T.M. Ignatova Clinic of Nephrology, Internal and Occupational Diseases named after. E.M. Tareeva MMA named after. I.M. Sechenova, Laboratory for the Study of Rheumatological Problems of Liver Diseases, Institute of Rheumatology, Russian Academy of Medical Sciences Clinical Hepatology, 2009, 2
During physiological pregnancy, a number of changes are observed, mainly in laboratory parameters (Table 1), which must be taken into account when assessing pathological conditions of the liver. Most of the changes (the appearance of “spider veins” on the skin, increased levels of bile acids, cholesterol, triglycerides in the blood serum, increased concentrations of coagulation factors) are due to the influence of increased levels of estrogen and progesterone, some (2-4-fold increase in the level of alkaline phosphatase (ALP) ), ceruloplasmin) – synthesis in the placenta. In addition, the increase in circulating blood volume (CBV) and the simple dilution effect cause a decrease in total protein and albumin levels. All of these deviations are most pronounced in the third trimester of pregnancy. The levels of bilirubin, γ-glutamyl transpeptidase (GGTP), serum aminotransferases (AST, ALT) and γ-globulins do not increase normally. There are no specific histological changes in the liver. Normalization of changed indicators occurs in the first 4-6 weeks after birth. Liver diseases observed during pregnancy are usually divided into three main groups:
Liver damage associated with pregnancy
- liver damage due to excessive vomiting during pregnancy;
- intrahepatic cholestasis of pregnancy;
- acute fatty liver of pregnant women;
- liver damage due to preeclampsia, eclampsia;
- HELLP syndrome.
Liver diseases not associated (combined) with pregnancy
- acute hepatitis of various etiologies (viral, drug, toxic);
- acute cholestasis caused by biliary obstruction;
- Budd-Chiari syndrome.
Chronic liver diseases preceding pregnancy
- chronic hepatitis and various liver cirrhosis;
- etiology (viral, drug, toxic;
- hereditary, autoimmune, etc.);
- familial non-hemolytic hyperbilirubinemia;
- liver tumors;
- extrahepatic portal hypertension (portal vein thrombosis);
- condition after liver transplantation, etc.;
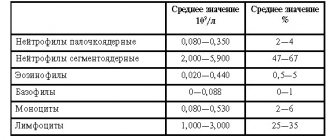
Changes in laboratory parameters during physiological pregnancy
| Indicators | Change in levels compared to normal | Trimester of maximum change |
| Total protein | Decline | II - III |
| Albumin | Decrease (by 20%) | II - III |
| γ-globulins | Normal or slight decrease | III |
| α-globulins | Promotion | III |
| β-globulins | Promotion | III |
| Cholesterol | Increase (1.5 - 2 times) | III |
| Triglycerides | Increase (3 times) | III |
| Alkaline phosphatase | Increase (2 - 4 times) | III |
| Bile acids | Increase (3 times) | III |
| Excretion of bromsulfalein | Slowdown | III |
| Bilirubin (conjugated) | Does not change or increases slightly | I - III |
| AST/ALT | Do not change | — |
| γ-GT | Doesn't change | — |
| Ceruloplasmin | Promotion | III |
| Transferrin | Promotion | III |
| Fibrinogen | Promotion | III |
| Coagulation factors VII, VIII, IX, X, | Promotion | III |
| Prothrombin index | Promotion | III |
| α-fetoprotein | Promotion | III |
These lesions develop only in pregnant women.
Liver damage due to excessive vomiting in pregnancy Excessive vomiting in pregnancy occurs with an incidence of 0.3% to 2%. It usually develops between the 4th and 10th weeks and stops before the 20th week of pregnancy. The condition leads to dehydration, electrolyte disturbances, weight loss, and protein catabolism. In 50-60%, transient functional changes in the liver may occur: a slight increase in the level of bilirubin, AST, ALT, alkaline phosphatase, a decrease in the level of albumin in the blood serum with a rapid normalization of these indicators after the cessation of vomiting and restoration of nutrition. Rarely, a significant increase in the activity of AST and ALT is observed, which requires the exclusion of acute viral (AVG) or drug-induced hepatitis, exacerbation of latent chronic liver disease (CLD) preceding pregnancy. There are no specific histological changes in the liver. The condition does not require termination of pregnancy. Intrahepatic cholestasis of pregnancy (ICP) is a relatively rare (from 1/1000 to 1/10000 births) condition, which, nevertheless, is the second most common cause (after ICH) of jaundice in pregnant women, causing up to 20-25% of cases of its development. ICP is based on a genetic predisposition to an unusual cholestatic response to estrogens and progesterones produced during pregnancy. Evidence has been obtained of the role of polymorphism of genes encoding proteins that transport bile components through the canalicular membrane of the hepatocyte or their nuclear regulatory proteins in the development of ICP. There is often a family history of itchy skin during pregnancy in the mother and sisters. The main clinical manifestation is skin itching, which usually appears in the third trimester (in 10% of cases in the first and in 25% in the second trimester of pregnancy), increases towards the end of pregnancy and disappears in the first two days after birth. May recur with repeated pregnancy and taking hormonal contraceptives. Skin itching precedes the appearance of mild (up to a 5-fold increase in bilirubin level) jaundice, which develops in only 20% of patients and is accompanied by darkening of urine and lightening of stool. The general condition of the patients does not suffer. A typical increase in alkaline phosphatase levels (7-10-fold) with a slight increase in the activity of AST/ALT (<300 U/l) and GGTP. The most sensitive test is to determine the level of bile acids in the blood serum. It increases 10-25 times with a change in the cholic/chenodeoxycholic acid ratio (4:1) compared to that observed normally (<1.5:1). Histologically, cholestasis is detected without hepatocellular necrosis and signs of inflammation. The prognosis for pregnant women is favorable. Increased risk of gallstones. ICP worsens the prognosis for the fetus: the frequency of premature births and stillbirths increases. Differential diagnosis includes obstructive jaundice, cholestatic form of AVH, drug-induced hepatitis, primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC). The greatest difficulty is in the differential diagnosis of ICP with the onset of latent PBC or PSC during pregnancy. Often, the disease can be recognized only after childbirth on the basis of persistent clinical and laboratory signs of cholestasis and the results of histological examination of the liver. Liver biopsy during pregnancy is usually not required, as it does not affect management tactics. It is aimed at reducing the manifestations of cholestasis, preventing premature birth and intrauterine fetal death. In ICP, the positive clinical and biochemical effect of ursodeoxycholic acid (UDCA) drugs at a dose of 1.5-2.0 g per day has been proven. Its use is safe for the fetus and significantly reduces the total level of bile acids in the blood serum, as well as in umbilical cord blood, amniotic fluid and colostrum. The use of UDCA not only relieves skin itching and improves the condition of the mother, but also significantly improves the prognosis for the fetus, reducing the incidence of premature birth and stillbirth.
Liver damage in preeclampsia, eclampsia In severe cases of gestosis (preeclampsia, eclampsia), liver damage is observed, the cause of which is microangiopathy as part of generalized vascular disorders. Spasm of arterioles and damage to the vascular endothelium with deposits of fibrin and platelets in them leads to ischemia, necrosis of hepatocytes and hemorrhages into the liver parenchyma. Signs of liver damage appear at the end of the second and third trimesters of pregnancy against the background of a detailed clinical picture of gestosis. Often only laboratory changes are observed (increased alkaline phosphatase, AST/ALT, slight thrombocytopenia).
HELLP syndrome is a rare (0.1-0.6% of pregnancies) complication that is considered as a variant of preeclampsia. It is observed in 4-12% of cases of its development. It is characterized by intravascular hemolysis (microangiopathic hemolytic anemia) - Haemolysis (H), increased levels of liver enzymes - Elevated Liver enzymes (EL), thrombocytopenia - Low Platelet count (LP). It develops, as a rule, from 27 to 36 weeks of pregnancy, in 25-30% - in the first 2 days after birth. Clinically, the condition is manifested by abdominal pain (in 65-90% of patients), nausea and vomiting (in 50% of patients), jaundice, complications of DIC syndrome, acute renal failure, and pulmonary edema. In some patients, arterial hypertension may be absent. The condition can be combined with acute fatty liver of pregnant women, which has been proven morphologically: in addition to fibrin thrombi in the sinusoids, centrilobular necrosis and hemorrhages characteristic of HELLP syndrome, small-droplet obesity of hepatocytes is often detected. A rare and very severe complication of liver damage is the formation of subcapsular hematomas with liver rupture and the development of intra-abdominal bleeding. Maternal mortality with HELLP syndrome is 1-5%, perinatal infant mortality (due to premature placental abruption, intrauterine hypoxia, prematurity) – from 7 to 23%. The main treatment method is urgent delivery, after which the symptoms of the disease regress and liver damage is completely reversible. It is rare that symptoms persist or intensify in the first two days after birth, which requires careful monitoring, correction of coagulopathy, plasmapheresis sessions, and hemodialysis.
Acute fatty liver (AFL) of pregnancy, or Sheehan syndrome, is a rare (1/7000 to 1/15000 births) severe complication of pregnancy. The etiology has not been definitively established. The development of CBD is predisposed by the first and multiple pregnancies, the male sex of the fetus, the development of preeclampsia, and the use of certain medications. In the pathogenesis of CBD in pregnant women, the main significance is the disruption of the process of β-oxidation of fatty acids in mitochondria, and therefore CBD in pregnant women is classified as a group of mitochondrial cytopathies, which includes Reye's syndrome, toxic reactions to certain drugs (sodium valproate, nucleoside analogues, tetracycline). The basis of liver damage in these diseases is the development of severe microvesicular steatohepatitis. Observations of CBD in pregnant women are associated with the identification of genetically determined deficiency of 3-hydroxyacyl-coenzyme A long-chain fatty acid dehydrogenase (LCHAD). Normally, heterozygous carriage of the defective gene in the mother does not lead to impaired β-oxidation of fatty acids. However, if she develops a fetus homozygous for the defective gene, then during pregnancy toxic long-chain fatty acids enter the mother's body through the placenta and their critical accumulation by the end of pregnancy, which leads to damage to hepatocyte mitochondria and liver damage. In the pathogenesis of CBD, the influence of internal (preeclampsia, in which an increased supply of fatty acids to the liver may be observed) and external (taking drugs that interfere with β-oxidation of fatty acids, a diet rich in fats) factors is also discussed. CBD usually develops between 30 and 38 weeks. It typically begins with nonspecific symptoms: vomiting (~80%), pain in the right hypochondrium or epigastrium (~60%), heartburn, headache, polydipsia. After 1-2 weeks, jaundice, fever, rapidly progressing liver failure, blood clotting disorders (DIC syndrome), and acute renal failure develop. Leukocytosis up to 20-30 x 109, a significant increase in the level of uric acid in the blood serum, severe hypoglycemia, a decrease in the protein-synthetic function of the liver, a moderate increase in the levels of bilirubin, AST, and ALT are detected. The condition is often associated with preeclampsia, can be combined with HELLP syndrome and is characterized by high mortality for the mother (up to 20%) and fetus (more than 20%). The disease may progress within 1-2 days after birth, then the condition improves. No specific therapy has been developed. As with HELLP syndrome, immediate delivery is indicated (caesarean section is preferable). Correction of coagulopathy, hypoglycemia and treatment of esophagitis, which is the most common source of bleeding, is carried out. As the condition progresses after childbirth, indications for liver transplantation may arise. The main causes of fetal death are the presence of genetic defects in fatty acid metabolism incompatible with life, as well as the development of hypoxia and asphyxia. Genetic testing of all newborns from mothers with a clinical picture of CBD is recommended for early detection of LCHAD deficiency in children and its dietary correction. Recurrences of CBD during repeated pregnancies are rare.
Liver diseases not associated (combined) with pregnancy Most of the acute liver diseases occur with equal frequency in pregnant and non-pregnant women, however, pregnancy may predispose to the development or more severe course of some of them (for example, cholelithiasis, Budd-Chiari syndrome, acute hepatitis, caused by herpes simplex virus, hepatitis E virus). In addition, pregnancy predisposes to the development of certain benign focal lesions due to hyperestrogenemia. Acute viral hepatitis (AVH) can develop at any stage of pregnancy. It causes 40-50% of cases of jaundice in pregnant women. In economically developed countries, the frequency of acute hepatitis caused by hepatitis A, B, C and D viruses (HAV, HBV, HCV, HDV), as well as their clinical course, do not differ from those in non-pregnant women. Signs of cholestasis may be more pronounced. Fulminant forms of AVH pose a danger to mother and fetus. OVH in pregnant women does not lead to an increase in the incidence of congenital malformations. When OVH develops at the end of pregnancy, there is a risk of infection of the child. Termination of pregnancy and childbirth aggravate the course of OVH, so management tactics are aimed at preventing premature birth. Specific prevention of infection of the child with HAV, HBV is carried out (administration of specific immunoglobulin and vaccine). Administration of the vaccine against hepatitis A and specific immunoglobulin against hepatitis A and B to pregnant women for preventive purposes is safe. AVH, caused by the hepatitis E virus (occurs sporadically in Russia), is characterized in pregnant women by a more severe (often fulminant) course and higher mortality (15-20%) than in the population (2-5%), a higher risk of spontaneous abortions and stillbirths, high incidence of perinatal infection of the child. Specific treatment and prevention have not been developed. In pregnant women, acute hepatitis caused by the herpes simplex virus is observed at a higher frequency than in the population. The disease is characterized by fever, herpetic rashes on the mucous membranes of the mouth or genitals, pain in the right hypochondrium, absence of jaundice with a very high level of AST/ALT activity. Without treatment, it is severe and characterized by high mortality. Antiviral treatment (acyclovir) is effective and leads to a significant reduction in maternal mortality.
Acute drug-induced hepatitis The drugs that cause drug-induced hepatitis and the clinical course of drug-induced hepatitis are the same as in non-pregnant women. A greater severity of the cholestatic reaction is possible. Severe liver damage has been described associated with the use of chlorpromazine for excessive emesis of pregnancy, tetracycline and nitrofuran derivatives for pyelonephritis. The use of drugs whose toxic effect affects mitochondria (sodium valproate, tetracyclines, nucleoside analogues) can provoke the development of CBD in pregnant women.
Gallstone disease, obstructive jaundice During pregnancy, the lithogenic properties of bile increase, the emptying of the gallbladder is disrupted, which predisposes to the formation of stones. Clinical manifestations, as well as management tactics, are the same as in non-pregnant women.
Budd-Chiari syndrome (acute hepatic vein thrombosis) is a very rare, but extremely severe prognosis complication. Hypercoagulation characteristic of pregnancy is a factor provoking the development of Budd-Chiari syndrome in women with previous thrombophilia of various origins. Thrombosis develops, as a rule, in the postpartum period and is manifested by abdominal pain, hepatomegaly, diuretic-resistant ascites, moderate increases in bilirubin, alkaline phosphatase, AST/ALT. Diagnosis and treatment measures for Budd-Chiari syndrome in pregnant women remain within the generally accepted framework.
Chronic liver disease in pregnant women Pregnancy may be preceded by any of the known diffuse CKD or focal liver lesions. The presence of CKD of various etiologies at the stage of hepatitis, as well as compensated liver cirrhosis without signs of portal hypertension, does not pose a significant risk to the mother and is not a contraindication to pregnancy. Timely diagnosis and treatment of CKD in women of childbearing age before pregnancy is especially important, since the presence of liver activity and severe cholestasis are risk factors for the development of exacerbation of the disease in connection with pregnancy, preterm pregnancy, and adverse outcomes for the fetus.
Chronic viral hepatitis (CVH) is the most common CKD in pregnant women. Pregnancy in patients with chronic hepatitis does not have an adverse effect on the course and prognosis of liver disease. ALT levels usually decrease or even return to normal during the second and third trimesters of pregnancy. At the same time, the level of viremia usually increases towards the end of pregnancy. Antiviral therapy is not recommended during pregnancy and breastfeeding due to the risk of negative effects on the fetus and newborn. The main problem associated with the presence of an active viral infection in the mother (both acute and chronic) is the risk of perinatal infection of the child with HBV and HCV. The risk of a child becoming infected if the mother has an HBeAg-positive HBV infection is 80-90%, and the risk of developing a chronic infection is 90%. In the absence of HBeAg, the risk of infection is significantly lower - 2-15%, and chronic infection rarely develops in infected children. From mothers infected with HBV and HDV, infection with HDV in the perinatal period is possible together with HBV, but the role of the perinatal route of transmission for HDV is extremely small. Infection of the child occurs mainly intrapartum, that is, during childbirth. In 5-15% of newborns from mothers with HBeAg-positive infection, infection occurs in the prenatal period (in utero). The effectiveness of specific passive-active immunoprophylaxis (vaccine against hepatitis B and specific immunoglobulin) exceeds 90%. However, it varies significantly in different regions and depends on the frequency of detection of HBeAg. The ineffectiveness of immunoprophylaxis in 10-20% of newborns from HBeAg carrier mothers is mainly due to intrauterine infection. The effectiveness and safety of the use of lamivudine in the third trimester of pregnancy has been shown to reduce the risk of perinatal infection from HBeAg-positive mothers with a high level of viremia. With HCV infection, the risk of perinatal infection does not exceed 5%. Infection, as with HBV infection, is predominantly intrapartum. The frequency and significance of intrauterine HCV infection have not yet been determined. Specific prevention of perinatal HCV infection has not been developed. The majority (80%) of children infected at birth develop chronic HCV infection. To reduce the incidence of hepatitis C in children, it is most appropriate to screen young women for the presence of HCV infection and conduct antiviral therapy before planning pregnancy. To date, there have been no compelling reasons to recommend cesarean section to reduce the risk of infection of the child with both HBV and HCV, but the contradictory results of available studies necessitate further study and clarification of recommendations. The presence of high-risk factors for intrapartum infection (high level of HCV or HBV viremia, multiple pregnancy, etc.) should be taken into account when discussing the method of delivery. HBV and/or HCV infection in the mother is not considered a contraindication to breastfeeding a newborn. Pregnancy, often repeated, is often observed in patients with autoimmune hepatitis, including at the stage of liver cirrhosis. Exacerbations of the disease during pregnancy are extremely rare. Disease activity usually decreases during pregnancy, allowing the dose of immunosuppressive therapy to be reduced. Observation and adequate therapy determine a favorable course and outcome of pregnancy. Exacerbations are common (about 80%) after childbirth, and therefore careful monitoring and adjustment of immunosuppressive therapy are necessary in the postpartum period. The use of glucocorticosteroids (GCS) is considered safe during pregnancy and lactation, however, there is a risk of having children with cleft palate (3.4 times higher than in the population) when using GCS (especially in high doses) in the first trimester of pregnancy. The safety of using azathioprine in the first trimester has not been fully determined (an increased risk of developing congenital heart defects cannot be ruled out), and therefore azathioprine, if possible, should be discontinued during pregnancy.
The course of primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC) during pregnancy is characterized by an increase in signs of cholestasis, usually in the II-III trimesters of pregnancy, sometimes after childbirth. These diseases are often manifested by itchy skin during pregnancy, which requires a differential diagnosis with ICP. Despite the relative rarity of PBC and PSC, their possible presence should be considered in all cases of cholestasis in pregnant women. An increase in signs of cholestasis leads to an increased risk of prematurity and stillbirth, which justifies the use of UDCA during pregnancy (at least in the second and third trimesters) as the main pathogenetic agent for these diseases. Observations of the use of the drug during the first trimester of pregnancy are not enough to draw conclusions about its complete safety.
Wilson-Konovalov disease (hepatocerebral dystrophy) is a rare genetically determined disease with predominant damage to the liver and central nervous system, which is based on excessive accumulation of copper. The disease develops at a young age and is accompanied by infertility and spontaneous abortion. Timely copper-eliminating therapy (drugs of D-penicillamine, zinc) for Wilson-Konovalov disease leads to restoration of liver function and reproductive function. Copper-eliminating therapy should be continued during pregnancy, the dose may be reduced in the third trimester of pregnancy. It is assumed that zinc preparations are safer for the fetus than D-penicillamine preparations.
Portal hypertension in patients with liver cirrhosis The presence of severe portal hypertension creates an increased risk of bleeding from esophageal varices (EVV), which reaches 25%. Bleeding occurs more often in the second or early third trimester of pregnancy, which is associated with the maximum increase in blood volume during this period. At the same time, a study conducted in Russia showed that bleeding from varicose veins most often developed in the early postpartum period (in the first 2 weeks). Observations of the development of bleeding from VUV during childbirth are extremely rare, and therefore the prevailing opinion is that vaginal birth does not increase the risk of bleeding. The tactics for managing pregnant women with bleeding are within the generally accepted framework. Maternal mortality reaches 50%. Careful risk assessment of possible pregnancy in patients with cirrhosis and, if necessary, surgical correction of portal hypertension or liver transplantation should be carried out before pregnancy. Pregnant women with a high risk of bleeding (URV >2 degrees, especially in the presence of inflammatory and trophic changes in the esophageal mucosa), as well as those with signs of liver failure and the development of hepatocellular carcinoma, are recommended to terminate pregnancy in its early stages (up to 12 weeks).
Conclusion During pregnancy, a number of liver diseases are observed - associated with pregnancy or combined with it. Timely diagnosis of liver damage and a thorough assessment of the degree of risk for the mother and fetus in each specific case is necessary to select the correct management and treatment tactics.
References 1. Benjaminov FS, Heathcote J. Liver disease in pregnancy. AmJ Gastroenterol., 2004, 99, 2479-2488. 2. Hay JE Liver disease in pregnancy. Hepatology, 2008, 47(3), 1067-1076. 3. Lee NM, Brady CW Liver disease in pregnancy. World J Gastroenterol., 2009, 15(8), 897-906. 4. Zapata R, Sandoval L, Palma J. et al. Ursodeoxycholic acid in the treatment of intrahepatic cholestasis of pregnancy. A 12-year experience. Liver Int., 2005, 25, 548-554. 5. Cappell MS Hepatic disorders affected by pregnancy: medical and obstetric management. Med Clin North Am., 2008, 92(4), 739-760. 6. Ibdah JA Acute fatty liver of pregnancy: an update on pathogenesis and clinical implications. World J Gastroenterol., 2006, 12 (46), 7397-7404. 7. Mukhin N.A., Nikonov A.P., Abdurakhmanov D.T. etc. Acute fatty liver of pregnancy. Clinical Hepatology, 2008, 4 (2), 40 45. 8. Gambarin-Gelwan M. Hepatitis B in pregnancy. Clin Liver Dis., 2007, 11, 945-963. 9. Ignatova T.M. Chronic liver diseases in pregnant women (literature review). Ter. arkh., 2002, 10, 55-59. 10. Tan J., Surti B., Saab S. Pregnancy and cirrhosis. Liver transpl., 2008, 14 (8), 1081-1091. 11. Ignatova T.M. Chronic hepatitis C and pregnancy. Clinical Hepatology, 2009, 5 (1), 32-38. 12. Pembrey L, Newel ML, Tovo PA, the EPHN Collaborators. The management of HCV infected pregnant women and their children. J Hepatol., 2005, 43, 515-525. 13. Hiratsuka M, Minakami H, Kochizuka S, Sato I. Administration of interferon-alpha during pregnancy: effects on fetus. J Perinat Med., 2000, 28, 372-376. 14. Roberts SS Assessing ribavirin exposure during pregnancy: the ribavirin pregnancy registry. Gastroenterol Nurs., 2008, 31 (6), 413-417. 15. Xu WM, Cui YT, Wang L. et al. Lamivudine in late pregnancy to prevent perinatal transmission of hepatitis B virus infection: a multicentral randomized double-blind, placebo-controlled study. J Viral Hepat., 2009, 16 (2), 94-103. 16. Ershova O.N., Shakhgildyan I.V., Kuzin S.N. and others. Characteristics of the activity of perinatal transmission of the hepatitis C virus. Epidemiology and infectious diseases: scientific and practical journal, 2005, 1, 39-41. 17. Zanetti AR, Tanzi E, Semprini AE Hepatitis C in pregnancy and maternal infant transmission of HCV. Congenital and other related infectious disease of the newborn. Isa K. Mushahwar (Editor). 2007, 153-171. 18. Yang J., Zeng XM, Men YL, Zhao LS Elective caesarean section versus vaginal delivery for preventing mother to child transmission of hepatitis B virus – a systematic review. Virol J., 2008, 5, 100-112. 19. Jonas MM Hepatitis B and pregnancy: an underestimated issue. Liver Intern., 2009, 29 (s1), 133-139. 20. Park-Wyllie L., Mazzotta P., Pastuszak A. et al. Birth defects after maternal exposure to corticosteroids: prospective cohort study and meta-analysis of epidemiological studies. Teratology, 2000, 62, 385-392. 21. Russel MA, Craigo SD Cirrhosis and portal hypertension in pregnancy. Semin Perinatol., 1998, 22, 156-165. 22. Rogachkova E.V., Eramishantsev A.K. Risk factors for bleeding from varicose veins of the esophagus and stomach in women with portal hypertension and pregnancy. Hepatology, 2004, 1, 14-19.
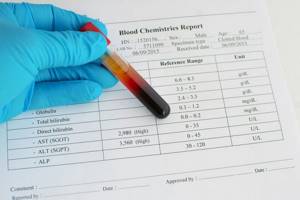
What does the term ALT mean?
When trying to decipher test results, many are faced with letter abbreviations, and the question often arises: what is ALT? As is known, this enzyme (alanine aminotransferase) serves as the main source of energy necessary to maintain the activity of the whole organism. It is difficult to talk about him in the singular, since together with him, AST takes an active part in the work of the bodies. These components are involved in the synthesis of amino acids such as alanine, which then becomes glucose.
ALT is involved in the functioning of not only the liver, but also the kidneys and heart. To obtain a reliable picture of the health status, the indicators of both enzymes (AST and ALT) are taken into account. They are like indicators that signal a problem. In addition, it may be necessary to assess the level of bilirubin, cholesterol, LDH, and alkaline phosphatase. This will allow us to establish a more accurate picture of the disease. In practice, the increase in liver enzyme levels occurs in the second or third trimester of pregnancy.
If any organ is damaged, the levels of these enzymes increase several times. And then they talk about increased ALT during pregnancy. This does not always immediately indicate an obvious problem or developing pathology. To monitor your health, a follow-up test is usually performed after taking medications. Only a specialist can prescribe them.
Available treatment in the third trimester
If ALT is increased during pregnancy in the 3rd trimester, then most likely the woman is accompanied by headaches, dizziness, nausea, and pain in the temporal region. These symptoms are characteristic of late gestosis and can cause quite significant discomfort. The load on the liver can be caused by the presence of diseases such as pancreatitis, heart disease, thyroid disease, genitourinary system, untreated infectious and inflammatory processes in the body. Definitely, this should not be ignored.
Treatment methods for elevated ALT in the blood during pregnancy come down to helping the liver perform its functions and recover. Therefore, any toxic drugs are excluded. Moreover, most of them are contraindicated for women during pregnancy. Doctors choose drugs that are made on a plant basis. These include: “Essentiale N”, “Tykveol”, “Gelabene”, “Legalon”. They protect the cells of the organ and restore it, and also perform functions that the liver cannot currently cope with. For example, this could be a secretory function, participation in metabolic processes, getting rid of toxic products.
How to prepare for analysis
Any medical procedures that a pregnant woman needs to undergo require preparation. The case of tests to determine the quality of metabolic processes is no exception. One of the most accessible ways to detect an increase in ALT during pregnancy is to donate blood for a biochemical analysis. Even at an early stage, you can get information about how the body reacts and behaves during pregnancy, whether the internal organs can cope with the increased load.
On the eve of the test, it is necessary to exclude from the diet:
- carbonated drinks and coffee;
- sweet, overly salty, fatty or spicy foods.
It is advisable to prepare porridge or vegetable salad for dinner. They are easy to digest and do not burden the stomach.
How to help a pregnant woman

The ALT level in women in the first trimester of pregnancy is considered a good indicator. This is due to the fact that not only hormonal changes occur, but also an active exchange of blood cells between the mother and the growing fetus. Only a qualified specialist can give a specific assessment of a woman’s health status.
If the reason for the increase in alanine aminotransferase levels is a lack of vitamin B, then restorative therapy is prescribed, which includes vitamins B and C, hepatoprotectors. It is also worth noting that normalizing the diet is one of the main ways to normalize ALT levels in the blood. It is believed that eating brown rice, fruits and vegetables, green or any herbal tea has a positive effect on restoring liver function.
The goal of treatment is not to reduce indicators, but to eliminate the inflammatory process, which leads to an increase in ALT during pregnancy. Only in this case can we talk about the possible restoration of the organ and health in general.
Diseases that accompany increased ALT
Only a qualified doctor can answer the question: “If ALT is elevated during pregnancy, what should you do?” Initially, you need to understand that you cannot do this with medications alone. This deviation is not typical for pregnancy. The norm indicators are influenced by many factors. Readings exceeding 32 IU/l are considered alarming.
If a discrepancy in ALT levels increases, it is important to determine the causes and only then select a treatment regimen. The main signs of diseases that can show an increase in the level of the enzyme in the blood:
- Toxic hepatitis: can develop not only as a result of alcohol and tobacco abuse, but also from working in hazardous industries or prolonged use of medications.
- Viral hepatitis: one of the most complex, transmitted by contact or through blood. It is insidious in that it may not show obvious signs of the disease for a long time. Hepatitis C is considered the most complex form.
- Liver cirrhosis refers to the most advanced form of the disease, when irreversible consequences have started in the body. Dead cells are no longer capable of recovery, and the prognosis in this case is not comforting.
However, it is always necessary to sensibly evaluate test results. Not a single case is taken into account, but to ensure the accuracy of the data obtained, the analysis is repeated. The duration of pregnancy is also of great importance. The duration of treatment is determined by the return to normal ALT in a pregnant woman.
Reasons for ordering the study

There are many terms in medicine, and it is not always immediately clear what ALT is and why its level needs to be monitored. In addition to the mandatory procedure for taking tests during pregnancy, as a result of the patient’s complaints or according to screening data, the doctor may suspect the presence of one or another abnormality. Despite the fact that most of the reasons for prescribing an extended blood test are common to many pregnant women, there are a number of symptoms that should alert you:
- pain symptoms in the chest area;
- dizziness, feeling of bitterness in the mouth;
- jaundice, increased levels of bilirubin in the blood, edema;
- decreased appetite, frequent belching;
- increased blood pressure, protein in the urine;
- vomiting and nausea in the last trimester;
- abdominal discomfort, fatigue.
We should not hush up the presence of these problems by attributing them to a special situation. They can become prerequisites for the development of a serious disease. Since not everyone knows what this means - an increase in ALT, it is necessary to obtain clarification from a competent specialist. In short, this enzyme is contained in several organs: skeletal muscles, heart, liver, kidneys.
Special diet

If ALT is elevated during pregnancy, diet is one of the key points for restoring health. It is quite affordable and simple; for example, it is recommended to replace the usual tea with herbal tea. It is worth paying attention to the composition and giving preference to dandelion, astragalus, and thistle. It is recommended to add turmeric and garlic as seasonings. These simple components help launch natural processes in the body that have antitumor and anti-inflammatory effects.
Among the dietary supplements, it is allowed to include antioxidants in the diet, which help the body rejuvenate cells and strengthen them. Nuts and avocados, mangoes and citrus fruits are quite affordable. Which also belong to the group of antioxidants. It is advisable to consume at least 50 g of dietary fiber per day, which serves as a natural “cleanser” of “bad” cholesterol.
The key is not only to eat healthy food, but also clean water. It is advisable to adhere to the daily norm and replace coffee and tea with it. If a woman does not take any vitamins during pregnancy, this may cause an increase in ALT during pregnancy. Why is this issue receiving so much attention? Because during the period when a woman is carrying a child, the body undergoes great changes and experiences increased stress. It is important not to miss the moment when you can help and restore the working capacity of important organs, in particular the liver.
The process of taking biomaterial for research and deciphering the results

Before you come to a medical facility for testing, you need to prepare. The day before, you should exclude dairy products and plant foods from your diet, including legumes, eggs, and sausages. On the day of delivery, you should refrain from eating so that the results are reliable.
The procedure for collecting blood occurs by taking it from a vein, so we can say that it is not painful. In order to eliminate the risk of hematoma formation, the injection site must be covered with a plaster or bandaged. The results are prepared almost immediately, but you can receive them the next day (if we are talking about a public clinic).
It happens that the standards differ in different clinics, so you should judge the results only after consulting a doctor. An increase in ALT by 2 times during pregnancy is considered uncritical, but if the numbers are increased by 5 times or more, then this is a reason for additional research (for example, ultrasound) and consultation with a specialist. In medical practice, a value has been established that clearly indicates the presence of pancreatitis or hepatitis; the deviation from the norm is 20 times higher.
Risk factors that lead to deviations from norms

It happens that a pregnant woman is prescribed certain medications, the use of which leaves behind specific enzymes in the blood cells. They can also cause an increase in ALT during pregnancy. Or this may be a consequence of the introduction of a catheter, which violates the integrity of the skin, and particles of the active substance of the drug remain in the blood.
Toxic components can easily cause damage and death of liver cells. There is a certain list of drugs that have a detrimental effect on the organ:
- hormonal drugs prescribed to maintain pregnancy;
- antibiotics, including those allowed during pregnancy;
- antifungal, antiepileptic, anticonvulsant;
- diuretics;
- non-steroidal dosage forms that have an anti-inflammatory effect.
The growing fetus puts pressure on the internal organs, which leads to disruption of the liver. Usually at the end of the second - at the beginning of the third trimester, due to compression of the gallbladder, bile stagnation occurs. Disruption of its natural outflow can also provoke an increase in ALT in the blood. If a pregnant woman suffers from diabetes, then while carrying a baby, her medications are replaced with insulin.
If a woman’s well-being does not change, but there is a deviation from the norm in the indicators of this enzyme, then weekly monitoring is necessary. However, when the opposite phenomenon is observed and the woman’s condition is close to critical, emergency delivery by cesarean section may be required.