Sugar levels during pregnancy
While carrying a child, many women begin to develop chronic diseases that did not make themselves felt before pregnancy.
This happens because the body has to work under increased stress. To track the slightest deviations from the norm, the gynecologist regularly prescribes tests. Expectant mothers donate blood for sugar twice: upon registration and at 24–28 weeks. Blood sugar levels during pregnancy:
- 5.8 mmol/liter when blood is taken from a vein
- 4.0–6.1 mmol/liter when taken from a finger
A slight increase in sugar levels, if it occurs against the background of hormonal changes during pregnancy, due to stress or overwork, is not considered critical. But if the blood glucose level exceeds 7.0 mmol/liter, then urgent measures must be taken, as this is a sign of diabetes. An accurate diagnosis can be made after repeated tests.
To ensure that the results are not erroneous, you must follow certain rules for preparing for analysis:
- donate blood in the morning on an empty stomach;
- do not brush your teeth with toothpaste or use chewing gum before visiting the clinic, as both products contain sugar;
- do not change your usual diet before taking tests, because this may affect the results obtained;
- take your last meal at least 8 hours before donating blood;
- drink still water.
It is important to remember that if during pregnancy your blood glucose level ranges from 5.1 to 6.9 mmol/liter, then there is no particular cause for concern. Gestational diabetes will go away after giving birth. But if the sugar level is 7.0 or more mmol/liter, a diagnosis of “manifest diabetes” is made. His treatment will have to continue after the birth of the child.
Treatment of diabetes in pregnant women
The first step in treating GDM is a balanced diet and moderate exercise.
The main goal of the diet is to reduce sugar to normal values, so the expectant mother will have to give up sweets and fast carbohydrates. Pregnant women are recommended:
- Eat little, but often.
- Exclude foods with a high glycemic index (sugar, honey, potatoes, white bread, baked goods, bananas, grapes).
- Avoid fast food and fatty sweet pastries.
- Drink enough fluids if there are no contraindications from the kidneys.
- Diversify your diet with fresh vegetables, lean meats, and cereals.
Like all pregnant women, it is important for patients with GDM to receive the full range of vitamins and minerals that are necessary to maintain their own health and the proper development of the fetus.
Walking, swimming, water gymnastics, physical therapy for pregnant women - any light activity will be beneficial.
If diet and exercise do not help lower blood sugar levels, insulin therapy is prescribed.
Important: with high sugar, a woman should check her glucose level daily. Measurements are taken on an empty stomach and an hour after each meal using a home glucometer.
High sugar during pregnancy
Most doctors believe that a glucose level of 6.9 during pregnancy is not a cause for concern - in this situation one can hope for normalization after childbirth. However, if sugar is elevated from 7.0 mmol/l or more, then a diagnosis of “manifest diabetes” is made. This means that the woman will remain ill after the birth of the child, and treatment will need to be continued.
Causes
High blood sugar occurs during pregnancy for several reasons:
- The kidneys have to work harder, so they sometimes do not have time to process the increased dose of glucose.
- Hormonal imbalance can also cause high blood sugar during pregnancy.
- A large load on the pancreas provokes gestational diabetes mellitus, which in most cases goes away 2-6 weeks after birth.
- Elevated glucose levels can be caused by diseases of the endocrine system, kidney or liver diseases before pregnancy.
Symptoms
This disease often occurs in a mild form. However, some symptoms should alert a pregnant woman, after which the woman should urgently consult a doctor. Among them:
- vision problems;
- constant thirst;
- regularly tormenting hunger;
- high blood pressure;
- general weakness, drowsiness;
- frequent and sometimes uncontrollable urination.
Indications for insulin therapy, recommendations of the Russian national consensus
Sulfonylurea drugs (glibenclamide, glimepiride) penetrate the placental barrier and can have a teratogenic effect, therefore they are not used for GDM.
- Failure to achieve target plasma glucose levels
- Signs of diabetic fetopathy by ultrasound (indirect evidence of chronic hyperglycemia [13])
- Ultrasound signs of diabetic fetopathy:
- large fetus (abdominal diameter greater than or equal to the 75th percentile);
- hepatosplenomegaly;
- cardiomegaly and/or cardiopathy;
- dual-circuit head;
- swelling and thickening of the subcutaneous fat layer;
- thickening of the neck fold;
- newly identified or increasing polyhydramnios with an established diagnosis of GDM (if other causes are excluded).
When prescribing insulin therapy, a pregnant woman is treated jointly by an endocrinologist (therapist) and an obstetrician-gynecologist.
What does high blood sugar mean during pregnancy?
At the first visit to the antenatal clinic, the expectant mother receives from the doctor a referral for tests that allow her to assess the general condition of the pregnant woman. One of the most significant indicators in this huge list is the determination of blood glucose. If it is discovered that sugar is elevated during pregnancy, the woman will be asked to undergo additional examination, as well as a course of treatment if necessary.
- Blood sugar is normal in the evening, but elevated in the morning: why does this happen?
An increase in blood glucose concentration is not at all as harmless as it might seem at first glance. A change in sugar levels triggers a whole complex of pathological mechanisms that lead to a significant deterioration in the condition of a pregnant woman. The processes occurring in the body of the expectant mother will inevitably affect the development of the fetus, increasing the risk of having a child with signs of diabetic fetopathy.
Management of patients with GDM
Within 1–2 weeks after diagnosis, the patient is advised to be monitored by obstetricians-gynecologists, therapists, and general practitioners.
Rules for conducting an oral glucose tolerance test (OGTT)
- The test is carried out against the background of normal nutrition. At least 150 g of carbohydrates should be consumed per day for at least three days before the study.
- The last meal before the test should contain at least 30–50 g of carbohydrates.
- The test is performed on an empty stomach (8–14 hours after eating).
- Drinking water before the test is not prohibited.
- You are not allowed to smoke during the study.
- The patient must sit during the test.
- If possible, on the eve of and during the study, it is necessary to avoid taking medications that can change blood glucose levels. These include multivitamins and iron supplements, which contain carbohydrates, as well as corticosteroids, beta blockers, beta adrenergic agonists.
- OGTT should not be performed:
- with early toxicosis of pregnant women;
- if necessary, on strict bed rest;
- against the background of an acute inflammatory disease;
- with exacerbation of chronic pancreatitis or resected stomach syndrome.
Recommendations for a pregnant woman with diagnosed GDM according to the Russian national consensus:
- Individual correction of the diet depending on the woman’s body weight and height. It is recommended to completely eliminate easily digestible carbohydrates and limit the amount of fat. Food should be distributed evenly over 4-6 meals. Non-nutritive sweeteners can be used in moderation.
For women with a BMI >30 kg/m2, average daily caloric intake should be reduced by 30–33% (approximately 25 kcal/kg per day). It has been proven that this measure can reduce hyperglycemia and plasma triglyceride levels [12].
- Aerobic physical activity: walking at least 150 minutes per week, swimming.
- Self-monitoring of key indicators:
- glucose level in capillary blood on an empty stomach, before meals and 1 hour after meals;
the level of ketone bodies in urine in the morning on an empty stomach (before bedtime or at night, it is recommended to additionally take carbohydrates in an amount of about 15 g for ketonuria or ketonemia);
- arterial pressure;
- fetal movements;
- body mass.
In addition, the patient is recommended to keep a self-monitoring diary and a food diary.
Reasons for the increase
A wide variety of causative factors can lead to an increase in glucose in the female body during pregnancy. Quite often it happens that they act simultaneously, enhancing each other’s effects. Doctors call a persistent increase in blood glucose hyperglycemia.
According to statistics, 5% of pregnant women develop gestational diabetes mellitus while carrying babies. This pathology is accompanied by constant elevated blood sugar levels. This disease can be dangerous for both the mother and her baby.
For a long time, researchers have been trying to establish why the risk of developing diabetes mellitus increases so significantly during pregnancy. The main reason turned out to be related to altered hormonal levels.

Metabolites of progesterone, as well as other pregnancy hormones, have a pronounced effect on metabolic processes, including the metabolism of glucose in the body.
A change in the concentration of certain hormones in the blood of a pregnant woman leads to the phenomenon of insulin resistance. This condition causes blood glucose levels to increase.
Sugar levels rise almost constantly with this pathology. The severity of the disorders depends largely on how much the hormonal levels are changed, and whether the woman has any concomitant diseases of the internal organs.

- Maximum blood sugar level in diabetes in a diabetic: normal limits
Quite often it happens that the blood sugar level of the expectant mother begins to rise in the second half of pregnancy. This feature is largely due to altered kidney function. The growing uterus puts pressure on these urinary organs, leading to congestion in them.
A decrease in the excretion of glucose by the kidneys contributes to its accumulation in the blood, which also increases the manifestations of hyperglycemia. In this case, an increased concentration of sugar is also determined in the urine when it is submitted for testing to the laboratory.
Glucose appears when its concentration in plasma is above 9 mmol/l. This situation is extremely unfavorable and requires urgent medical correction.
Pancreatic diseases are another common cause leading to the development of gestational diabetes mellitus.
Such diseases usually appear even before pregnancy.
Chronic pancreatitis, which occurs with frequent exacerbations, can contribute to the development of persistent hyperglycemia during pregnancy. In this case, treatment cannot be avoided.
Scientists have found that heredity plays a huge role in the development of persistent hyperglycemia. In women with a family history of diabetes, the risk of developing the gestational variant increases by 50%.
All expectant mothers with risk factors must be observed by a therapist. Women who already suffer from diabetes mellitus or frequent episodes of hyperglycemia are monitored by an endocrinologist, including during pregnancy.
Many concomitant diseases of internal organs can also cause the expectant mother to develop persistent hyperglycemia. This is usually caused by persistent pathologies of the liver, gall bladder, metabolic disorders in the endocrine system, and chronic kidney disease. Injuries to the gastrointestinal tract or previous surgeries can also contribute to an increase in blood glucose.
Scientists have found that prolonged prolonged stress has a negative impact on the functioning of the endocrine system. This is manifested by a persistent increase in blood sugar.
- How is blood sugar measured: units and designations
Many pregnant women note that they experienced hyperglycemia for the first time after some severe stress in life. During pregnancy, exposure to even a slight intensity is sufficient to increase blood sugar.
Calculate gestational age
Reviews from women who experienced increased sugar in their urine during pregnancy
At least 10% of women experience gestational diabetes during pregnancy, so there are a lot of reviews on this problem on the Internet.
Many of us know people who suffer from diabetes. During pregnancy, the manifestations of this disease are especially dangerous, because it will spread to two organisms at once (if diabetes is not compensated). That is why, during the period of bearing a child, it is important for a woman to undergo all the necessary tests on time and be sure to check the sugar level in the urine. If you are at risk, then even before conception you should visit an endocrinologist. Only in this case will the pregnancy pass without complications, and the child will be born healthy.
Hello! My name is Valentina. I am 29 years old. An engineer by education. Rate this article: Share with friends!
Why is sugar dangerous during pregnancy?
First of all, excess glucose can lead to fetal pathology. These babies are born very large. In addition, they are at risk of developing neurological diseases, jaundice, respiratory problems, and mental retardation.
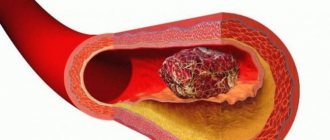
But the most serious consequence of high sugar is miscarriage. Medical statistics indicate the risk of losing a child in most cases precisely with high sugar levels. With excess glucose, blood vessels are primarily affected. They do not supply blood and nutrients to the placenta in the required volume, which leads to its “drying out,” which is the cause of premature birth.
Moreover, a pregnant woman suffers:
- swelling;
- overweight;
- high blood pressure;
- deterioration of vision, which increases the risk of retinal detachment;
- the occurrence of inflammatory processes in the genitourinary system due to increased proliferation of bacteria in a sweet environment;
- in 60% of cases, the expectant mother develops excess amniotic fluid.
It is very important to periodically visit a doctor who monitors the progress of pregnancy in a particular woman. She should undergo all research procedures and adhere to the gynecologist’s recommendations.
Diabetes mellitus during pregnancy
Gestational diabetes mellitus (GDM) is a condition in a woman in which her blood sugar levels become high during pregnancy and then return to normal after childbirth.
What leads to the development of GDM?
In the second half of pregnancy, the level of hormones increases, the action of which is opposite to the effects of insulin, i.e. they provide an increase in blood sugar levels. Usually, the mother's insulin reserves are sufficient to maintain normal sugar levels, but in the presence of factors such as obesity, hereditary predisposition to diabetes, decreased physical activity, the action of insulin becomes insufficient, and blood sugar levels rise above normal.
What is the danger of developing GDM if left untreated?
High blood sugar levels in a pregnant woman lead to changes in the vessels and walls of the placenta, the development of diabetic fetopathy of the fetus (intrauterine increase in body length, increase in the size of the liver and spleen, swelling of tissues and subcutaneous tissue, impaired development of lung tissue and, as a consequence, intrauterine fetal hypoxia) . All this increases the risk of developing preeclampsia (swelling and increased blood pressure in a pregnant woman).
Who may develop GDM?
High risk of developing gestational diabetes mellitus: presence of diabetes in relatives, overweight/obesity, previously documented disorder of carbohydrate metabolism (impaired glucose tolerance), glucosuria (increased sugar levels in the urine) during this pregnancy, age over 30 years
How to find out if a pregnant woman has GDM?
To diagnose GDM, blood sugar levels are determined - a test with 75 grams of glucose. The sugar level is measured on an empty stomach, and then 1 hour and 2 hours after taking the glucose solution. Blood is taken from a vein, and the sugar level in the blood plasma is determined.
Gestational diabetes is diagnosed if fasting sugar is from 5.1 to 6.9, 1 hour after taking glucose - up to 10 or higher, and after 2 hours - from 8.5 to 10.9.
If these indicators are above 7.0 on an empty stomach and 11.0 after taking glucose, then newly diagnosed diabetes mellitus is diagnosed.
What to do if a doctor diagnoses GDM?
If GDM is diagnosed, it is important to understand that the condition is temporary and will most likely resolve after delivery. Therefore, all recommendations will relate to the period remaining before childbirth.
Firstly, it is necessary to review the diet and exclude those products in the preparation of which sugar (honey, molasses), starch, premium flour, as well as products that have undergone intensive culinary processing (puree, boiled, instant products) are used. In them, glucose is in an easily accessible form, their consumption will lead to a rapid increase in blood sugar levels, and the insular apparatus will not have time to produce the required amount of the hormone (this is why blood sugar increases 1 hour after eating, which is harmful for the baby).
Secondly, you need to move more, because muscle is the main consumer of glucose, which actively consumes blood sugar. You can swim, walk, attend sports classes for pregnant women, do simple exercises with your arms and legs within the limits of what your obstetrician-gynecologist allows. Any muscle can work to lower glycemic levels.
Third, monitoring is needed to evaluate efforts to reduce blood sugar levels to normal. You need a glucometer that is calibrated for plasma (Accu-Chek, Van Touch.) to independently determine blood sugar. (To measure, you need a very small drop of blood, which is obtained with a special lancer with a thin needle that is not even visible). Typically, the doctor prescribes monitoring before and 1 hour after main meals and at night. Before meals, sugar should be up to 5.0 mmol/l, and 1 hour after meals up to 6.9 mmol/l. It is with these indicators that the fetus will not receive excess sugar and will not experience complications. It is important to record all your self-monitoring results or mark them with special symbols in the meter's memory.
Fourth, it is necessary to measure the level of acetone in the urine, because when there are excessive restrictions on the intake of carbohydrates in the pregnant woman’s body, she can produce ketone bodies, which compensate for the lack of energy, but are toxic substances. If there is acetone in the urine, you should inform your doctor; most likely, a decision will be made to take additional carbohydrates before bed (for example, kefir and a piece of bread)
How to follow a diet for GDM?
Can be consumed without limitation: mushrooms, raw vegetables, legumes, cheeses, beef, poultry, fish, seafood, eggs.
It is necessary to reduce the usual portion by half: unsweetened fruits and berries, liquid dairy products, cereals and pasta.
In general, the more chopped or processed a carbohydrate product is, the faster it will raise your blood sugar levels.
You should not overuse animal fats, although they will not affect your blood sugar levels.
What to do if, during self-control, high sugar levels persist, despite the diet?
Unfortunately, this happens. It is important to inform the doctor about this in a timely manner, without relying on the fact that this is accidental, and tomorrow there will be different numbers during self-monitoring. The doctor will prescribe insulin (select it based on self-control indicators). Unfortunately, you cannot take any diabetes pills during pregnancy. Don't be afraid, it's only for a few months. After birth, insulin will be stopped. But it is important to follow this recommendation in order to carry and give birth to a healthy baby on time, and not suffer from complications.
How does childbirth occur with GDM?
They are usually delivered through the natural birth canal. The decision on a cesarean section is made taking into account obstetric indications (as for women without GDM). Patients on insulin are hospitalized in advance in a special maternity hospital, again in the interests of the child, so that he receives the right help if it is needed.
What happens after childbirth?
After giving birth, insulin will be stopped and you will not need to strictly follow a diet. However, 2-3 months after birth, you need to repeat the glucose test (on an empty stomach and 2 hours after taking 75 g of glucose) using capillary blood (from a finger) or blood plasma (from a vein). Based on the results, the doctor will advise you on what to do next.
If GDM was detected during a previous pregnancy, is it still possible to plan a pregnancy?
It’s possible, but you need to plan it. Take care in advance of losing weight, stop eating a lot of sweets, and get used to leading a healthy lifestyle. During pregnancy, monitor your blood sugar. All this will help avoid recurrence of GDM or make its course milder.
Be healthy!

about the author
- Ivlieva Evgenia Sergeevna
- Endocrinologist of the first category
- All publications by the author