Insulin is a hormone produced in the pancreas, so named because it is located behind the stomach. Insulin allows our body to use glucose for energy. Glucose is a type of sugar, a monosaccharide (simple carbohydrate) found in many foods.
After a meal or snack, enzymes in the digestive tract break down complex carbohydrates and convert them into glucose. Glucose is then absorbed into the blood through the lining of the small intestine.
What does insulin do to glucose?
As soon as glucose enters the bloodstream, insulin begins to work. The hormone causes cells in our body to absorb sugar and use it to produce energy.
Insulin also helps balance blood glucose levels. When there is too much glucose in the blood, insulin signals the body to store the excess in the liver. Glucose stored in liver cells is not released until its level in the blood decreases, for example, between meals or when our body is stressed or needs additional energy (during exercise, intense mental work).
In addition to the liver, at the “command” of insulin, excess glucose accumulates in adipose (lipid) tissue, also creating a kind of “depot” there to quickly compensate for the energy spent.
A little history
The hormone insulin, isolated from the pancreas, was first successfully used for medicinal purposes by the Canadian physician, physiologist, F.G. Bunting. For this, in 1923, at the age of 32, he was awarded the Nobel Prize in Physiology or Medicine along with his Scottish colleague, Professor MacLeod, in whose laboratory the young scientist conducted experiments on dogs. The discovery of insulin therapy completely revolutionized approaches to the treatment of diabetes. In recognition of the services of Banting, who tragically died in a plane crash during the Second World War, World Diabetes Day is celebrated on his birthday, November 14th.

Frederick Grant Banting was the scientist who first obtained insulin extract and successfully used it in the treatment of diabetes. One of the youngest Nobel Prize laureates ever since it was awarded.
Insulin: normal hormone content in the blood, methods of increasing and decreasing
It is very important that the level of insulin in the blood is always within normal limits. Both low and high insulin are evidence of metabolic disorders (primarily carbohydrate metabolism).
However, determining the amount of hormone released into the blood in itself is rarely sufficiently informative. The fact is that the level of insulin in the blood can normally fluctuate widely - from 3 to 20 µU/ml in children and up to 25 µU/ml in adults. In pregnant women and women over 60 years of age, these boundaries are shifted; their normal amount of the hormone ranges from 6 to 27/36 µU/ml.
Therefore, it is necessary to determine the level of insulin in the blood together with the level of glucose (sugar) - on an empty stomach and after a certain time after eating. Based on these indicators, certain indices are calculated, which allow the doctor to detect the problem and take measures to correct or eliminate it.
Elevated fasting insulin with normal sugar may be a consequence of cancer (adenocarcinoma of the insulin-producing cells of the pancreas).
Excessive amounts of insulin and normal amounts of sugar 2 hours after eating are detected in people with so-called prediabetes. Their metabolic processes are sluggish, and the body tries to speed up glucose metabolism by producing increased amounts of the hormone. Such intensive work over time leads to “wear and tear” of the pancreas, as a result of which it can no longer produce not only excess, but also sufficient amounts of the hormone.
1. General blood test.
Before taking a general blood test, the last meal should be no earlier than 3 hours before the blood draw.
2. Biochemical blood test.
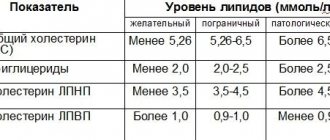
To determine cholesterol and lipoproteins blood is taken after a 12-14 hour fast. Two weeks before the study, it is necessary to discontinue drugs that lower blood lipid levels, unless the goal is to determine the lipid-lowering effect of these drugs.
To determine the level of uric acid in the days preceding the study, it is necessary to follow a diet: avoid eating foods rich in purines - liver, kidneys, limit meat, fish, coffee, tea as much as possible in the diet. Intense physical activity is contraindicated.
Blood donation for hormonal testing is carried out on an empty stomach (preferably in the morning; if this is not possible, 4-5 hours after the last meal in the afternoon and evening). On the eve of the test, high-fat foods should be excluded from the diet, and the last meal should not be large.
The results of hormonal studies in women of reproductive age are influenced by physiological factors associated with the stage of the menstrual cycle, therefore, when preparing for an examination for sex hormones, you should indicate the phase of the cycle and adhere to the recommendations of your doctor about the day of the menstrual cycle on which you need to donate blood.
Hormones of the reproductive system in women are tested strictly according to the days of the cycle:
- LH, FSH - 3-5 days;
- Estradiol - 5-7 or 21-23 days of the cycle;
- progesterone 21-23 days of the cycle.
- prolactin, 17-OH-progesterone,
- DHA sulfate, testosterone - 7-9 days.
- Blood for insulin and C-peptide is given strictly on an empty stomach in the morning. Thyroid hormones, insulin, C-peptide are given regardless of the day of the cycle.
In men, reproductive hormones are released in the morning (8-9 am).
Before donating blood for stress hormones (ACTH, cortisol) , you need to calm down, when donating blood, get distracted and relax, since any stress causes an unmotivated release of these hormones into the blood, which will lead to an increase in this indicator.
The requirements for donating blood when testing for infections are the same as when studying a hormonal profile. Blood is donated on an empty stomach (in the morning or 4-5 hours after the last meal in the afternoon and evening, and this last meal should not be heavy, and high-fat foods should be excluded from the diet the day before the test). The results of tests for the presence of infections depend on the period of infection and the state of the immune system, so a negative result does not completely rule out infection. In doubtful cases, it is advisable to re-test after 3-5 days.
A blood test for the presence of antibodies of the IgG, IgM, IgA classes to infectious agents should be carried out no earlier than 10-14 days from the moment of illness, since the production of antibodies by the immune system and the appearance of their diagnostic titer begins during this period. At an early stage of the disease, seroconversion occurs (absence of antibodies during the acute period of the disease).
Before donating blood for viral hepatitis , 2 days before the test, it is advisable to exclude citrus fruits, orange fruits and vegetables from the diet.
Before donating blood for coagulation studies, you must inform your doctor about taking anticoagulant medications.
How to lower insulin in the blood
You can regulate the level of insulin in the blood when it increases during food intake:
- drugs that reduce insulin resistance of body cells (metformin, etc.);
- normalization of disturbed night sleep;
- dosed sports activities - swimming, running, etc.
By the way, when diagnosing prediabetes, restoring normal night sleep, as a rule, becomes the most important condition for losing weight, the ability to tolerate physical activity, and, most importantly, for restoring hormonal metabolism and eliminating insulin resistance. This allows you to slow down the transition of prediabetes to diabetes, and in some cases, completely stop this process.
Low insulin with high sugar is determined when the pancreas is unable to produce the required amount of insulin on its own, i.e. The patient develops diabetes mellitus. This picture can be observed both in type 1 diabetes (T1DM) and in the non-insulin-dependent form of the disease. And although type 2 diabetes (T2DM) is called non-insulin-dependent, when pancreatic function decreases below certain values, such patients, like people with type 1 diabetes, are treated with insulin.
When is an insulin level test prescribed?
To control the metabolic processes responsible for the absorption of glucose, a variant was developed to measure the amount of the hormone in the blood. It is prescribed to patients for the following indications:
- any cuts and small wounds take a very long time to heal;
- without physical activity, dizziness appears;
- the patient complains of double vision;
- without physical activity, sweating increases;
- fails the memory of young patients;
- there is constant irritability;
- proper rest does not help get rid of the feeling of chronic fatigue;
- tormented by constant thirst.
In addition, insulin levels are studied:
- for the purpose of diagnosing endocrine system disorders;
- if you suspect the development of diabetes mellitus;
- if necessary, monitor the progression of diabetes mellitus;
- in order to establish the required dose of insulin for a diabetic patient;
- in order to find out the reason for the decrease in blood sugar levels;
- if you suspect the formation of pancreatic tumors;
- if the patient is overweight;
Insulin as a cure for diabetes
Insulin injections can help treat both types of diabetes. Injectable insulin for diabetes acts as a replacement or supplement for your body's insulin. Type 1 diabetes requires insulin to control blood glucose levels.
Many people with type 2 diabetes can control their blood glucose levels with oral medications and/or lifestyle changes. However, if these treatments do not help, then, as mentioned above, they may also need insulin.
general characteristics
A hormone secreted by beta cells of the pancreas. Regulates the metabolism of carbohydrates, proteins, fats in the body. An increase in blood glucose stimulates insulin secretion. Insulin, in turn, ensures the absorption of glucose by tissues and stimulates glycogenesis in the liver. When treated with insulin drugs (due to the possible appearance of antibodies to exogenous insulin), the level of insulinemia varies depending on the concentration of antibodies. In this case, it is better to replace the determination of the level of endogenous insulin with a study of C-peptide. An insulin-glucose ratio > 0.3 suggests the presence of insulinoma.
Insulin therapy for type 1 diabetes
Since the body of patients with this form of the disease has practically no insulin of its own, its supply must be replenished every day to maintain a stable level of sugar (glucose) in the blood. Therefore, the main treatment for patients with T1DM is insulin therapy. All types of insulin have the same effect. They mimic the natural rise and fall of insulin levels in the body throughout the day. The composition of different types of insulin affects how quickly and for how long they work.
- Rapid-acting insulin: This type of insulin begins to work about 15 minutes after the injection. Most often used before meals. Its effect can last from three to four hours.
- Short-acting insulin: You also take this insulin before meals. Short-acting insulin begins to work 30–60 minutes after administration, and its effect lasts from five to eight hours.
- Intermediate-acting insulin: This type of insulin begins to work one to two hours after the injection and its effects can last from 14 to 16 hours.
- Long-acting insulin or long-acting insulin: begins to work no earlier than two hours after administration, the effect lasts up to 24 hours or more.
With the basal-bolus therapy regimen, two types of insulin are administered:
- A "basal" dose of insulin (also called long-acting insulin) allows the body's cells to process sugar, providing the body with the energy it needs to keep it functioning properly.
- In addition to basal insulin, people with type 1 diabetes also need a “bolus” (rapid-acting dose) of insulin at mealtimes, which helps to properly utilize the sugar from each meal.
That is, basal insulin maintains sugar levels at the desired level outside of meals and at night to ensure the accumulation of background insulin, and bolus insulin - before meals to prevent spikes in blood sugar levels after meals.
Patient preparation rules
Standard conditions:
In the morning before 11-00, on an empty stomach, after 8-12 hours of fasting.
Important:
Agree with your doctor about the possibility of performing it on an empty stomach and/or after a load of glucose or food.
Possible:
During the working day of the diagnostic department of ML "DILA". A break of at least 6 hours after eating (fatty foods should be excluded).
You can add this study to your cart on this page