Detailed description of the study
Human immunity is normally supported by different types of cells, the functions and structure of which differ markedly. One of them are neutrophils. They belong to the group of granulocytes. These cells play an important role in the development of inflammatory bowel diseases. Their main function is phagocytosis - the absorption of foreign harmful agents by the cell: bacteria, viruses and other pathogens.
During the inflammatory process, neutrophils infiltrate (“impregnate”) the intestinal wall with themselves. They synthesize and secrete a protein called calprotectin. It binds to calcium ions and becomes resistant to breakdown. Calprotectin suppresses some of the biochemical processes inside microorganisms and promotes their death. As a result, this protein is found in feces and is a marker of inflammation in the intestines.
Assessment of fecal calprotectin levels is widely used in the differential diagnosis of irritable bowel syndrome and inflammatory bowel disease (IBD). In addition, the analysis is carried out to monitor the activity of these diseases and monitor the effectiveness of their treatment.
Crohn's disease (CD) and ulcerative colitis (UC) are inflammatory bowel diseases. They are associated with the pathology of the immune system and are manifested by the formation of defects in the intestinal mucosa (ulcers and erosions). IBD develops in genetically predisposed people under the influence of certain environmental factors. Symptoms of Crohn's disease and ulcerative colitis can be different, the most common of them are:
- Abdominal pain;
- Diarrhea, sometimes mixed with blood;
- Loss of body weight.
Irritable bowel syndrome (IBS) is a disorder characterized by abdominal pain that occurs at least once every 7 days and is associated with changes in the patient's bowel habits and stool shape. These symptoms of IBS last for more than 3 months. The diagnosis of irritable bowel syndrome is usually made after excluding other diseases.
Testing for fecal calprotectin, if interpreted correctly, allows you to obtain preliminary data on the likelihood of inflammation in the intestines. The level of this protein in feces may reflect the activity of Crohn's disease and ulcerative colitis. In addition, the study is used as a lower cost method compared to colonoscopy or enterography.
The great advantage of the fecal calprotectin test is its non-invasiveness. This means that for the study there is no need to violate the integrity of any body tissues and to submit biomaterial after special complex preparation, which is an advantage when examining children and pregnant women. This test is included in Russian and international recommendations for the diagnosis and treatment of IBD in both adults and children. Its sensitivity for this pathology is 99%, and specificity is 97%.
Calprotectin. Is fecal calprotectin elevated? Don't panic!
Many patients with diseases of the gastrointestinal tract (GIT) are familiar with such an analysis as fecal calprotectin. This analysis is also known to doctors of various specialties. Why then is this article needed? It is necessary, I would even say necessary!
The widespread use of the method for assessing the level of fecal calprotectin in recent years has led to the emergence of various myths around this analysis. “Is the level of calprotectin in the stool increased? Do you have Crohn's disease or ulcerative colitis? Or this option: “Calprotectin is 3 (!) times higher than normal, what a severe inflammation in your intestines! Run to a gastroenterologist immediately!”
And patients come to the gastroenterologist, alarmed and frightened by the high numbers in the analysis and the already announced (albeit questionable) diagnosis. And the gastroenterologist has to explain the meaning of this study from the beginning.
So, let’s start with the basics.
What is calprotectin?
Calprotectin is a calcium- and zinc-binding protein belonging to the S-100 family of proteins. That is, the name of the protein has nothing to do with the word “feces”. This protein is concentrated predominantly in the cytoplasm of neutrophils, and (to a lesser extent) in monocytes and macrophages, which can be found in any human organ, but is mainly concentrated in the blood, cerebrospinal fluid, feces, saliva or synovial fluid.
Calprotectin is involved in various processes of the human body, including cell differentiation, inflammation processes, immune reactions, apoptosis, etc. Calprotectin plays an important role in inflammatory processes and is considered an acute phase protein of inflammation.
How and why is fecal calprotectin determined?
As we have already said, calprotectin can be contained in feces (in this case it is called fecal calprotectin, FC), and this fact is widely used in gastroenterology for the diagnosis of certain gastrointestinal diseases. Let me remind you once again that calprotectin is an inflammatory protein. Some pathological conditions (infection or inflammation of the intestinal mucosa of another origin) lead to an increase in the permeability of the mucous membrane and the movement of immune cells (neutrophils, macrophages) to the site of inflammation. They also cause the release of calprotectin from the cytoplasm of neutrophils. All this leads to the fact that the amount of calprotectin in feces increases significantly.
FA is resistant to digestion by enzymes of the gastrointestinal tract, as well as bacterial degradation. Its uniform distribution in stool and stability in stool (for 3 days at room temperature, 5-7 days at 4C0 and for a long time at -20C0) allows stool samples to be transported to a laboratory for analysis in any other country. The concentration of calprotectin in feces is determined by several laboratory methods, such as enzyme-linked immunosorbent assay (ELISA). This simple, non-invasive and less expensive (compared to colonoscopy) quantitative test is the most widely used marker for detecting and monitoring inflammatory activity in the intestines.
When does fecal calprotectin increase?
So, we have already seen that FC is used as a marker of intestinal inflammation. It is very important to understand what conditions can lead to an increase in it, and whether it is always a disease.
Let's start with the fact that calprotectin can be detected in the feces of absolutely healthy individuals. Cells containing calprotectin in their cytoplasm naturally die, and a small amount of this protein ends up in the feces. In such cases, FC is within the reference values (as laboratory standards are called). If the values of this indicator exceed the norm, then this requires additional assessment.
Thus, FC can be increased during acute bacterial (less often viral) intestinal infection. Sometimes it is higher than normal with celiac disease, acute appendicitis, taking non-steroidal anti-inflammatory drugs and proton pump inhibitors. A slight increase can be observed even with erosive and ulcerative lesions of the stomach and esophagus.

Finally, there is another group of diseases for which FC was introduced into clinical practice: inflammatory bowel diseases (IBD). IBDs include Crohn's disease (CD) and ulcerative colitis (UC). It went something like this: it was necessary to find a reliable marker that would allow the doctor to quickly and accurately distinguish an inflammatory process in the intestine from a non-inflammatory one. Why is this relevant?
For example, because irritable bowel syndrome (IBS) is very similar to CD in its clinical manifestations (abdominal pain and bowel movements). At the same time, every 15 people out of 100 inhabitants of the Earth suffer from IBS, and CD is much less common. How to distinguish between these diseases at the first stage of diagnosis? Should everyone get a colonoscopy? You can't save enough money: the cost of one colonoscopy with anesthesia and biopsy in Europe reaches 1,500 euros.
Studies have shown that with FA values below 50 μg/g, the likelihood of having active IBD is less than 1%. In clinical practice, I see approximately the same numbers - a rare patient with an exacerbation of UC or CD has a normal FC level. That is, if calprotectin values are normal and there are no alarm symptoms (fever, blood in the stool, etc.), most likely the patient's symptoms are not due to IBD.
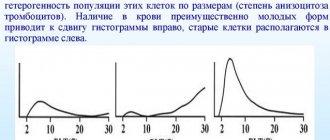
And what values will allow you to most reliably distinguish IBD from functional intestinal diseases? This is where the difficulties begin. Over the past ten years, many studies have been conducted to determine FC cutoff values above which a diagnosis of IBD is likely. Values range from 150 to 250 µg/g, but most expert communities have settled on figures >150 µg/g. In this case, significant inflammation in the intestine (if symptoms are present) should be considered and a colonoscopy should be discussed.
Will we always find IBD in the intestine even with FC values greater than 150 μg/g? Of course not! Firstly, no one can rule out a method error. Secondly, an increase in this indicator can be caused by the diseases described above and taking medications. Thirdly, high FC values can also be observed in other diseases that cause intestinal inflammation - diverticulitis, Behcet's disease, intestinal damage as part of vasculitis, etc.
Once a diagnosis of IBD is established, fecal calprotectin is well suited to assess intestinal mucosal healing and achieve endoscopic remission. Moreover, an increase in FC levels is observed before an exacerbation of the disease or during a postoperative relapse, and can help make a decision on timely adjustment of therapy.
Finally, I would like to discuss one more question: is a high level of calprotectin associated with the severity of inflammation in the intestine? Yes and no. On the one hand, there are studies that indicate that fecal calprotectin values of more than 250 μg/g are more often associated with the detection of large ulcerative defects of the colon mucosa in CD and UC. However, there is no information that 1000 mcg/g is much more pronounced inflammation than 250-300 mcg/g. In practice, one often encounters FA values of more than 1000 mcg/g, at which even ulcers are not always found in the intestine.
As a summary, my recommendations for assessing the level of FC:
- FA values may slightly exceed the norm of 50 mcg/g in healthy individuals. Re-evaluation of the indicator is required.
- A slight excess of FC compared to the norm can be caused by taking certain medications.
- High FC values do not help make a definite diagnosis, but only allow you to expand the patient’s examination plan. Elevated FC does not equal Crohn's disease or ulcerative colitis!
- Interpretation of stool FC test results should be done in conjunction with other tests based on the patient's symptoms.
- FC is a reliable marker for assessing intestinal healing during treatment in individuals with an established diagnosis of IBD.
References
- Clinical laboratory diagnostics: national manual: in 2 volumes - T. I. / ed. V.V. Dolgova, V.V. Menshikov. - M.: GEOTAR-Media, 2012. - 928 p.
- Livzan, M.A., Dolgikh, T.I., Lyalukova, E.A. Fecal calprotectin in the complex diagnosis of intestinal diseases. - EiKG, 2013. - No. 12.
- Ivashkin, V.T., Shelygin, Yu.A., Baranskaya, E.K. and others. Clinical recommendations of the Russian Gastroenterological Association and the Association of Coloproctologists of Russia for the diagnosis and treatment of irritable bowel syndrome, 2021. - T. 27(5). — P. 76-93.
- Russian Gastroenterological Association and Association of Coloproctologists of Russia. Clinical guidelines for the diagnosis and treatment of adult patients with Crohn’s disease, 2013. - 56 p.
Calprotectin in feces
Calprotectin is a protein produced in leukocytes; its concentration in the feces is directly proportional to the number of leukocytes entering the intestine. Determining the amount of calprotectin in feces is a test that allows diagnosing inflammatory bowel diseases.
Synonyms Russian
Fecal calprotectin, neutrophil protein, marker of intestinal inflammation.
English synonyms
Calprotectin, CALPRO, Stool Calprotectin, Calprotectin in human faeces.
Research method
Enzyme-linked immunosorbent assay (ELISA).
Determination range: 25 - 2500 µg/g.
Units
μg/g (micrograms per gram).
What biomaterial can be used for research?
Cal.
How to properly prepare for research?
- No special preparation is required.
General information about the study
In medical practice, determining the amount of calprotectin in a patient’s stool in conjunction with clinical manifestations is used to diagnose inflammatory bowel diseases.
The analysis is recommended if inflammatory bowel disease is suspected (detection of spasms, impaired intestinal motility, irregular stool with mucus in the patient, weight loss, fever, increased sweating, general weakness, increased fatigue, arthralgia, excessive bleeding in feces, perianal pathology). areas (fistulas, abscesses), constipation, pain in the right lower quadrant of the abdomen, around the navel, nausea, vomiting), if necessary, differential diagnosis with irritable bowel syndrome, other causes of abdominal pain, gastrointestinal bleeding.
Measuring the amount of calprotectin in a patient's stool sample is a simple, noninvasive way to diagnose inflammatory bowel disease, allowing physicians to distinguish this group of diseases from irritable bowel syndrome, in which there is no inflammation of the lining of the gastrointestinal tract.
Calprotectin is a neutrophil protein. Essentially, it is a protein bound to calcium. It makes up more than 60% of the total amount of proteins contained in the cytoplasm of neutrophil granulocytes (each neutrophil contains 25 picograms of calprotectin). Calprotectin is released from activated leukocytes, which leads to an increase in the concentration of this protein in the feces of inflammatory diseases of the corresponding organs.
Inflammatory bowel disease (IBD) occurs due to disruption of the host immune response and intestinal microflora. The main diseases belonging to this group are ulcerative colitis and Crohn's disease, which can affect the mucous membrane of any part of the gastrointestinal tract. There is a hereditary predisposition to the occurrence of IBD, and patients suffering from this pathology are more likely to develop malignant neoplasms.
There are a number of studies to confirm the diagnosis of inflammatory bowel disease, but none of these methods are specific, and the results should be assessed by a specialist in conjunction with examination data and the clinical picture. The main treatment for patients suffering from IBD is step-by-step symptomatic therapy aimed at healing defects in the mucous membrane of the gastrointestinal tract and preventing complications of the disease.
What is the research used for?
- To examine patients with suspected inflammatory bowel diseases;
- for differential diagnosis with irritable bowel syndrome, other causes of abdominal pain, gastrointestinal bleeding;
- for preventive examination of healthy people.
When is the study scheduled?
- If a patient has spasms, impaired intestinal motility, irregular stool mixed with mucus, weight loss, fever, increased sweating, general weakness, increased fatigue, arthralgia, developmental delay in children, excessive bleeding in feces, pathology of the perianal area (fistulas, abscesses), constipation, abdominal pain (in the right lower quadrant of the abdomen, around the navel), nausea, vomiting.
What do the results mean?
Reference values:
If the level of calprotectin in the patient’s stool is within the reference values, then he does not have inflammatory bowel disease.
A moderate increase in calprotectin levels requires further monitoring of the patient and dynamic testing. A strong increase (taking into account the clinical picture) indicates that the patient is suffering from inflammatory bowel disease, therefore, targeted examination and specific therapy are required. It can also be a consequence of the following pathological conditions: bacterial and viral infections of the gastrointestinal tract (salmonellosis, campylobacteriosis, adenoviruses, rotaviruses, noroviruses), intestinal neoplasms, diverticula, cystic fibrosis, allergies to cow's milk, celiac disease, intestinal bleeding.
Also recommended
- Fecal occult blood test
- Coprogram
- Carcinoembryonic antigen (CEA)
- C-reactive protein, quantitative (highly sensitive method)
- General blood analysis
- Leukocyte formula
- Erythrocyte sedimentation rate (ESR)
- Rheumatoid factor
- Antibodies to nuclear antigens (ANA), screening
Who orders the study?
Gastroenterologist, pediatrician, therapist, general practitioner.
Literature
- J. Walkowiak, S. Nousia-Arvanitakis, J. Henker, S. Stern, M. Sinaasappel, J. A. Dodge Indirect pancreatic function tests in children // J. Pediatr Gastroenterol Nutr, 40 (2) (2005), pp. 107–114.
- Aomatsu T, Yoden A, Matsumoto K, et al. Fecal calprotectin is a useful marker for disease activity in pediatric patients with inflammatory bowel disease. Dig Dis Sci. 2011 Aug;56(8):2372-7.
- Damms A, Bischoff SC. Validation and clinical significance of a new calprotectin rapid test for the diagnosis of gastrointestinal diseases. Int J Colorectal Dis. 2008 Oct;23(10):985-92.
- Jellema P, van der Windt DAWM, Schellevis FG, van der Horst HE: Systematic review: accuracy of symptom-based criteria for diagnosis of irritable bowel syndrome in primary care // Alimentary Pharmacology & Therapeutics 2009, 30(7):695-706 .
- Gisbert JP, McNicholl AG: Questions and answers on the role of faecal calprotectin as a biological marker in inflammatory bowel disease // Dig Liver Dis 2009, 41(1) : 56-66.
- Van Rheenen PF, Van de Vijver E, Fidler V: Faecal calprotectin for screening of patients with suspected inflammatory bowel disease: diagnostic meta-analysis // BMJ 2010, 341 : c3369.
Why is the concentration of a marker protein informative?
The body fights the infection, the protein begins to accumulate, and its increased concentration can be detected in the patient’s stool. Calprotectin disintegrates extremely slowly, which means it is easiest to detect when examining fecal matter.
The obtained data on protein will be directly proportional to the number of leukocytes “working” in the inflamed intestine.
An indicator for anti-infective treatment will be an excess of fecal calprotectin of more than 300 mcg/g. Such research data were obtained in 90% of patients with confirmed inflammatory processes in the intestines. It is important that if there are specific complaints from patients, such a protein test will help make a diagnosis without resorting to the unpleasant (albeit informative) colonoscopy procedure.
Who is he, the invisible “informant”?
Calprotectin is the result of the breakdown of leukocytes, a protein that is formed after the death of neutrophils and macrophages - the natural defenders of our body. It is leukocytes that are involved in the fight against inflammation, so their number exceeding the norm is very indicative for doctors.
Leukocytes are not detected in the feces, but what remains from the dead “defenders” - calprotectin, serves as a kind of litmus test that reacts to the presence of a focus of inflammation in the intestines.