Chemotherapy
Levikin
Evgeny Alexandrovich
20 years of experience
Oncologist
Make an appointment
Bone cancer is the common name for malignant tumors that develop in bone and cartilage tissue. Oncologists call such neoplasms sarcomas, since they are formed from connective tissue cells, not epithelium. The main share of diseases is secondary cancer caused by metastases from other organs. Primary tumors develop in bone and cartilage tissue much less frequently. Sarcomas typically develop in children, adolescents and young adults under 35 years of age and more often affect men than women.
Kinds
Based on histological characteristics, bone cancer is divided into the following types.
- Metastatic. The secondary tumor has all the properties and features of the original focus of pathology.
- Osteosarcoma. The most common primary neoplasm that forms in the bones of the pelvis and limbs. The main risk group is boys and young men aged 10 to 30 years.
- Chondrosarcoma. The second most common type of primary tumor is formed from cells of cartilage tissue, and the incidence increases with increasing age. The limbs, pelvic and cranial bones, shoulder blades, as well as internal organs that contain cartilage - the larynx, trachea - are affected.
- Ewing's sarcoma. The disease is typical for children and young people under 30 years of age and forms in the bones of the limbs, pelvis, ribs, and shoulder blades.
- Fibrous histiocytoma. In the malignant form, the neoplasm usually develops in soft tissues, but sometimes occurs in the bones, localized mainly in the knee area, and very rarely metastasizes, being limited to local growth.
Black spots on MRI of the brain
Black spots on a brain MRI may indicate the following:
- Loss of MR signal (The fact is that the tomograph is tuned to hydrogen atoms in the human body. If they are not present in some places, the tomograph signal simply does not pass through): In the paranasal sinuses
- At the base of the skull
If the first reason is the norm for MRI of the brain, then the rest speak of pathologies. But don’t try to decipher the picture and diagnose yourself! Most likely, this will lead to missing the true disease.
MRI in our center
Power 1.5 Tesla
High image quality
Study for patients up to 250 kg
Burn to disc for free
Symptoms
The disease begins to manifest itself quite early compared to other tumors, but the first signs and symptoms of bone cancer are not specific, inherent exclusively to this pathology. First, pain appears in the joint or bone affected by the tumor. The pain is short-term, but then becomes constant and intensifies, and cannot be reduced with conventional painkillers. The pain gets worse at night and when the bone is under load. In addition, the patient develops:
- swelling of soft tissues in the tumor area;
- decreased joint mobility or softening of the bone;
- lameness or other mobility limitations;
- decreased sensitivity of the affected limb;
- an increase in the size of regional lymph nodes;
- local increase in temperature at the tumor site;
- thinned, pale skin with a clear vascular pattern;
- weight loss for no apparent reason;
- feeling of constant fatigue.
If one or more of the listed symptoms persist for two to three weeks or longer, you should immediately consult an oncologist.
Diagnosis of bone tumors
The main symptom when a tumor appears is the presence of the tumor itself, often a growing one, and pain in the area of the tumor lesion. Diagnostics comes down to examining the patient by a doctor, performing diagnostic procedures such as X-rays, MRIs, and, if necessary, other more specialized techniques. The crown of the diagnostic trifecta is the morphological examination of the tumor, which involves either the study of biopsy material or the study of the tumor itself, that is, its preparation (surgical material).
Causes and risk factors
Currently, the mechanism of development of cancer of the bones of the skull, extremities, pelvis and other bone formations has not been thoroughly determined, but oncologists have been able to identify unfavorable factors that increase the risk of developing tumors in bone tissue. The most important of them are:
- predisposition inherited from close relatives;
- history of bone tissue injuries - fractures, cracks;
- benign neoplasms in bones;
- deviations in hormonal levels that provoke active cell division in children and adolescents;
- increased dose of radioactive radiation received by the body;
- prolonged contact with carcinogenic substances;
- smoking tobacco.

The most common cause of the disease is metastases from other organs affected by tumors.
Recently, the theory of psychosomatics of bone cancer - the relationship between psychological experiences and diseases affecting the body - has been gaining popularity. Of course, there is a certain relationship here, and any doctor will confirm that a patient who sincerely and strongly wants to get well restores health faster than an apathetic person broken by illness. However, this theory has not yet been confirmed by serious research, so official medicine does not take it into account.
1.What is an x-ray of the spine?
X-rays of the spine are possible thanks to special radioactive beams that can penetrate most objects, including the human body. The image obtained using x-rays is developed on film or displayed on a computer screen. Dense tissues, such as bone, block more radiation, so they appear white on an x-ray. Less dense tissues - such as internal organs - block less X-rays, so they appear gray.
Spinal x-rays are performed to detect injuries or diseases of the discs or joints of the spine. X-rays of the spine can show fractures, displacements, infections, tumors, spurs, and intervertebral disc disease. An X-ray of the spine also allows you to see spinal curvature, scoliosis, and other defects.
The spine is usually divided into 4 parts, and x-rays of these parts are usually taken separately:
- X-ray of the cervical spine;
- X-ray of the thoracic spine;
- X-ray of the lumbar spine;
- X-ray of the sacral spine and coccyx.
X-rays of the lumbar spine and X-rays of the cervical spine are the most common.
A must read! Help with treatment and hospitalization!
Stages
Oncologists distinguish four main stages of bone cancer, which vary in size and spread of the tumor.
- The small neoplasm is limited to the area of the bone in which it originally formed and consists of highly differentiated cells.
- The tumor remains within the bone, but its cells transform into malignant ones. The lymph nodes are not affected, there are no metastases to other organs.
- Malignant cells leave the bone and spread to nearby lymph nodes or soft tissue. There are no metastases to other organs.
- The tumor penetrates deep into the soft tissues, metastasizes to other organs - lungs, liver, kidneys, reproductive system, etc.
The need to visualize tumors using MRI
New growths in the images can be detected already at the initial stage of cancer. A modern MRI machine is capable of detecting the slightest fluctuations in neoplasia.
If bone cancer is suspected (detected), MRI is performed in the following cases:
- When diagnosing the bone, benign formations/indurations of unclear origin were identified, which threaten to progress to the stage of a malignant tumor. In this situation, it is necessary to undergo an MRI a couple of times a year.
- The tumor was detected at the initial stage using other diagnostic methods and its treatment requires a simple operation without the use of chemotherapy or radiotherapy, but only requires clarification of the location of the tumor.
- In case of opposite diagnoses made using other methods (after radiographs and ultrasound).
- Before performing surgery in order to draw up a plan for tumor elimination. An MRI image will allow you to see the level of proliferation, damage to neighboring vessels, and decide whether it is necessary to involve a neurosurgeon or cardiac surgeon in the operation.
- In order to monitor the effect of the treatment. MRI does not use dangerous radiation, so the procedure can be performed several times a year.
To scan the bones of the neck and chest, contrast tomography is mandatory. Therefore, questions like “Is the tumor visible on MRI?” should not arise. Only with its help can you clearly visualize the result. The bones in these sections have a hollow structure and a small number of water molecules, so the signal passes through worse, and the MRI scanner produces an unclear picture, which is why the doctor has incomplete information.
Diagnostics
Symptoms and manifestations of bone cancer do not allow us to accurately determine the presence of a tumor. Therefore, laboratory diagnosis of bone cancer and instrumental studies are of utmost importance.
- Radiography. Images of the affected bone in several projections make it possible to recognize structural disturbances and identify damaged areas.
- . Computed tomography is the most accurate and informative non-invasive study of bone tissue, allowing to identify the smallest changes in its structure.
- PET/CT. The study reveals even small tumors, which is important if the oncological process is secondary.
- Biopsy. Local or general anesthesia is used to collect a bone tissue sample.
- Histological analysis of the biopsy specimen. The dissected cells are examined under a microscope to determine the histological type of tumor.
- Genetic analysis of biomaterial. To identify a specific marker for Ewing's sarcoma, this test must be performed before the biopsy.

Attention!
You can receive free medical care at JSC “Medicine” (clinic of Academician Roitberg) under the program of State guarantees of compulsory medical insurance (Compulsory health insurance) and high-tech medical care.
To find out more, please call +7, or you can read more details here...
Treatment
To cure bone cancer, a team of doctors with different specializations is needed: an oncologist, an orthopedic surgeon, a chemotherapy and radiation therapist, as well as a rehabilitation specialist and a psychotherapist. During the treatment process, the following techniques are used in different combinations.
- Surgery. Currently, organ-preserving schemes for performing operations are used. The affected bone is not amputated, but replaced with a graft, metal or plastic endoprosthesis. When a fragment of bone is removed, the underlying parts of the limb are preserved, thereby preserving its functionality, although to a limited extent.
- Alternative methods. Instead of surgical intervention for small tumor volumes, other methods are used - cryodestruction (freezing) of tumor tissue, injection of polymethylacrylate hot cement into the bone cavity, curettage of the tumor, etc.
- Radiation therapy. Ionizing radiation is used to destroy residual cells after surgery or in case of an inoperable tumor to reduce its size in order to prolong the patient's life. Radiation therapy is most successfully used to treat Ewing's sarcoma.
- Chemotherapy. Typically, cytotoxic drugs are used to treat Ewing's sarcoma and osteosarcoma.
- Targeted therapy. The patient is given specific medications that block the molecules of certain proteins necessary for the growth of malignant cells. Drugs are prescribed only after genetic molecular analysis confirms the presence of the desired protein.
- Treatment of metastatic bone cancer. To destroy metastases, the same chemotherapy drugs are used as to treat the primary tumor.

Classical medicine and treatment of aseptic bone necrosis.
Aseptic necrosis of bone has a high probability of making a person incapacitated (disabled), because often leads to complete destruction, for example, of the hip joint. What is the possible treatment? In the final stages of osteonecrosis of the bone, surgical treatment with total endoprosthetics of the affected joint is used. According to the American National Osteonecrosis Association and the Osteonecrosis Research Center, the average age of patients undergoing surgery for avascular osteonecrosis of the femoral head is 38 years. Given the relatively young age of such patients, it can be expected that some time after the first operation, a subsequent operation will be necessary to replace the prostheses. To try to stop the progression of necrosis and restore the structure of the femoral head, treatment such as forage alone or in combination with PRP, osteotomy, etc. must be carried out over a period of time. None of the listed methods has proven to be sufficiently effective in treating this disease. None of the currently proposed treatment methods for aseptic bone necrosis is aimed at eliminating the root cause disorders, namely restoring impaired blood circulation at the site of necrosis.
Rehabilitation
After surgery to remove a section of bone, recovery lasts about six months if amputation was performed, and about a year if an organ-preserving technique was used. Rehabilitation treatment includes a set of measures for proper bone fusion and healing of surgical wounds, restoration of mobility and function of the limb. Without these measures, the functions of the operated limb will be irretrievably lost in a short time. Complex and lengthy treatment is individual and depends on the extent of the surgical intervention.
What do tumors look like on photographs?
Typically, in photographs, various neoplasms stand out with their contours and are clearly visible against the general background. A malignant tumor can be identified by its heterogeneous structure, which has inclusions and compactions. And when viewed from different planes, it may look lumpy with some branches.
Important!
When performing an MRI, neoplasms on the bones should look like clear inclusions of round shapes with clear boundaries. With the lattice scanning method, the picture should be clearer. With the transverse scanning method, secondary tumors may appear in lighter colors, or even completely merge with the normal anatomical area. The introduction of a contrast agent will eliminate the problem and increase the brightness of the affected areas.

Otherwise, when scanning bones, the surrounding capillaries should be clearly visible. However, if the contours of the tumor are uneven, they can interfere with the view or even imitate the bifurcation of the tumor. When studying the results of an MRI examination of bones, the oncologist must pay attention to the condition of the lymph nodes, because they are the first to retain the affected cells when cancer occurs and are involved in malignant development.
How are metastases detected?
When metastases form, the patient remains fully functional without noticing any changes. To prevent new bone diseases, doctors recommend periodic examinations after surgery to remove a tumor (after undergoing cancer treatment).
Here diagnostics can be carried out using various methods:
- If an ultrasound or CT scan reveals problem areas where contours of an unclear nature are visible, then only they are subject to MR scanning.
- In the remission stage, it is recommended to undergo an examination of the whole body. It will help to identify new metastases, dense calcifications or bone tumors on MRI in a timely manner.

Diagnosis and treatment of bone cancer in Moscow
If you have symptoms of bone cancer, contact the Medicina clinic for a high-quality, reliable diagnosis, and if the diagnosis is confirmed, for treatment in accordance with high international standards. The clinic provides its patients with:
- performing any analyzes in our own well-equipped laboratory;
- examination using the latest diagnostic equipment;
- consultations and treatment with the best oncologists, surgeons, orthopedists, and rehabilitation specialists;
- stay in a comfortable hospital, care and service according to the standards of Western medicine.
Call us to schedule an initial consultation with your chosen specialist.
“White spots” and “white dots” on MRI - what are they?
Interpretation of MRI is an extremely complex and responsible matter, which is professionally performed by radiologists (radiologists). But often patients, after undergoing an examination, see some changes in the images themselves and wonder what they mean. This article was written to help such patients. The article will also talk about the benefits of a second opinion.
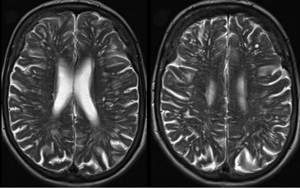
MRI OF THE BRAIN: WHITE SPOTS
One such question is what kind of white spots or dots are visible on MRI images of the brain. Normally, the structure of the brain is relatively homogeneous, but in various diseases, areas of the brain tissue are visible that differ in color (as diagnostic specialists say, in signal intensity) from the surrounding brain matter. In principle, any pathological changes are manifested in one way or another by a change in signal intensity on MRI images. Here we will look at the main causes of “white spots” on magnetic resonance imaging.
Get an MRI of the brain in St. Petersburg
1) Perivascular Virchow-Robin spaces, also known as criblures. What are perivascular spaces? These are accumulations of fluid along the vessels that penetrate the brain tissue. Normally, they are almost invisible, but if blood circulation is impaired, they can expand, causing a picture of “white dots” in the pictures. Perivascular spaces do not have much clinical significance and are quite common in healthy people. True, they are observed somewhat more often in people with labile vascular tone.
Multiple dilated perivascular spaces are a common finding on MRI, including in young adults. This is not a very dangerous condition, but requires consultation with a neurologist.
2) Multiple foci of demyelination in multiple sclerosis. This is a dangerous disease that requires immediate examination and treatment by a neurologist! The diagnosis of multiple sclerosis or another demyelinating disease can be confirmed or excluded only by carefully analyzing the results of a contrast-enhanced MRI and conducting some blood tests (in particular, an analysis for oligoclonal antibodies). Lesions of multiple sclerosis on MRI look different from criblures, but only a radiologist with extensive experience can reliably understand this.
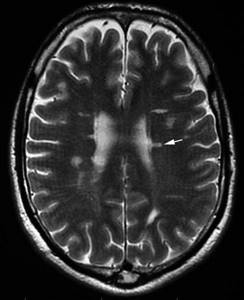
The location of hyperintense (increased MR signal) foci is characteristic of multiple sclerosis - in the white matter along the walls of the lateral ventricles. To confirm, a consultation with a neurologist is necessary, and if possible, obtaining a Second Opinion from an experienced neuroradiologist on MRI images.
3) Multiple “vascular” foci in dyscirculatory encephalopathy . In case of chronic cerebrovascular accident (due to atherosclerosis, hypertension, cervical osteochondrosis, etc.), areas in the form of white dots or spots also appear in the white matter of the brain. They have different names, including gliosis and leukoaraiosis. In most cases, they can be distinguished from multiple sclerosis by their location, the absence of accumulation of contrast agent, and some other signs. Unfortunately, sometimes it can be very difficult to distinguish between multiple sclerosis and dyscirculatory encephalopathy using MRI! In such cases, additional examinations, blood tests, and, if possible, a repeat MRI review with the involvement of an experienced radiologist are required.
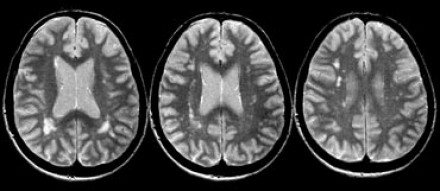
Multiple sclerosis or dyscirculatory encephalopathy (DEP)? In some cases, analysis of MRI images without in-depth knowledge of neuroradiology does not reliably differentiate these different conditions.
WHITE SPOTES ON MRI OF THE SPINE
In other cases, patients undergoing an MRI of the spine see “white spots” on the vertebrae. A natural question arises: what causes them and how dangerous it is.
1) Vertebral hemangioma. Single or multiple hemangiomas in the vertebrae occur in a quarter of patients, and in the absence of vertebral deformation they do not pose any danger and do not require special attention. If these formations look light on the images in both T1 and T2 modes, this is a sign of fatty replacement of hemangioma (angiolipoma, lipohemangioma) and the most favorable option.

A bright spot on a vertebra is a typical picture of a hemangioma. This is a benign formation and is not a true tumor.
3) Metastases in the vertebrae. Metastasis of cancer to the spine is a common condition in cancer of the prostate, lung, ovary or breast. Therefore, light or dark spots on an MRI of the spine may be due to malignant tumor screenings - metastases. Metastases in the vertebrae can be distinguished from hemanioma, fatty degeneration or a cyst by a number of signs - a bright signal in fat suppression mode, accumulation of a contrast agent, destruction or swelling of the cortical layer, a soft tissue component along the contours of the vertebra. Sometimes such differential diagnosis is very difficult and requires the opinion of an experienced radiologist.
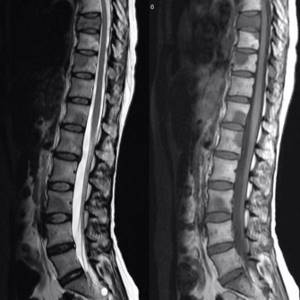
Dark spots on an MRI of the spine indicate metastases of prostate cancer in a young man. Consultation with an experienced specialist is required.
Get an MRI of the spine in St. Petersburg
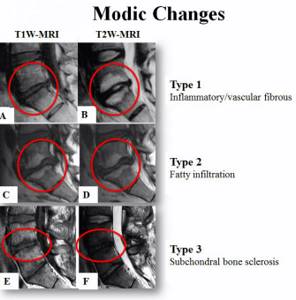
2) Fatty degeneration and bone marrow edema. Changes in the vertebrae during osteochondrosis - a degenerative-dystrophic disease of the intervertebral discs - are classified according to Modic. Depending on the predominant type of changes in the adjacent parts of the vertebrae (edema, fatty infiltration and osteosclerosis), types Modic 1, Modic 2 and Modic 3 are distinguished. This terminology is sometimes used to describe MRI of the spine. When interpreting images, it is important not to confuse these changes with metastases.
SECOND OPINION ON MRI
Even experienced doctors in difficult cases resort to the advice of colleagues, showing them MRI images in order to get a second opinion. After all, even the most experienced doctor cannot know everything, and sometimes an additional opinion of a specialist is required. For these purposes, Russia has created the National Teleradiological Network - a system for exchanging medical data, with the help of which you can get expert advice on the results of MRI, CT, PET and other modern examinations. Experienced radiologists from specialized centers in Moscow and St. Petersburg, such as the Institute of the Human Brain or the Military Medical Academy, conduct a thorough diagnosis of the submitted images and form an expert opinion. Any person, by going to the organization’s website, can order a remote interpretation of an MRI or CT scan of the brain, and receive an official report signed by a specialist.
Read more about Second Opinion
Read more about telemedicine
Pavel Popov
Candidate of Medical Sciences, Member of the European Society of Radiologists
Questions and answers
Is there a cure for bone cancer?
The success of bone cancer treatment depends on the stage of the tumor and the degree of aggressiveness of the malignant cells. It should be remembered that there is always a chance for recovery, even in the most advanced cases.
How long do people live with bone cancer?
Each case is individual, and the lifespan of a patient with bone cancer is largely determined by the type of tumor. With chondrosarcoma and osteosarcoma, up to 80% of patients live longer than five years after diagnosis of the disease.
How to detect bone cancer?
It is impossible to determine on your own that you have bone sarcoma. For an accurate diagnosis, it is necessary to undergo an examination, which includes a number of complex laboratory tests, X-ray and other studies. If you experience bone pain that lasts longer than two weeks, you should be examined by an oncologist to confirm the diagnosis or dispel your suspicions.
Attention! You can cure this disease for free and receive medical care at JSC "Medicine" (clinic of Academician Roitberg) under the State Guarantees program of Compulsory Medical Insurance (Compulsory Medical Insurance) and High-Tech Medical Care. To find out more, please call +7(495) 775-73-60, or on the VMP page for compulsory medical insurance
Treatment of aseptic bone necrosis at the Avatage Medical Center.
One of the new treatment methods that has emerged is the use of a shock wave, which can alleviate the condition at all stages of osteonecrosis of the head of the hip bone. This method is especially effective in stages 1 and 2 of the disease (corresponds to the Ficat and Arlet classifications) when complete recovery is possible. With the advent of shock wave therapy, the situation has changed radically. Many people ask how the SWT method contributes to the treatment of avascular necrosis of the femoral head? The answer is obvious; one of the key effects of shock wave therapy is the stimulation of angiogenesis (growth of new vessels) and osteogenesis. As a result, tissue renewal occurs at the site of exposure. Vascular collaterals and new capillaries are formed, which bring blood with nutrients and bone growth factors to the site of bone necrosis, thereby promoting the restoration of bone tissue structure.
Scientific works devoted to the use of ESWT in the treatment of aseptic bone necrosis.

The work showed extracorporeal shock wave therapy (ESWT) as a new therapeutic technology that can replace surgery in patients with aseptic necrosis of the femoral head (ONFH) without surgical risks. In animal experiments, ESWT has been shown to induce a cascade of biological reactions and molecular changes ranging from neovascularization to tissue regeneration.