Uterine polyps are local benign neoplasms growing from the endometrial mucosa. They look like tubercles located on a wide base, or round or oval formations on a thin stalk. There may be one or several of them in the uterine cavity; in the latter case they speak of polyposis. The size of polyps varies from a few millimeters to 8 or more centimeters.
- Signs of a polyp in the uterine cavity and their diagnosis
- When is polyp removal necessary?
- Methods for removing endometrial polyps
- What is hysteroscopy of the uterus for polyps
- Types of hysteroscopy
- Indications for hysteroscopy
- Features of the event
- Preparation
- Basic recovery recommendations
- Complications after polyp removal
- Contraindications
Signs of a polyp in the uterine cavity and their diagnosis
Often uterine polyps do not manifest themselves, but some patients have the following symptoms:
- Menorrhagia - heavy menstruation.
- Bleeding outside of menstruation.
- Spotting after sexual intercourse.
- Bleeding during menopause.
- Infertility and miscarriages.
- With large polyps, women may notice copious whitish discharge, discomfort and pain during intercourse, as well as periodic cramping pain in the lower abdomen.
To make a diagnosis, it is necessary to undergo a comprehensive examination, which includes the following procedures:
- Gynecological examination - particularly large polyps can be palpated during manual examination; cervical polyps can be detected during examination in the speculum.
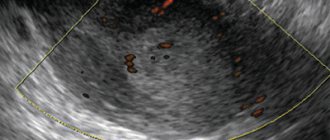
- Ultrasound of the pelvis - in the uterus, growth of the endometrium with a local increase in its mucous layer is detected. The structure of this neoplasm is homogeneous.
- Separate diagnostic curettage followed by histological examination of the obtained material.
- Hysteroscopy - allows you to examine the endometrium from the inside, visualize single or multiple polyps and determine their location. The procedure is also therapeutic in nature, since it allows for the simultaneous removal of all identified tumors and their subsequent histological examination. This is the most effective method for diagnosing a polyp in the uterus.
Operation stages:
- To examine the walls of the uterus, it is stretched.
For better visibility, a contrast medium is used - saline solution or 5% glucose. Most serious complications during hysteroscopy arise from the selection of an inappropriate environment. For example, the use of carbon dioxide as a medium is more suitable for performing hysteroscopy in the absence of bleeding from the genital tract. The presence of even slight bloody discharge will cause clouding of the environment, which will make examination of the uterine cavity impossible. In addition, carbon dioxide when stretched can cause embolism due to the thermal energy effect on tissue. Therefore, I prefer liquid media, particularly non-electrolyte solutions, as they are not susceptible to hemolysis and will not cause electrolyte disturbances. The saline solution I use does not irritate tissues and is quickly removed from the vascular bed, increasing the volume of circulating blood only temporarily. In a modern hysteroscope, thanks to its flow-through design, it is possible to remove blood and tissue particles without impairing visibility even during bleeding. - During the examination of the uterine cavity, in addition to assessing its size and shape, the relief of the uterine wall, the condition of the endometrium, and the accessibility of the mouths of the fallopian tubes are determined. The fundus of the uterus, angles, isthmic region, and cervical canal are also examined. If there are suspicious areas, tissue samples are taken using special forceps for subsequent histological examination.
- Removal of endometrial polyp using a bipolar hysteroresectoscopy loop
Using a bipolar resectoscope, the body and base of the polyp are removed; this approach prevents the development of bleeding from the polyp bed, and scar formation is excluded in the future. Multiple polyps can be removed by curettage. For better results, a combination of different methods is possible. For large polyps with a wide stalk, removal is carried out in parts - fragmentation. When removing polyps located in the area of the mouth of the fallopian tubes, technical difficulties arise, since the loop of the hysteroresectoscope may be too large for manipulation in the corners of the uterus. To destroy polyps localized in this area with underlying basement membrane, I use a loop electrode or coagulation with a ball electrode. This approach also reduces the risk of relapse in the future.
- Deviations discovered during the examination: synechiae, intrauterine septa, submucosal myomatous nodes are also removed.
Endometrial polyps are often combined with other diseases of the reproductive system: fibroids, ovarian cysts, endometriosis, etc. In this case, in our clinic it is possible to perform hysteroscopy with laparoscopy; During one anesthesia, correction of all disorders is carried out using transvaginal and laparoscopic access - through punctures of the anterior abdominal wall.
When is polyp removal necessary?
The choice of patient management tactics and determination of the need to remove the polyp is determined individually. If a woman is of reproductive age and has no symptoms of a polyp, conservative management tactics can be chosen. In this case, the patient should undergo regular monitoring.
In all other cases, removal of polyps is indicated:
- Presence of symptoms of the disease.
- Pre- and postmenopausal periods, even if there are no symptoms.
Technique of the operation
There are several types of operations as surgical interventions:
- endoscopic removal;
- removal using laser;
- transanal excision;
- rectal resection.
Endoscopic removal is carried out using an endoscope, which is inserted through the anal canal to the patient. A loop electrode is attached to the end of the device. It allows you to capture the polyp at the base, after which high-frequency current is supplied. In a few seconds, the leg is charred and the tissue of the formation is removed. If the polyp is flat and it is not possible to capture it, adrenaline is injected into it. The procedure is painless and well tolerated by most patients. Used to eliminate fibrous polyps. The body recovers in a short time. The next day you can return to your normal lifestyle.
The laser method is one of the newest. The process is also controlled by an endoscope. This allows the surgeon to see the area of impact and prevent damage to the intestinal walls. The polyp is excised with a laser, and the attachment site is treated to avoid relapse. It also promotes rapid healing and recovery after the procedure.
If the polyps are located above 7 centimeters from the anus, transanal excision is used. A rectoscope is used, which gives access to the surgeon, an electric knife or an ultrasonic scalpel. The operation lasts from 15 minutes to 1 hour depending on the number of formations. In this way, villous polyps are removed through the anus. It is performed under general anesthesia in a hospital setting. The duration of rehabilitation is short.
If the patient has malignant tumors and there is a risk of metastasis, resection is used. During the operation, the affected area of the intestine is completely removed. It is performed only under general anesthesia. This is followed by a long recovery process, which will require patient care. In particularly severe cases, complete removal of the rectum and formation of a colostomy is performed.
Methods for removing endometrial polyps
Surgical removal of endometrial polyps is called polypectomy. It involves curettage of the endometrium followed by histological examination of the resulting material. Curettage can be performed blindly, under visual control using ultrasound or hysteroscopy. The latter method is the most preferable because it allows you to control the completeness of polyp removal and avoid the development of surgical complications (uterine perforation, excessive curettage with damage to the basal layer of the endometrium, etc.).

If treatment does not help, and the patient is in menopause, she may be offered surgery to remove the uterus in the following cases:
- Persistent relapses of multiple polyposis.
- High risk of malignancy of polyps.
- The presence of severe symptoms that significantly worsen a woman’s quality of life.
Do I need to remove polyps in the uterus?
The opinion of experts is clear - remove them, since they are often the cause of infertility and can lead to various complications. In some cases, the final decision is made by the patient, who is informed of the possible consequences of refusing surgery. If the following indications are present, surgical intervention is mandatory:
- age after 40, premenopausal period, when hormonal changes occur in the body, provoking the active growth of tumors;
- if the size of the polyps is more than 10 mm, they interfere with conception, cause bleeding, and can develop into oncology;
- in the treatment of infertility - overgrown formations impair the movement of sperm through the tubes, and even in the case of fertilization lead to termination of pregnancy in the early stages;
- lack of effect from hormone therapy, which relieves the symptoms of the disease - bleeding, menstrual irregularities, pain, discharge mixed with pus;
- the presence of adenomatous forms.
The decision is made by the doctor after diagnosis. If the neoplasms are single, their size does not reach 10 mm, conservative treatment with the use of hormonal drugs is possible.
Types of hysteroscopy
There are diagnostic or surgical hysteroscopy. Diagnostic involves only examining the endometrium and endocervix for the presence of pathologies. The study is performed on an outpatient basis and does not require serious anesthesia (local anesthesia and sedation are sufficient) and a long recovery period. Therefore, it was called office hysteroscopy. Based on its results, the doctor draws up a plan for further management of the patient.
Surgical hysteroscopy allows for diagnosis and immediate treatment of identified pathologies. It is performed in an operating room and requires full anesthesia. The procedure is prescribed either when the diagnosis has already been established, or when the likelihood of detecting a pathology is extremely high.
We specialize in surgical hysteroscopy because we believe that invasive diagnostic techniques can be successfully replaced by safer tests. This will help make the correct diagnosis without the risk of surgical complications.
Examinations and tests performed before hysteroscopy
Before performing a hysteroscopy, it is necessary to undergo an examination. The list of tests depends on the specific situation and may vary; for diagnostic purposes, the first three points are sufficient:
- Ultrasound of the pelvic organs
. - Smear on flora and degree of vaginal cleanliness
. - Blood test for Syphilis; HIV; Hepatitis B and C
. - Detailed blood test.
- Biochemical blood test (total protein, bilirubin, creatinine, urea, sugar, Ka, Na).
- Coagulogram.
- ECG.
- Consultation with a therapist.
Based on the results of the examination, the woman consults a gynecologist; if there are no contraindications, she is sent for the procedure.
If acute inflammatory processes and STDs are detected, hysteroscopy is contraindicated!
Back to contents
Features of the event
Therapeutic hysteroscopy is carried out on a hospital basis, including a one-day hospital in an operating room. An hour before the start of the intervention, premedication is performed - a sedative injection is given. After being delivered to the operating room, the patient is placed in a gynecological chair and given intravenous anesthesia. Next, proceed to the operation:
- Dilation of the cervical canal.
- A certain amount of sterile liquid is injected into the uterine cavity to “straighten” its walls.
- A hysteroscope is inserted through the cervical canal. As it is introduced, a step-by-step examination of all parts of the uterus is performed. First, the cervical canal is examined, then the uterine cavity and its angles.
- If necessary, surgical procedures are performed - taking a biopsy, removing polyps, dissecting synechiae, etc.
- At the end of the operation, fluid is removed from the uterine cavity.

Hysteroscopic method
Polyp removal using hysteroscopy is a low-traumatic procedure performed under local or general anesthesia, lasting no more than 20 minutes. When examining the uterine cavity using an endoscopic device with a fiber optic system, the number of outgrowths and location are determined, after which they are removed. Removal of the polyp can be done either by unscrewing or cutting, then the bed is treated (cryogenically, tincture of iodine, cauterization).
In recent years, laser removal of a polyp in the uterus has been considered more effective. In this case, pathological tissues are destroyed, the risk of relapse is minimal. In addition, after the procedure there are no scars, reproductive function is not impaired, this is very important for women planning to conceive. The material extracted during hysteroscopy is sent for histology. In some cases (bleeding, the presence of several formations, etc.), it is necessary to perform curettage, during which the top layer of the mucosa is removed. If atypical cells are found in it, or there is a risk of degeneration into a malignant formation, surgical removal of the polyp in the uterus is recommended. The operation consists of hysterectomy or supravaginal amputation. In some situations, removal of the appendages is recommended.
Preparation
Preparation for hysteroscopy is similar to other surgical interventions in gynecology. First, an examination and, if necessary, certain treatment are carried out. The following tests are performed:
- General blood and urine analysis.
- Coagulogram.
- Blood type and Rh factor.
- Vaginal smear for flora.
- ECG.
- Test for STIs.
- Tests for HIV and parenteral hepatitis.
Hysteroscopy is planned at the beginning of the menstrual cycle (before day 10), since endometrial tumors are clearly visible during this period.

Immediately before surgery, it is recommended to follow these rules:
- Two days before hysteroscopy, avoid sexual contact.
- On the day of the operation, take a shower and then put on underwear made from natural fabrics.
- Remove jewelry and contact lenses.
- Immediately before entering the operating room, empty your bladder.
- Do not eat for at least 6 hours before anesthesia.
Hysteroscopy of the uterus

Hysteroscopy is an accurate diagnostic method that allows you to detect gynecological diseases of the uterine cavity with a probability of almost 100%. This is not an alternative to ultrasound, radiography and other endoscopic examination methods, but a technique that is the final method of diagnosis when it comes to the uterine cavity.
The essence of hysteroscopy
The procedure is performed using a hysteroscope device.
It makes it possible to penetrate the uterine cavity without surgical incisions and punctures - through the cervical canal. The device is a tube with an optical device and a light bulb at the end, only 3 mm thick. The tube is inserted into the uterus, the image is shown on the monitor screen, where the doctor assesses the condition of the internal walls of the organ, the cervical canal, and the mouths of the fallopian tubes. The hysteroscope provides an image magnified tens and hundreds of times and allows one to evaluate the nature of the tissue - the endometrium in the uterine cavity. To carry out the examination, the uterine cavity needs to be expanded - a sterile saline solution is pumped into it under controlled pressure, about 100 ml in total.
Why is hysteroscopy needed?
A diagnostic examination is prescribed if there are controversial suspicions about the diagnosis: to clarify the nature of the pathology, its localization or to refute doubts. The main goals of hysteroscopy:
- detection of polyps and other formations in the uterine cavity, establishing tissue integrity;
- searching for the source of internal bleeding;
- removal of foreign bodies, including spirals;
- removal of remnants of the fetal membrane during spontaneous termination of pregnancy;
- performing a biopsy if there is a suspicion of cancer;
- identifying possible causes of infertility and miscarriage;
- control examination after miscarriage, abortion or other surgical interventions on the uterus;
- monitoring the effectiveness of hormonal therapy.
In addition to diagnosis, hysteroscopy is used for treatment as a method of surgical intervention. The devices have additional instruments (forceps, scissors, electrodes, laser), with which the doctor excises tissues and adhesions, removes blood clots, and cuts out polyps. This operation, unlike a diagnostic procedure, is performed under general anesthesia.
Advantages of the method
Hysteroscopy takes the diagnosis of gynecological diseases to a new level - maximum information content is combined with safety and comfort for the patient. Advantages of the method:
- the procedure is painless and is performed under 20-minute anesthesia;
- does not require strong expansion of the cervical canal and minimal expansion when removing a polyp, for example;
- the risk of damage to the walls of the uterus is also low, since hysteroscopy is carried out under visual control;
- ensures a thorough inspection of all areas;
- allows for targeted biopsy, that is, to take cells for analysis from a precisely planned location of the uterus;
- the recovery period is faster and easier than with other examination methods;
- you can begin surgical treatment immediately after diagnosis;
- the process is filmed, the gynecologist can review the procedure again.
Thanks to such a detailed study, the doctor selects the most correct method of treatment.
Indications
Hysteroscopy of the uterus is prescribed for suspected pathologies, problems with pregnancy, complications after childbirth, or during menopause.
Frequent indications for therapeutic and diagnostic hysteroscopy:
- suspicion of malformations of the uterus and cervix - aplasia, bicornuate uterus, embryonic cyst;
- clarification of the preliminary diagnosis: endometrial hyperplasia, endometriosis, polyposis, fibroids, submucosal myomatous nodes;
- bleeding for unknown reasons;
- serious disruptions in the menstrual cycle;
- infertility;
- suspicion of cancer;
- control of cleanliness after surgical interventions on the uterus;
- preparation for the IVF procedure;
- ingrowth of intrauterine contraceptives into the walls of the uterus.
In addition, hysteroscopy helps determine the size of nodes and neoplasms and their exact location.
Therapeutic hysteroscopy of the uterus is usually combined with other methods - often with an endometrial biopsy, for the purpose of taking samples for histological analysis, as well as for immunohistochemical analysis (if indicated).
Contraindications
Although the procedure is simple, it cannot be performed in the following cases:
- serious inflammatory processes of the vagina, cervix or uterine cavity. Hysteroscopy can be performed after successful treatment;
- general infectious diseases - ARVI, inflammation of the kidneys, bladder and other organs in the acute stage;
- pregnancy at any stage;
- cervical stenosis. This is a tight closure of the cervical canal due to the presence of synechiae - fusion of the cervix.
Preparation for hysteroscopy
Hysteroscopy for diagnostic purposes is performed under local anesthesia on an outpatient basis. But first you need to get permission from your therapist and undergo research:
- general blood test, biochemistry, determination of group and Rh factor;
- coagulogram (test for blood clotting);
- general urine analysis;
- tests for HIV infection, syphilis, hepatitis;
- a smear from the genital tract for flora (if necessary, from the cervical canal) - to exclude infections in the vagina and not to bring it inside the uterus;
- electrocardiography (ECG);
- fluorography;
- Ultrasound of the pelvic organs - to determine the thickness of the walls of the uterus, to refute pregnancy.
Based on the results, the therapist gives permission for medical intervention and anesthesia and writes a conclusion.
If the patient suffers from diabetes, consultation with an endocrinologist will be required. Before hysteroscopy, it is recommended to stop taking medications that affect blood clotting and increase the risk of bleeding: heparin, warfarin, syncumar, and other anticoagulants. The doctor may prescribe a course of antibiotics to prevent infectious complications after the procedure.
On the eve of hysteroscopy you need:
- exclude sexual intercourse for two days;
- remove pubic hair, labia, perineum within 24 hours;
- in the morning, on the day of surgery, perform a thorough toileting of the external genitalia;
- immediately before the procedure, empty your bladder.
It is forbidden to eat 12 hours before hysteroscopy, and drink 6 hours before hysteroscopy.
Progress of the procedure
If diagnostic hysteroscopy is planned in advance, it is performed on a specific day of the menstrual cycle (in each specific situation, the doctor prescribes a specific day, depending on the purpose of the manipulation).
It can be done without anesthesia, but many patients prefer local anesthesia. The procedure is performed under mild anesthesia and lasts about 20 minutes.
First, the doctor treats the external genitalia with antiseptics, fixes the cervix with instruments and disinfects it with an antiseptic for the mucous membranes. Then a probe is inserted and the length of the uterus is determined. The cervix expands slightly, it is washed - an outflow of secretions occurs. Further actions:
- One part of the hysteroscope is inserted into the cervix, the other remains in the hands of the doctor;
- fluid is released to expand the uterine cavity and the mouths of the fallopian tubes;
- the doctor examines each area clockwise, assesses the color, relief, and structure of tissues based on the image on the monitor. If tissue excision is required, surgical instruments are inserted into the uterus at this stage;
- after all manipulations, the fluid is removed from the uterine cavity;
- the device is carefully removed.
Hysteroscopy for diagnostic purposes takes from 15 to 30 minutes.
Recovery period
After diagnostic hysteroscopy, the woman is immediately sent home.
She may feel nagging pain in the lower abdomen, similar to menstrual pain - the uterus contracts, reacting to irritation from instruments. Sometimes spotting appears on the first day, this is normal. Within 7–10 days you need to follow the recommendations:
- give up active physical activity, postpone fitness and sports activities;
- maintain careful intimate hygiene;
- abstain from sexual intercourse;
- do not visit bathhouses, swimming pools, or swim in open water. Also, after hysteroscopy, you should not take a bath - there is a high probability of infecting the tissues;
- replace tampons with sanitary pads, do not use candles;
Otherwise, after hysteroscopy you can lead a normal life. On the appointed day, you need to visit a gynecologist for a control examination of the uterus.
Possible complications
Diagnostic hysteroscopy is a fairly safe procedure; in most cases, serious consequences should not be expected, but the following phenomena are possible:
- severe cramping pain in the lower abdomen;
- heavy prolonged bleeding that does not stop even after 3–4 days;
- development of inflammatory processes - if the doctor’s recommendations after hysteroscopy were not followed and infectious agents entered the uterine cavity.
In this case, you cannot carry out treatment yourself - contact a gynecologist, he will prescribe hemostatic, anti-inflammatory, antispasmodic drugs.
Since hysteroscopy involves penetration into the uterus, albeit under visual control, there is a risk of medical errors. Perforation of the uterine walls is also possible.
To avoid such consequences, contact experienced and highly qualified specialists. In a multidisciplinary medical center, therapeutic and diagnostic hysteroscopy is performed by expert doctors with 15 years of experience, who have many complex gynecological operations under their belts. With us, you can undergo all the tests necessary to prepare for hysteroscopy, and after it, be observed by highly qualified gynecologists. We are waiting for you at Nizhny Novgorod, st. Studenaya, 57 - every day from 8:00 to 20:00.
Basic recovery recommendations
- If an antibiotic is prescribed, take it for as long as your doctor recommends.
- To relieve pain after hysteroscopy, you can take antispasmodics or analgesics.
- Avoid sexual intercourse and heavy physical activity until the bleeding stops, but not less than 10 days.
- Perform hygiene measures in the shower. Taking a bath is not recommended.
- Toilet your genitals as needed, but at least 2 times a day.
- During the recovery period, it is not recommended to use tampons and menstrual cups; discharge should come out of the vagina freely.
Most women generally feel satisfactory after therapeutic hysteroscopy. The main complaints are nagging pain in the lower abdomen and weakness. The full recovery period takes about two weeks. However, if complications develop - fever, heavy bleeding, foul-smelling discharge, you should immediately consult a doctor.
Recovery
After using minimally invasive polypectomy techniques, the recovery period is 2-3 months, which depends on the patient’s age, body condition, the nature of the tumors, their size, and quantity. To consolidate the effect and prevent relapses, the following types of therapy are practiced:
- Medication. For the first three days, No-Shpa (Drotaverine) is prescribed to eliminate pain and also prevent the accumulation of blood clots in the uterus. If necessary, anti-inflammatory, antiseptic and/or antibiotics if there is a pathogenic microflora.
- Herbal medicine, taking vitamins, dietary supplements, diet, promoting a speedy recovery.
- Hormone therapy. Indicated if the occurrence of polyps is due to hormonal imbalance. The selection of drugs is carried out individually.
One of the treatment methods or all in combination can be used. Also, after the operation, you cannot have sex, lift weights (no more than 3 kg), play sports, go to the sauna, or take baths.
Complications after polyp removal
As after any gynecological operation, the following complications may develop after hysteroscopy:
- Damage to the wall or cervix - treatment may require additional surgery to close the perforation.
- Damage to the cervix - may require stitches.
- Bleeding.
- Infectious complications.
It should be noted that complications after hysteroscopy are much less common than after other gynecological interventions performed “blindly”. But the possibility of their development cannot be completely excluded.
Content
- Why you need to prepare for hysteroscopy
- Examinations and tests performed before hysteroscopy
- Recommendations before hysteroscopy
- Recommendations after hysteroscopy
Hysteroscopy in Krasnoyarsk
In our clinic, hysteroscopy is performed in Gynecological 106.
- Diagnostic hysteroscopy - 9500.00 rub.
- Operative hysteroscopy - RUB 13,000.00.
- Intravenous anesthesia - RUB 3,500.00.
Registration for hysteroscopy
Read more about hysteroscopy in this article
Contraindications
- The presence of decompensated chronic diseases that may interfere with anesthesia, for example, cardiovascular pathology.
- Presence of STIs and vulvovaginitis.
- The presence of diseases accompanied by a tendency to bleeding.
Euroonco specialists closely monitor the condition of patients not only in the postoperative period, but also at the initial stage. In this regard, we perform the procedure only after we are convinced that the patient has no contraindications. You can make an appointment for a consultation about uterine polyps by calling:
Book a consultation 24 hours a day
+7+7+78
Benefits of hysteroscopy
- There is no need to dissect the anterior abdominal wall and uterus, so healing occurs faster;
- The possibility of visualization makes it possible to confirm or exclude the presence of a polyp with greater certainty compared to ultrasound or MRI, to specifically remove it without damaging surrounding tissues, and reduces the risk of developing intraoperative complications;
- In most cases, to remove polyps, a hysteroresectoscope is used - a special instrument that has a loop, with the help of which the polyp is cut off under visual control - when removing a polyp with a curette without visual control with a hysteroscope, it is possible to leave the “leg” of the polyp and its recurrence in the same place;
- Due to the absence of extensive tissue damage, there are no intense painful manifestations in the postoperative period;
- The hospitalization period does not exceed 1-2 days, which is economically beneficial for patients;
- Full recovery takes about 2 weeks, after which the woman is considered able to work;
- Since endometrial polyps are often combined with other pathologies (intrauterine septa, synechiae), they are also removed during hysteroscopy.
And most importantly: with the advent of this low-traumatic technique, the number of radical operations to remove an endometrial polyp has decreased by 40%, which means preserving the uterus and the ability to bear children.
What is a polyp
This is a benign formation that does not have characteristic symptoms. However, it can cause intrauterine bleeding, preventing a woman from becoming pregnant and successfully bearing a child. Another serious danger is that after 45 years, a polyp can degenerate into a cancerous tumor.
If several such balls appear in the uterus, this is called polyposis. The size of the formations varies from 1 to 80 mm. In some cases it may exceed these parameters. Often this phenomenon develops against the background of other concomitant diseases. One of them is endometriosis.
Causes
The causes of polypoid formations are disclosed only for certain types of pathology (familial polyposis). The risk groups for developing polyps in the intestines are calculated statistically. • The age factor is of great importance. WHO recommends regular colonoscopy after age 55. • In second place in importance is hereditary predisposition (benign tumors and/or rectal cancer in close relatives). • Doctors believe that additional factors are necessary for the genetic defect to occur: chronic inflammatory processes in the large intestine and/or congestion associated with stool retention. • The nature of nutrition matters: dairy and plant foods reduce the risk of benign and malignant formations. The presence of carcinogens in food, including smoked foods, can trigger the development of cancer.
Symptoms
Rectal polyps are characterized by an asymptomatic course. In typical cases, formations are discovered accidentally during examinations that were prescribed for preventive purposes or for the diagnosis of another disease. Symptoms appear with significant growth sizes, as well as with multiple polyposis. • Formations consisting of fibrous tissue are prone to inflammatory reactions, which are manifested by signs of proctitis: frequent painful urge to defecate, loose stools, mucus and pus on the surface of the stool. • Adenomatous (glandular) polyps secrete a lot of mucus into the intestinal lumen, which can cause loose stools. • Villous formations often bleed, so blood may be released in the stool. • growing on a long stalk can “fall out” from the anus, attracting the attention of patients.