places where farm animals are kept where direct contact with them is possible is also a significant risk factor for STEC infection.
Prevention
To prevent infection, control measures must be followed at all stages of the food chain, from agricultural production on farms to food processing, processing and preparation in both commercial establishments and at home.
In industrial settings
The incidence of disease can be reduced through the implementation of a variety of risk reduction strategies for ground meat (e.g. screening of animals prior to slaughter to prevent the introduction of large numbers of pathogens into slaughter areas). Good slaughter practices and hygiene reduce fecal contamination of carcasses, but do not guarantee the absence of STEC bacteria in the product. To minimize microbiological contamination, it is essential to provide food hygiene training to workers in farms, slaughterhouses and food processing plants. The only effective way to kill STEC bacteria in food is through a bactericidal treatment such as heat (such as cooking or pasteurization) or irradiation.
At home
Measures to prevent E. coli O157:H7 infection are similar to those recommended for the prevention of other foodborne illnesses. The basic good food hygiene practices outlined in the WHO Five Principles for Making Food Safer can help prevent the transmission of pathogens that cause many foodborne illnesses, as well as protect against foodborne illnesses caused by STEC.
The five essential principles for achieving safer food are:
- Five Essential Principles of Safe Food
These recommendations must be followed in all cases, especially the recommendation regarding “proper cooking of food”, whereby the core temperature of the food reaches at least 70°C. It is necessary to wash fruits and vegetables thoroughly, especially if they are eaten raw. If possible, vegetables and fruits should be peeled. Vulnerable populations (such as children and the elderly) should avoid consuming raw or undercooked meat products, raw milk, and products made with raw milk.
Regular hand washing is strongly recommended, particularly before preparing food, eating and after using the toilet, especially for people caring for young children, the elderly and people with weakened immune systems, as the bacteria can be transmitted not only through food, water and direct contact with animals, but also from person to person.
A number of STEC infections result from contact with recreational waters. Therefore, it is also important to protect such bodies of water, as well as sources of drinking water, from the entry of animal excrement into them.
Treatment
Treatment should be comprehensive:
- the patient should remain in bed and get more rest;
- it is important to normalize nutrition; your daily diet must include fermented milk products;
- use of vaginal and oral medications as prescribed by a gynecologist.
Most often, doctors prescribe Metronidazole and Clindamycin to women. After completion of therapy, a control smear of the vaginal contents is taken. This is necessary to assess the effectiveness of therapy. The exposure scheme is always determined on an individual basis, based on data obtained during testing. Self-treatment often causes the process to become chronic, the pathogen to enter the uterine cavity and the disease to become chronic.
Attention! Vaginal prebiotics and probiotics will help speed up the healing process.
Producers of fruits and vegetables
The WHO publication Five Keys to Growing Safer Fruits and Vegetables, aimed at farmers growing fresh fruits and vegetables for themselves, their families and for sale in local markets, provides basic practices for preventing microbial contamination of fresh produce during planting. cultivation, harvesting and storage.
The five most important principles for growing safer fruits and vegetables are:
- Maintain proper personal hygiene.
- Protecting fields from contamination by animal feces.
- Use of treated fecal waste.
- Assessing and managing risks associated with irrigation water use.
- Keeping equipment and premises for harvesting and storing crops clean and dry.
- Five Keys to Growing Safer Fruits and Vegetables
WHO activities
WHO is conducting scientific assessments to monitor foods for the presence of STEC. These assessments serve as the basis for international food standards, guidelines and recommendations developed by the Codex Alimentarius Commission.
In terms of prevention, WHO has developed a global strategy to reduce the burden of foodborne diseases. WHO has developed an advisory, Five Essentials for Safer Food. These five rules and associated training manuals provide country-specific materials that are easy to use, replicate, and adapt to different target audiences.
WHO helps strengthen food safety systems by promoting good production practices and educating retailers and consumers about proper food handling and preventing food contamination.
During E. coli outbreaks, such as those that occurred in Europe in 2011, WHO supports coordination of information exchange and collaboration through the International Health Regulations and the International Food Safety Authorities Network (INFOSAN) during all over the world; WHO works closely with national health authorities and international partners, providing technical assistance and providing the latest information on disease outbreaks.
- Outbreaks of E.coli infection in Europe
Escherichia - Escherichia coli - in the cervical canal
E. coli can normally be detected in stool cultures. We can talk about the development of pathology when it is detected in a smear of the vagina, cervical canal or urine culture. Most often, such a deviation from the norm indicates the development of a serious malfunction in the genitourinary and digestive systems. After determining the diagnosis, treatment must be started as soon as possible, otherwise the process may become chronic.
The danger lies in the resistance of Escherichia coli to various drugs, in particular to many antibiotics and compounds intended for the sanitation of the genital organs. Treatment of a lesion takes a long time, and achieving reliable results is not always possible.
Bacteria do not always pose a threat to the human body. Escherichia is directly involved in the formation of local immunity, therefore the disease is diagnosed when enterococci are detected in an atypical place in sufficient quantities. In such cases, pathological resistance of microorganisms to the immune response and a decrease in its activity are diagnosed.