The first signs of HIV in men and women, the main symptoms of HIV indicating infection
HIV is a virus that deprives the human body of protection by destroying the immune system. This disease became known in the 80s of the 20th century, when scientists found that an adult infected with HIV had weak immunity, like a newborn.
The disease is called AIDS - immune deficiency syndrome. The human immunodeficiency virus was officially announced in 1983. The disease is now so widespread that it has become an epidemic. Presumably, 50 million people in the world are currently carriers of the virus.
Story
In the summer of 1981, the US Centers for Disease Control published a report describing 5 cases of Pneumocystis pneumonia and 26 cases of Kaposi's sarcoma in previously healthy homosexual men from Los Angeles and New York.
Over the next few months, cases were reported among injecting drug users and, shortly thereafter, among blood transfusion recipients.
- In 1982, the diagnosis of AIDS was formulated, but the causes of its occurrence were not established.
- In 1983, HIV was first isolated from a cell culture of a sick person.
- In 1984, HIV was identified as the cause of AIDS.
- In 1985, a method for diagnosing HIV infection was developed using an enzyme-linked immunosorbent assay (ELISA), which detects antibodies to HIV in the blood.
- In 1987, the first case of HIV infection was registered in Russia - it was a homosexual man who worked as a translator in African countries.
When does HIV become AIDS?
The next stage of the disease is AIDS, immunity progressively decreases, the virus does not respond to medications, infections occur and malignant tumors arise. AIDS lasts no more than two years.
When HIV infection is detected, regular medical supervision is necessary to monitor the life process of the virus and promptly identify its resistance to drugs. Get help from an infectious disease specialist at the Center for Infectious Diseases at the international clinic Medica24 by calling. Anonymity is guaranteed.
The cause of HIV is infection with the immunodeficiency virus, which was discovered in 1982, but by that time there were already thousands of AIDS patients. Three years later, they found another variant of HIV, slightly different, since the symptoms of the disease were the same, they were simply called type 1 and type 2. Both agents belong to the family of lentiviruses, which live in animals for millions of years and do not cause disease, it is assumed that somewhere in West Africa, the first HIV was given to a person by a monkey a hundred years ago.
We will call you back, leave your phone number
Message sent!
expect a call, we will contact you shortly
Where did HIV come from?
In search of an answer to this question, many different theories have been proposed. No one can answer this for sure.
However, it is known that in the first studies of the epidemiology of HIV infection, it was found that the maximum prevalence of HIV was in the region of Central Africa. In addition, a virus capable of causing AIDS in humans has been isolated from the blood of the great apes (chimpanzees) living in this area, which may indicate the possibility of infection from these apes, perhaps through a bite or butchering of carcasses.
There is an assumption that HIV existed for a long time among the tribal settlements of Central Africa, and only in the twentieth century, as a result of increased population migration, it spread throughout the world.
Generalized lymphadenopathy
Generalized lymphadenopathy – enlargement of all groups of lymph nodes. This symptom appears most often during the stage of acute infection. It can be combined with other signs, or it can be independent. Lymph nodes enlarge in various diseases, so a patient who does not know his HIV status often does not attach importance to this.
A distinctive feature of generalized lymphadenopathy is its long course. The symptom persists for 1-3 months, is painless, more often the lymph nodes increase to a diameter of 1.5-2 cm. They are localized in one or more mobile and soft formations on the neck, behind the ears, in the armpits and subclavian cavities, in the groin.

Together with lymphadenopathy, the patient may experience:
- seborrhea;
- leukoplakia of the tongue;
- herpes simplex on mucous membranes and skin;
- polymorphic rashes;
- thrush of the oral cavity and genitals.
Symptomatic treatment during this period gives good results. Secondary diseases are treatable. With proper treatment, the patient feels satisfactory, can work, play sports, and have protected sex. The duration of this phase ranges from six months to 5 years. Although, depending on the patient’s lifestyle and the availability of treatment, this period can be either shortened or extended.
HIV and AIDS - what's the difference?
Fundamental differences between AIDS and HIV infection:
| HIV infection | a slowly manifesting viral infection that lasts for many years. All currently known methods of treating HIV infection do not lead to a complete cure. The disease affects the immune system, which protects the human body from the negative influences of the external environment. The virus, having entered the body from a carrier of the disease, may not manifest itself in any way for a long time, but within several years it destroys the immune system. |
| AIDS | a state of immunity in which the body is practically defenseless against harmful environmental influences and the development of oncological processes. Any infection that is harmless for a healthy person develops in a patient with AIDS into a serious illness with complications and subsequent death from complications, inflammation of the brain, or a malignant tumor. |
Further course of the pathology
Later, in patients with HIV infection, internal organs are affected by different types of bacteria, viruses and fungi. For example, pneumonia, secondary or complicated situations of herpes zoster are often observed. In later stages, when the immune system completely fails, severe immunodeficiency appears. At this stage, those infected develop the following severe infections:
- toxoplasmatosis,
- Neumocystis pneumonia,
- tuberculosis,
- extrapulmonary critococcal infection.
But if the disease is detected on time and treatment is started immediately, then a decline in the immune system and clinical manifestations may not appear. In this case, the woman’s immunity remains at the same level by suppressing the spread of the virus through medication. Therefore, the most correct approach is regular checks and the beginning of competent treatment. Thus, health and beauty will be preserved for a long time. It is also important to follow all the doctor’s recommendations, undergo examinations and tests several times a year.
Many people are interested in how long it takes for HIV to be detected ? To obtain the correct answer from the test, 3 months must pass from the date of infection. In rare situations, the manifestation of antibodies takes up to six months. And if after 3 months the result is negative, but you are sure that you are infected, then it is better to repeat it after six months.
It is important to realize that the appearance of HIV infection is not the end of life or death. There is no need to give up and do nothing. This is just a new stage at which you need to reconsider your everyday lifestyle and make every effort to prevent the disease from winning!
Statistics
Statistics on the number of people infected with HIV:
- Worldwide, as of December 1, 2016, the number of infected people was 36.7 million;
- In Russia, as of December 2021, there are about 800,000 people, with 90 thousand identified in 2015. In the same year, more than 25 thousand people died from AIDS in Russia, and over the entire observation period since 1987 - more than 200 thousand.
For CIS countries (data based on the results of 2015):
- Ukraine - about 410 thousand,
- Kazakhstan - about 20 thousand,
- Belarus - more than 30 thousand,
- Armenia - 4000,
- Tajikistan - 16400,
- Azerbaijan - 4171,
- Moldova - 17800,
- Georgia - 6600,
- Kyrgyzstan - about 10 thousand,
- Uzbekistan - about 33 thousand.
- Turkmenistan - officials claim that there are isolated cases of HIV infection in the country,
Since statistics record only officially detected cases, the actual picture is much worse. A huge number of people do not even suspect that they are HIV-infected and continue to infect others.

Manifestations of CNS damage
Damage to the nervous system, mainly the brain, is one of the main problems of HIV. CNS disorders are observed in 50-80% of patients, in 10% of them the symptoms are pronounced. There are several ways in which the peripheral and central nervous system can be affected by HIV infection. The first is the penetration of infected lymphocytes into the central nervous system, the second is the effect of secondary infections. Also in some cases, the development of brain tumors is possible.
The first signs of damage to the nervous system:
- headache;
- sleep disturbance (insomnia or drowsiness);
- tremor of the limbs;
- difficulty concentrating;
- memory impairment;
- behavioral changes.
As the disease progresses, signs of central nervous system damage become more obvious. A person experiences a change in behavior, fever, and convulsions. When the brain is damaged, vision deterioration and even blindness are also observed. At the final stages of disease progression, the patient may experience paralysis or paresis. Mental disorders can manifest themselves up to personality changes and dementia.

Some associated CNS diseases are treatable. However, the presence of such diseases complicates therapy in general and accelerates the onset of the terminal stage.
Symptoms and stages
The manifestation of symptoms of HIV infection in a man or woman depends on the stage of HIV development:
- Incubation period;
- Primary manifestations are acute infection, asymptomatic and generalized lymphadenopathy;
- Secondary manifestations are persistent lesions of internal organs, lesions of the skin and mucous membranes, generalized diseases;
- Terminal stage.
According to statistics, HIV infection is most often diagnosed at the stage of secondary manifestations and this is due to the fact that the symptoms of HIV become pronounced and begin to bother the patient during this period of the disease.
When do the first signs appear?
When infected, as well as during the intensive development of the infection, a person has no obvious signs. Once a pathogen enters the bloodstream, the immune system tries to protect the body. In the period from the first three weeks to three months, nonspecific symptoms may appear: chills, fever, cough, swollen lymph nodes. Rarely, these symptoms are accompanied by a skin rash. Such manifestations are very similar to a respiratory disease or allergy, so those infected often do not attach importance to these symptoms.
Content:
- When do the first signs appear?
- Main symptoms
- Signs at different stages
- Primary symptoms
- Secondary signs
- Generalized lymphadenopathy
- Manifestations of CNS damage
- What does an HIV-infected person look like?
- Symptoms in women
- Features of infection in men
- Children with HIV
- How to determine the immunodeficiency virus at home
Often the virus does not manifest itself at all for many years. On average, the first signs appear in the range from 3 months to 5 years after infection. And antibodies to the pathogen are detected 6-12 months after infection. Therefore, the main way to detect the presence of the virus is testing, which can be done free of charge.
Incubation period
After a person becomes infected with HIV, no symptoms or even small hints of the development of any pathology are observed for a long time. It is precisely this period that is called incubation; it can last, in accordance with the classification of V.I. Pokrovsky, from 3 weeks to 3 months.
No examinations or laboratory tests of biomaterials (serological, immunological, hematological tests) will help identify HIV infection, and the infected person himself does not look sick at all. But it is the incubation period, without any manifestations, that poses a particular danger - a person serves as a source of infection.
Some time after infection, the patient enters an acute phase of the disease - the clinical picture during this period may be a reason for questioning the diagnosis of HIV infection.
Primary prevention (preventive treatment) of secondary (opportunistic) infections
When the immune system is deeply damaged, it is important to prevent the development of diseases, the pathogens of which have the opportunity to parasitize in the body that finds itself without protection. Such diseases are called opportunistic, and pathogens are called opportunists from the Latin opportunus - opportunity. It is for this purpose that schemes for the prevention of opportunistic diseases were created for those patients whose immunodeficiency does not allow effective defense. These regimens involve taking medications used for treatment, but in doses that are lower than needed to fight an existing infection.
It is very important to take medications as prescribed by your doctor in accordance with the prescribed regimen. This can save lives, because against the background of a weakened immune system, such diseases can become fatal.
To prevent secondary infections, it is necessary to exclude their presence.
Prevention of Pneumocystis pneumonia and toxoplasmosis with CD4 count < 200 μl-1 (less than 15%) - it is recommended to take Co-trimoxazole according to the regimen until the CD4 + lymphocyte count increases during ART > 200 cells/μl for 3 months.
Prevention of fungal diseases, incl. candidiasis - antifungal drugs as prescribed by a doctor.
Prevention of non-tuberculous mycobacteriosis - azithromycin or clarithromycin according to the regimen.
Prevention of tuberculosis - isoniazid according to the regimen (or another drug combined in ART).
The dosage of drugs and the course of treatment depend on the degree of immunodeficiency and the severity of the patient’s condition.
Stage of primary manifestations
Active reproduction of the virus continues, but the body is already beginning to respond to the introduction of HIV. This phase lasts about 3 months.
It can occur in three ways:
- Asymptomatic – there are no signs of the disease, but antibodies to HIV are detected in the blood.
- Acute HIV infection - this is where the first symptoms of HIV infection appear, accompanied by an unmotivated rise in body temperature to subfebrile levels, increased fatigue, increased sweating, various rashes on the skin and mucous membranes, enlarged lymph nodes (usually posterior cervical, axillary, elbow), Some people may experience sore throat, diarrhea, and an enlarged spleen and liver. Blood test - decreased lymphocytes, leukocytes, thrombocytopenia. This period lasts on average from 2 weeks to 1.5 months, then passes into the latent stage.
- Acute HIV infection with secondary diseases - sometimes in the acute phase the suppression of immunity is so strong that already at this stage HIV-associated infections (pneumonia, herpes, fungal infections, etc.) may appear.
Clinic of the initial period of the disease
Infection with the immunodeficiency virus usually occurs unnoticed. The incubation period is long
- several weeks, months, sometimes years. Therefore, when HIV symptoms appear, a woman does not associate them with unprotected sex, surgery or injections. The first signs of the disease differ depending on the progression of the process:
Acute fever phase
At this stage, the patient is given a variety of diagnoses: infectious mononucleosis, gastroenteritis, meningitis, pneumonia... But most often the disease is hidden under the guise of influenza. A comparative analysis of influenza and HIV in women in the early stages shows the following differences:
Mycoplasmosis belongs to infectious pathologies. It can occur in any person, regardless of gender or age. And yet, the majority of cases of infection occur in young people, because the route of infection is predominantly sexual. Read more in the article: “mycoplasmosis symptoms and treatment.”
| Symptom | Flu | HIV (initial stage) |
| Catarrhal phenomena (cough, runny nose) | From the third day, pronounced (dry prolonged cough, nasal congestion, runny nose) | They are very weakly expressed, exist for a long time, and do not respond to traditional methods of treatment. |
| Fever | A sharp increase in body temperature and high numbers lasting no more than 3-5 days (in an uncomplicated form) | The temperature lasts 2-3 weeks within the subfebrile range (37-38 ° C) |
| Sweating | An unusual symptom for influenza | Expressed over a long period of time |
| Enlarged liver and spleen | Absent | Often |
| Presence of a rash | Happens very rarely | Characteristic rashes like measles or rubella |
| Enlarged lymph nodes | Rarely | Often |
Another “mask” of HIV infection at the initial stage is infectious mononucleosis. Inflammation of the tonsils comes to the fore.
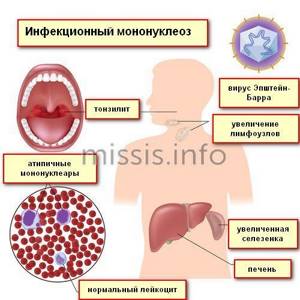
Sore throats recur several times a year, accompanied by enlarged cervical lymph nodes and prolonged low-grade fever. Women feel pain or discomfort in the right hypochondrium, the liver and spleen are enlarged.
Prolonged fever (more than 2 weeks) is a direct route to a doctor for a comprehensive laboratory examination.
Differentiate
These diseases can only be diagnosed in a laboratory way. Therefore, whenever there are external manifestations of infectious mononucleosis, patients are prescribed tests for HIV infection.
Other symptoms of this phase include:
- persistent diarrhea, which, unlike intestinal infections, is not relieved by traditional medications;
- general weakness, which is usually attributed to overwork or chronic fatigue syndrome in women;

- headache;
- symptoms of esophagitis (inflammation of the mucous membrane of the esophagus) - a “lump” in the throat when swallowing, pain along the esophagus;
- irritability, sleep inversion (drowsiness during the day and insomnia at night).
The characteristics of the female body explain the presence of specific “female” symptoms: painful periods, enlargement of the inguinal lymph nodes, heavy discharge, pain in the pelvic area. Of course, they cannot be called specific. But the repetition of these symptoms from cycle to cycle should be alarming.
A timely visit to a gynecologist, even with minor problems, will help diagnose HIV in women at the very beginning of the disease.
Psychoneurological symptoms (consequences of female emotionality):
- anxiety and depression;
- loss of coordination, dizziness, unsteady gait;
- pseudo epileptic seizures;
- memory loss, emotional poverty, inappropriate behavior.
Women are more likely to have lipodystrophy
- redistribution of fat in the body. At the same time, the breasts become enlarged and fatty tissue accumulates in the abdominal cavity.
Cytological examination of cervical cells is of great diagnostic importance. This is the easiest and fastest way to detect a number of pathologies at an early stage. Read more in the article: “cytological examination of a cervical smear.”

Asymptomatic phase
After the nonspecific manifestations of the fever phase, a period of calm begins. All manifestations disappear, the woman feels good and temporarily forgets about her health problems. This stage can last several years.
[media=
https://youtu.be/h7UuJu055f8
]
Generalized lymphadenopathy phase
Enlarged lymph nodes
various groups against the background of “absolute health”.
At first, the nodes are soft, small in size (up to 3 mm), then they become denser and increase to 5 cm in diameter. Other symptoms of this phase are:
- sweating;
- enlarged liver and spleen;
- increase in body temperature.
Additional symptoms force the patient to look for the cause of the disease and consult a doctor. But often lymphadenopathy is isolated, and the woman does not pay attention to it or tries to cope with it at home. Precious time is lost here too.
Acute infection
The most common first manifestation of HIV infection is symptoms resembling infectious mononucleosis. A person’s temperature rises to 38˚C or higher for no apparent reason, inflammation of the tonsils (tonsillitis) appears, and the lymph nodes become inflamed (usually the cervical ones). The cause of the increase in temperature often cannot be determined; it does not decrease after taking antipyretics and antibiotics. At the same time, severe weakness, fatigue, and profuse sweating appear, mainly at night. The patient suffers from headache, loss of appetite, and disturbed sleep.
- When examining the patient, one can determine an enlargement of the liver and spleen, which is accompanied by complaints of heaviness in the hypochondrium and aching pain there. A small maculopapular rash appears on the skin in the form of small pale pink spots, sometimes merging into larger formations. Long-term intestinal upset appears in the form of frequent loose stools.
- In blood tests with this variant of the onset of the disease, an increased level of leukocytes, lymphocytes is determined, and atypical mononuclear cells are detected. This variant of the first symptoms of HIV infection is observed in 30% of patients.
- In other cases, acute infection may manifest as serous meningitis or encephalitis. These conditions are characterized by intense headache, often nausea and vomiting, and increased body temperature. Sometimes the first symptom of HIV infection is inflammation of the esophagus - esophagitis, accompanied by chest pain and difficulty swallowing.
Other nonspecific symptoms of the disease, as well as an asymptomatic course, are also possible. The duration of this stage ranges from several days to 2 months, after which all signs of the disease disappear again. Antibodies to HIV may also not be detected at this stage.

HIV
Herpes
14248 04 September
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. HIV: causes, symptoms, diagnosis and treatment methods.
Definition
HIV (human immunodeficiency virus) is an infectious chronic disease, transmitted by contact, slowly progressing and characterized by damage to the immune system with the development of acquired immunodeficiency syndrome (AIDS). AIDS is the final stage of HIV infection, when due to a weakened immune system a person becomes defenseless against any infections and some types of cancer. The danger is posed by so-called opportunistic infections - diseases caused by opportunistic or non-pathogenic flora: viruses, bacteria, fungi, which in healthy people do not lead to serious consequences or occur easily and are cured on their own. With AIDS, they overlap each other, have a protracted course, are difficult to treat and can cause death.
Causes of HIV
The source of infection is a person infected with HIV at any stage of the disease. The virus is transmitted through blood, semen, vaginal secretions, and breast milk.
Sexual intercourse (unprotected sex with an infected partner) is the dominant factor in the spread of HIV infection.
Transmission of HIV from mother to child can occur at any stage of pregnancy (through the placenta), during childbirth (when passing through the birth canal) and breastfeeding (in the presence of ulcers, cracks on the mother’s nipples and in the child’s mouth).
A high risk of infection exists when intravenously administering narcotic substances with non-sterile syringes, when transfusing HIV-infected blood and its preparations, and using medical and non-medical instruments contaminated with biological fluids of a person infected with HIV. In addition, donor organs and tissues used for transplantation can pose a danger.

Once in the bloodstream, the virus penetrates helper T-lymphocytes, or CD-4 cells (a type of white blood cell), which help the body fight infections. Helper T cells have so-called CD4 receptors on their surface. HIV binds to these receptors, enters the cell, multiplies within it and ultimately destroys it. Over time, the viral load increases and the number of T helper cells decreases.
If left untreated, AIDS-related conditions and symptoms appear after several years due to a significant decrease in the number of T-helper cells.
Classification of the disease
- The incubation stage is from the moment of infection until the body reacts in the form of clinical manifestations of acute infection and/or the production of antibodies (specific proteins produced in response to the penetration of an antigen, in this case a virus).
- Stage of primary manifestations of clinical symptoms:
a) asymptomatic (no symptoms, antibodies are produced); b) acute HIV infection without secondary diseases: there is an increase in lymph nodes, fever, pharyngitis, rashes on the skin and mucous membranes, less often - enlargement of the liver, spleen, diarrhea; c) acute HIV infection with secondary diseases (sore throat, bacterial pneumonia, candidiasis, herpetic infection, etc.). These manifestations, as a rule, are mild, short-lived, and amenable to therapy. - Subclinical stage - the only clinical manifestation of the disease is enlarged lymph nodes.
- Stage of secondary diseases:
a) loss of body weight less than 10%, fungal, viral, bacterial lesions of the skin and mucous membranes, repeated pharyngitis, sinusitis, shingles; b) loss of body weight more than 10%, diarrhea or fever for more than a month, repeated persistent viral, bacterial, fungal, protozoal (caused by protozoa) lesions of internal organs, localized Kaposi's sarcoma (multiple malignant neoplasms on the skin and mucous membranes), repeated or generalized (by whole body) herpes zoster; c) cachexia (exhaustion), generalized viral, bacterial, fungal, protozoal, parasitic diseases, Pneumocystis pneumonia, tuberculosis, malignant tumors, lesions of the central nervous system. - Terminal stage - existing secondary diseases become irreversible, death occurs within several months after their development.
Symptoms of HIV/AIDS
After an incubation period of several days to several weeks, most infected people develop an acute illness with flu-like symptoms (fever, aches, general weakness, lack of appetite, headache, sore throat, swollen lymph nodes, skin rashes) . Weight loss and the formation of ulcers on the oral mucosa are possible. This phase usually lasts 7-10 days. Due to the nonspecific nature of its manifestations, the diagnosis of HIV is rarely made. Rarely, opportunistic infections are recorded at this stage of the disease. There is a cough with sputum, chest pain (with the development of pneumonia), painful blistering rashes on the skin (with herpes zoster). As a rule, health quickly returns to normal without specific HIV treatment.

After this stage, a temporary equilibrium is established between the infectious process and the antiviral immunity that restrains its development.
For a long time (8-10 years or more), the infection occurs asymptomatically or with persistent generalized lymphadenopathy - an increase in at least two groups of lymph nodes that persists for at least 3 months.
Subsequently, active reproduction of the virus and destruction of T-lymphocytes continue, a stage of secondary changes develops, which is characterized by progressive weight loss, general weakness, persistent fever, chills, and severe sweating. Clinical manifestations of opportunistic diseases determine the clinical picture of this stage: patients are bothered by cough and shortness of breath, nausea, vomiting, abdominal pain, severe diarrhea, skin rashes, severe headaches, decreased memory and attention, etc.
HIV diagnosis
Laboratory research methods:
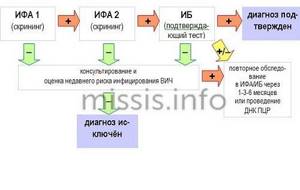
- HIV screening.
- An examination confirming the fact of HIV infection (in case of positive or questionable screening results).
- Measuring and monitoring the amount of virus in a person’s blood - determining the viral load in persons with an established diagnosis of HIV.
- Determination of immune status in patients with HIV infection.
Screening (examination of healthy people) for HIV should be carried out on any person who believes that they may be infected, as well as before any hospitalization and surgery, all pregnant women and their sexual partners.
The examination is advisable for people at high risk of contracting HIV, for example, in the presence of diseases that have the same transmission mechanism as HIV infection (viral hepatitis B and C, sexually transmitted diseases), people who have regular unprotected sexual intercourse, injection drug addicts, children , those born to mothers with HIV infection, medical workers who have direct contact with blood at work, etc.
There are rapid HIV screening tests that can be done at home. To determine specific antibodies/antigens to HIV (HIV-1, 2, p24 antigen), blood, saliva or urine are used. The accuracy of any rapid test is lower than a test performed in a laboratory.
For a standard screening examination, antibodies to HIV 1 and 2 and HIV 1 and 2 antigen (HIV Ag/Ab Combo) are determined in the blood using an enzyme-linked immunosorbent assay (ELISA).
Latent stage of HIV
It lasts up to 2-20 years or more. Immunodeficiency progresses slowly, the symptoms of HIV are expressed by lymphadenitis - enlarged lymph nodes. They are elastic and painless, mobile, the skin retains its normal color. When diagnosing latent HIV infection, the number of enlarged nodes is taken into account - at least two, and their location - at least 2 groups not connected by a common lymph flow (with the exception of inguinal nodes).
Lymph moves in the same direction as venous blood, from the periphery to the heart. If 2 lymph nodes are enlarged in the head and neck area, then this is not considered a sign of the latent stage of HIV. A combined increase in groups of nodes located in the upper and lower parts of the body, plus a progressive decrease in the number of T-lymphocytes (helper cells) testify in favor of HIV.
Signs at different stages

The infection develops in stages. As the number of viral particles increases, more and more cells of the immune system are involved in the process, an adequate immune response is blocked, and inflammatory, autoimmune, and oncological changes develop. The use of antiretroviral therapy slows down the progression of the disease, prolonging the life of patients. The HIV clinic at different stages is characterized by its own characteristics. Symptoms are varied and gradually increase with a decrease in the number of active immune cells.
Incubation period
According to the classification of V.V. Pokrovsky, the first stage of infection is called incubation. This is the period of time from the pathogen entering the body until the appearance of antibodies in the blood or primary symptoms. On average, this stage lasts 3-12 weeks. As a rule, there are no obvious symptoms. The person looks healthy and feels good. In rare cases, symptoms of ARVI are possible. Tests for HIV infection during this period are negative, so you need to repeat the examination after 3 and 6 months. Once antibodies appear, symptoms may also not be observed for many years. When antibodies are already present in the blood, and there are no manifestations of infection, the next stage begins - latent.
Asymptomatic period
This is the longest phase of the disease; a person can be a carrier of the pathogen for 5-15 years. If the patient leads a healthy lifestyle, the asymptomatic period may last even longer. In patients with bad habits and a low standard of living, the latent course quickly passes into the acute phase.
Also, the duration of incubation and asymptomatic course depends on:
- patient's age;
- infectious dose;
- immune status of the patient;
- routes of infection.
For example, with blood transfusion, the incubation and asymptomatic periods pass faster than with sexual transmission. The virus continues to multiply during the latent phase, but the immune system is still able to suppress infections. The virus does not manifest itself clinically and can only be determined through laboratory testing.
Stage of secondary diseases or AIDS
The number of lymphocytes decreases so much that infections that otherwise would never have arisen begin to cling to a person. These diseases are called AIDS-associated infections:
- Kaposi's sarcoma;
- brain lymphoma;
- candidiasis of the esophagus, bronchi or lungs;
- cytomegalovirus infections;
- Pneumocystis pneumonia;
- pulmonary and extrapulmonary tuberculosis, etc.
Actually this list is long. In 1987, a WHO expert committee compiled a list of 23 diseases that are considered markers of AIDS, and the presence of the first 12 does not require immunological confirmation of the presence of the virus in the body.
See also: seminars and webinars about AIDS/HIV.
Main symptoms
Typical signs of HIV infection are a set of symptoms of secondary diseases, that is, those diseases that a weakened immune system is not able to fight. Classic manifestations include symptoms of fungal infection of the mucous membranes, aphthous stomatitis, polylymphoadenopathy, various manifestations of herpes virus infection, Pneumocystis pneumonia, infiltrative tuberculosis, digestive disorders, rashes, central nervous system damage and others. Along with them, symptoms of infection appear that resemble a respiratory disease. The main sign by which HIV can be suspected is generalized lymphadenopathy and pancytopenia.
The occurrence of episodes of fever, diarrhea, and mucosal lesions should alert you. The further the infection progresses, the greater the range of symptoms may become.
Features of the first signs of HIV infection in women
Women are much more likely than men to experience secondary manifestations such as herpes, cytomegalovirus infection and vaginal candidiasis, as well as candidal esophagitis.
In addition, at the stage of secondary manifestations, the first signs of the disease may be menstrual irregularities, inflammatory diseases of the pelvic organs, and most often acute salpingitis. Diseases of the cervix, such as carcinoma or dysplasia, may occur.

Secondary signs
Based on secondary manifestations of infection, doctors may suspect HIV. However, even these manifestations can initially be considered as an independent disease.
Testing for the immunodeficiency virus is mandatory for the following secondary symptoms:
- Pneumonia. The patient develops a dry, prolonged cough, low-grade fever (increased body temperature no higher than 38° for a long time). Over time, the cough turns into a wet one, you feel a general malaise, weakness, and sweating. The use of classical antibiotics does not give a positive result.
- Generalized infections are a combination of bacterial, fungal and viral diseases. Most often these include: tuberculosis, oral, genital and visceral candidiasis, infections caused by cytomegalovirus and Epstein-Barr virus, common and herpes zoster, viral gastroenteritis. Against the background of immunodeficiency, these diseases are especially difficult.
- Kaposi's sarcoma is a neoplasm in the lymphatic system. It looks like a single tumor or a cluster of formations, and is most often localized on the torso, neck, mouth and head. Sometimes sarcoma has a cherry tint to the skin, but it can also be without any color change.
- Intoxication syndrome. About half of the patients experience the following symptoms: nausea, muscle and joint pain, diarrhea, night sweats, severe weakness, headache, increased irritability.
In addition to these symptoms, the patient sometimes experiences worsening chronic diseases. Secondary diseases and symptoms can occur one after another or together. The moment of onset and duration depend on the adequacy of therapy, the age of the patient, bad habits and other factors. On average, each symptom lasts 1-2 weeks. Cough and diarrhea may not go away for 1-2 months.
What to do if you had unprotected sexual intercourse?
There are a number of medications that are used for post-exposure prophylaxis for HIV. Unfortunately, they are not available for sale, so you will have to go to an appointment with a therapist and explain the situation. There is no guarantee that such measures will 100% prevent the development of HIV infection, but experts say that taking such medications is quite advisable - the risk of developing the human immunodeficiency virus is reduced by 70-75%.
If there is no opportunity (or courage) to consult a doctor with a similar problem, then there is only one thing left to do - wait. You will need to wait 3 months, then undergo an HIV test, and even if the result is negative, you should take a control test after another 3 months.
How long after infection does HIV appear?
The human immunodeficiency virus circulates in all human tissues, secretions and secretions. Therefore, infection occurs through blood transfusion of a patient, tissue transplantation, from a pregnant woman to the fetus through a single blood supply system, or through close contact of blood, saliva, sperm of an infected person with damaged skin or mucous membrane of a healthy person. Risk groups include anyone who comes into contact with the secretions and blood of an infected person.
As expected, the invading enemy is captured by the immune defender - the monocyte, for one reason - this is its job - to cleanse the blood. The monocyte is about to digest the enemy agent into its constituent atoms. And this is all the virus needs; it devours the cell from the inside, divides and is thrown out of the cellular remains with newborn comrades in order to penetrate into a new cell. So HIV wanders for two to four weeks, breeding and multiplying, so that by the end of the month it manifests itself in the form of a disease.
Early detection of HIV infection allows you to break the chain of transmission of the virus. An HIV test must be done every year; in most cases it is impossible to determine the time and source of infection.
Some facts on the methods and causes of infection of Russians
- Of the nearly one million infected Russians, the largest group is 30-40 year olds, 47 out of every hundred.
- Out of every ten HIV-infected people of all ages, six are caused by a dirty syringe.
- Infection from medical procedures occurs on average five times a year, and the main cause is the transfusion of untested donor blood.
- Among infected Russians, only 1.2% are homosexuals; in foreign countries, members of the LGBT community make up 42%.
- A national peculiarity is that 40% of those infected are respectable women who are in a civil marriage with men who arrived from neighboring countries.
- 80% of women find out about their positive HIV status when they go to an antenatal clinic due to the desired pregnancy from their beloved man.
- A third of HIV carriers also have the hepatitis virus, and every twentieth has tuberculosis.
At the international clinic Medica24, an individual approach is applied to each patient based on clinical recommendations from the world's leading medical centers, which allows for optimal results to be achieved in a short time.
We will call you back, leave your phone number
Message sent!
expect a call, we will contact you shortly
Can you get infected through oral sex?
The risk of contracting HIV infection through oral sex is minimized. The fact is that the virus does not survive in the environment, so in order to be infected orally, two conditions must come together: there are wounds/abrasions on the partner’s penis and wounds/abrasions in the partner’s mouth. But even these circumstances do not in every case lead to HIV infection.
For your own peace of mind, you need to take a specific HIV test 3 months after dangerous contact and undergo a “control” examination after another 3 months.
Who is at risk of contracting HIV?
The infection is transmitted by the immunodeficiency virus with contaminated blood; it cannot be acquired through normal contact or even a kiss. You can become infected by using medical or hairdressing equipment contaminated with the blood of a patient, only by biological fluids in which formed blood elements float. Traditional risk groups that come into contact with the blood of patients and have a chance of infection: drug addicts, sex workers, promiscuous people, doctors.
HIV tests
The most common method for diagnosing HIV is an enzyme-linked immunosorbent assay (ELISA or ELISA test), which detects specific antibodies to the immunodeficiency virus. Antibodies to HIV are formed between three weeks and 3 months after infection and are detected in 95% of cases. After six months, HIV antibodies are found in 9% of patients, later - only in 0.5-1%.
Blood serum taken from a vein is used as a biomaterial. You can get a false-positive ELISA result if HIV infection is accompanied by autoimmune (lupus, rheumatoid arthritis), cancer or chronic infectious diseases (tuberculosis, syphilis). A false negative response occurs during the so-called period. seronegative window, when antibodies have not yet appeared in the blood. In this case, to control HIV, you need to donate blood again, after a pause of 1 to 3 months.
If the ELISA is assessed as positive, the HIV test is duplicated using PCR, polymerase chain reaction, determining the presence of viral RNA in the blood. The technique is highly sensitive and specific and does not depend on the presence of antibodies to the immunodeficiency virus. Immunoblotting is also used, which makes it possible to detect antibodies to HIV protein particles with precise molecular weights (41, 120 and 160 thousand). Their identification gives the right to make a final diagnosis without confirmation by additional methods.

Red ribbon - a symbol of the fight against AIDS in women's palms
Laboratory detection of HIV infection in the early stages
Clinically, it is often impossible to determine how HIV manifests itself in women; the first signs are usually visible in laboratory tests.
The importance of early HIV diagnosis:
- timely treatment significantly improves life expectancy;
- early prevention at the source of infection reduces the risk of unintentional transmission of the virus to a healthy environment;
- better results in social adaptation and effective psychological assistance to people infected with HIV.
The modern approach to the early diagnosis of HIV infection includes a symptom complex, the presence of which always requires the appointment of laboratory tests to exclude this disease
:
- fatigue that cannot be explained by other reasons;
- sweating, especially at night;
- prolonged diarrhea syndrome;
- headache;
- frequent tonsillitis;
- recurrent inflammatory diseases of the respiratory system;
- weight loss without dieting in a short time (at an early stage by less than 10%);
- furunculosis and various skin rashes (papules, roseola, spots, pustules);

- lymphadenopathy, especially generalized, with the exception of inguinal lymph nodes;
- herpes zoster at a young age.
Laboratory diagnosis of HIV infection in women is carried out in three areas:
| Directions | Types of laboratory tests |
| Isolation of human immunodeficiency virus antigens | Polymerase chain reaction (PCR), virus cultivation. |
| Determination of specific antibodies | Antibodies are detected by ELISA (enzyme-linked immunosorbent assay) or IB (immunoblotting). The latter is most informative in the early stages of infection. In the structure of the virus, there are a number of proteins with pronounced immunological activity, to which antibodies are primarily produced. In the early stages of the disease, these are proteins p17 and p24. |
| Identifying accompanying changes in the immune system | Determination of CD4+ lymphocytes in the blood. This is the main criterion for diagnosing HIV in everyday life. If the rate is below 200 cells per mm?, the disease is considered confirmed. |
The difficulties of laboratory diagnosis in the early stages of HIV lie in obtaining false-positive test results, especially by ELISA. This most often occurs in patients with autoimmune diseases and Epstein-Bar infection. The percentage of false positive reactions varies from 0.02 to 0.5% of cases. Behind such “mistakes” are the broken destinies of people and incorrectly prescribed treatment.
Laboratory diagnostic algorithm
To definitively confirm HIV infection in women, laboratory diagnostics are carried out in stages:
- Stage of screening study using ELISA. Due to its relatively low cost, it allows for mass examination.
- Stage of reference research using ELISA. It is carried out in case of positive and false-positive results at the first stage.

- Stage of expert research using IB, PCR, RIP (radioimmunoprecipitation), determination of reverse transcriptase activity, virus cultivation. If at this stage the results of the listed methods are negative, then the suspicion of HIV is removed. Only positive tests at this stage provide grounds for a final diagnosis of HIV infection.
Treatment of infection
Of the 35 million people living with HIV, some remain alive thanks to antiretroviral therapy. In the absence of antiretroviral therapy for HIV infection, death occurs on average 9-11 years after infection.
- With antiretroviral therapy, the patient's life expectancy is 70-80 years. Antiretroviral drugs prevent HIV from multiplying in the cells of the human immune system, blocking the introduction of virions into cells and disrupting the process of assembly of new virions at various stages. Timely treatment with antiretroviral drugs reduces the risk of developing AIDS and subsequent death by hundreds of times. Antiretroviral drugs cause side effects in some patients, in some cases even requiring a change in the treatment regimen (the set of medications taken).
- Therapy is prescribed when immunity is reduced and/or the viral load is high. If the number of CD4+ lymphocytes is high and the viral load is low, therapy is not prescribed. After prescribing therapy, medications must be taken daily at the same time and for life, which creates inconvenience for patients. You should also take into account the high cost of a monthly course of medications. In 2014, less than half of the 9.5 million people who needed antiviral therapy received the necessary medications. Also, all pregnant women with acute HIV infection should begin immediate HAART to prevent transmission of HIV to the fetus.
According to WHO recommendations, HAART should be started immediately in all HIV-infected children under one and a half years of age[66]. Initiating therapy within 3 months of birth in infants who acquire HIV from their mother reduces mortality by 75%. Without treatment, a third of HIV-infected children die within the first year of life and 50% during the second year. If HIV diagnosis is not possible, treatment should begin at 9 months of age, or earlier if symptoms appear.
As of February 2021, it was announced that a group of German scientists had succeeded in completely removing a type of HIV-1 from living cells. Tests were carried out on human cells implanted into experimental mice. Human trials should be carried out soon.
How is HIV transmission from mother to child prevented?
An infected woman can give birth to a healthy child; there is no clear understanding of the mechanism of infection, just as there is no clear knowledge of the principles of life of viruses. The risk of transmission to the fetus developing in the mother's womb increases in the acute stage of infection and when more than 10 thousand viral copies are detected. It is dangerous when a pregnant woman’s CD4 T-lymphocyte count drops below 500 cells; chronic diseases increase the likelihood of infection of the fetus.
All HIV pregnant women receive preventive therapy from week 28 and do not stop until all stages of labor are completed. It is impossible to guarantee 100% effectiveness of the drugs, so the pregnant woman is examined every 2-4 weeks from the start of therapy. The baby will be tested for HIV in the first two months of life and at six months.
Over the two decades of knowledge of the immunodeficiency virus, it has been possible to find simple and inexpensive ways to diagnose it and effective treatment, but therapy must be continuous and controlled. Get help from an infectious disease specialist by calling +7 (495) 230-00-01. Anonymity is guaranteed.
A chronic, slow infection, the final stage of development of which is a fatal deficiency of immune defense. The stage of complete decline in immunity accompanied by opportunistic diseases and infections is called acquired immunodeficiency syndrome (AIDS), the previous condition is HIV infection.
We will call you back, leave your phone number
Message sent!
expect a call, we will contact you shortly
Some numbers and facts:
- More than 933 thousand infected citizens are officially registered in Russia.
- Every year, 92 thousand Russians become infected.
- Every year, almost 20 thousand young people die from the deadly complications of AIDS.
- The increase in HIV-infected people is mainly due to young women who come into contact with infected foreigners.
Many disorders can be identified and detected through in-depth research; at the infectious disease center of the International Clinic Medica24, a patient can find out his genetic “prospects” - predisposition and the real probability of developing an infectious disease.
Prevention of HIV infection
It is important to avoid activities that may put you at risk of contracting HIV. The main steps to prevent infection include:
- Possession of truthful information about ways of contracting HIV and AIDS.
- Use condoms (male or female) when participating in any type of sexual intercourse (anal, oral, vaginal).
- Limiting the number of sexual partners.
- Awareness of the sex life of all new partners before engaging in sexual intercourse.
- Use of disposable sterile needles.
- Use only your own personal hygiene items that may have blood on them (for example, razors).
So-called emergency prophylaxis can be used if a person believes or knows that they have been exposed to the virus within the last 72 hours (three days). This risk of HIV infection exists among health care workers and among people with HIV-positive sexual partners during unprotected sex.
If exposed to the virus, post-exposure prophylaxis (PEP) should be started within 72 hours to prevent infection. It should be started as quickly as possible, ideally within a few hours of exposure to the virus. The longer the pause, the less likely it is that post-exposure prophylaxis will be effective. Additionally, please be aware that PEP may have serious side effects and does not guarantee results.
Memo for HIV-positive people: what is important to remember about your health
Studying all the information about the treatment of HIV infection is not an easy task. To help people with HIV better navigate health issues, you need to know some quick information that can help you stay healthy.
1. Avoid eating raw or undercooked meat, raw fish or raw eggs. They may contain germs that are dangerous to you.
2. If you have never had hepatitis A or B, talk to your doctor about getting vaccinated against them.
3. Undergo medical examination prescribed by the attending physician of the AIDS center:
Fluorography or radiography of the OGK - diagnosis of tuberculosis (once every 6 months)
electrocardiogram
Ultrasound examination of the abdominal organs (comprehensive)
ultrasound examination of the kidneys and adrenal glands
Examinations of doctors depending on the clinical manifestations of secondary diseases (dermatovenerologist, general practitioner, neurologist, otolaryngologist, ophthalmologist, obstetrician-gynecologist, oncologist and others).
4. Going to the dentist regularly is very important. It is advisable to have a dental examination twice a year. The first HIV-related diseases usually appear in the oral cavity.
5. Do not refuse visits to the doctor at the AIDS center. It is necessary to undergo regular testing for viral load and immune status.
6. It is better to avoid unnecessary “activation” of the immune system; due to HIV, it already has enough work to do. All diseases, especially infections, even those not related to HIV, must be treated as soon as possible. When the immune system is “activated,” the virus can multiply faster.
7. HIV-positive women need to monitor the condition of the cervix. Every 6 months you need to undergo a full gynecological examination, and it is advisable to do a cytological analysis of the cervical mucosa. This will help prevent cervical cancer.
8. If you feel constantly tired, talk to your doctor about possible anemia (low hemoglobin levels in the blood) or low hormone levels. Prompt diagnosis and treatment of these problems can help.
9. If you suddenly and rapidly lose weight, you will need treatment for weight loss syndrome.
10. If your immune status is above 200 cells/ml, get vaccinated according to the national vaccination calendar, this will help you avoid severe infectious diseases - influenza, coronavirus infection.
11. If you have HIV, this does not mean that your child will have it. Currently, the risk of mother-to-child transmission of HIV is less than 2%.
12. ARV drugs can cause undesirable (side) effects in the first month of use. If after a month they continue to bother you, consult your doctor; perhaps the proposed treatment regimen is not suitable for you.
13. Immune status determines the state of the immune system, and is an even more important test than viral load. HIV infection affects the number of CD4 cells that are destroyed by the virus. The CD4 count can be a percentage (of the total number of lymphocytes) or an absolute count (the number of CD4 per milliliter of blood). The percentage is more stable, so it can more accurately indicate the development of HIV infection.
14. Usually, although not always, viral load allows you to “predict” how quickly HIV infection will develop. The higher your viral load, the more likely it is that your CD4 count will begin to decline rapidly in the near future. If the viral load is less than 50 copies/ml, the likelihood of disease progression is extremely low.
15. Find out what signs may be present in HIV-associated cancers: Kaposi's sarcoma and non-Hodgkin's lymphoma. The sooner these diseases are diagnosed, the easier it will be to treat them.
The main treatment for HIV infection is a combination of three or more antiretroviral drugs. They make it possible to reduce the viral load below a detectable level, improve immune status and prevent HIV-associated diseases. Your doctor will choose a combination depending on your medical history and your attitude toward the dosage regimen, dietary restrictions (for example, take the drug on an empty stomach or with food) and possible side effects. You need to work with your doctor to choose a combination that's truly right for you.
Medicines must be taken every day, on time. If you are unable to do this, it is best to talk to your doctor about stopping therapy and possibly changing the combination. Regularly skipping medications can cause the virus to become resistant to their effects.
Half-time rule: if you forget to take the drug at the appointed time and there is less than half the time left before the next dose that should pass between doses, then you should not take the pill. If it is less, then the drug can be taken. For example, if you take the drug every 12 hours (in the morning, at 7.00 and in the evening at 19.00), then in the first 6 hours after missing it (i.e. until 13.00) you can take the missed pill. If you remember about the omission when there are less than 6 hours left before the next dose, the tablet must be taken only at the appointed time, i.e. at 19.00
Do not take any medications, vitamins, or dietary supplements, including over-the-counter ones, until you are sure they are compatible with the medications you are taking.
It's important to take care of your eyes. If your vision has deteriorated or you experience a “blurry picture,” be sure to consult a doctor.
Learn to communicate and collaborate with your doctor. Many people have problems in their relationship with their doctor, while others simply avoid visiting the doctor. However, as a result, you will only suffer yourself. Be proactive about your health and it will save you from many problems in the future.
Children with HIV
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Babies can become infected during pregnancy and childbirth. Infection is also possible through breastfeeding or blood transfusion. The probability of transmission of the virus from an HIV-infected mother to a newborn is 30%. Of these, 11% are infected in utero, 15% during natural childbirth, and 10% during breastfeeding.
HIV-positive babies are usually born prematurely. The infection most often appears in the first year of life. Symptoms include: delay in physical development, prolonged diarrhea, swollen lymph nodes, vomiting and nausea. Manifestations include skin rashes: pustules, vesicles, spots, atopic or seborrheic dermatitis, vasculitis, eczema.
If left untreated, HIV infection in children quickly progresses to AIDS. Life expectancy is 1-3 years. In the final stages, exhaustion syndrome, pneumonia, heart failure, and central nervous system damage are observed. Therapy for children is prescribed from the first 4-6 months of life. The treatment regimen, as for adults, changes periodically to avoid the development of viral resistance. Manifestations of HIV in adolescents are the same as in adults, with the exception of rarer cases of cancer.