The capabilities of the laboratory of the Medical Women's Center on Zemlyanoy Val make it possible to perform a comprehensive diagnosis of chronic and systemic kidney diseases: pyelonephritis, renal artery stenosis, renal failure. Thanks to the use of highly sensitive analyzers and specialized test systems, we are able to identify signs of pathological processes even during a latent course.
In addition to laboratory tests, our clinic conducts intravital examination of renal tissue - puncture biopsy with histology.
What tests to take for kidney failure
- General urine analysis
- Bakposev
- General blood analysis
- Blood biochemistry
The density, color of urine, and the presence of sediment are assessed. The level of functional renal impairment is determined. The presence of eosinophils is interpreted as a sign of an allergic reaction, including to medications.
Cultural analysis is aimed at searching and classifying the causative agent of infection - a possible cause of renal dysfunction. Necessary for the selection of effective antibiotics.
In acute or chronic renal failure, the level of leukocytes in the blood increases, and the number of red blood cells and hemoglobin decreases significantly. An increase in the ESR index indicates the development of an infectious or inflammatory process.
Creatinine levels control blood flow to the kidneys. During the latent period, its concentration is 0.702-0.352 mmol/l, in the severe stage - 0.702-1.055 mmol/l.
Impaired kidney function is accompanied by an increase in nitrogenous metabolic products in the blood, a decrease in the amount of calcium and sodium, vitamin D, and an increase in the level of glucose, potassium, and phosphorus.
Chronic renal failure
Chronic renal failure (CRF) is a gradual deterioration of kidney function over a long period of time. In modern literature, the term “chronic kidney disease” is found, which has a slightly broader meaning and implies a decrease in kidney function for three months or more.
The function of the kidneys is to maintain a normal balance of fluids and salts in the body, as well as to remove protein metabolic products (nitrogenous waste) from the body, forming urine. With chronic renal failure, blood purification does not occur sufficiently, which over time can lead to serious complications.
In the early stages of chronic kidney failure, there may be no symptoms. The disease is often discovered when kidney function deteriorates significantly.
It is very important to diagnose ESRD as early as possible in order to promptly begin treatment to slow the rate of decline in kidney function, since long-term kidney damage is irreversible. Without treatment, kidney function may deteriorate critically, which may require hemodialysis (artificial blood purification using an artificial kidney machine).
In some cases, the only treatment for a patient with chronic renal failure may be a kidney transplant.
Synonyms Russian
Chronic kidney disease, chronic renal failure, CKD, kidney shrinkage, nephrosclerosis, uremia.
English synonyms
Chronic Renal Failure, Chronic Kidney Disease, Chronic Kidney Failure, Chronic Renal Disease, CRF, CKF, CKD, CRD, Uremia.
Symptoms
Signs and symptoms of kidney failure may not appear for a long time. Symptoms can vary and include:
- nausea, vomiting, loss of appetite;
- frequent night urination;
- fatigue, fatigue;
- dry, pale skin, persistent itching;
- high blood pressure (hypertension);
- muscle twitching, tingling in different parts of the body, convulsions;
- bleeding from the gastrointestinal tract, gums, nose;
- perversion of taste;
- decreased libido, amenorrhea (lack of menstruation);
- swelling of the feet and ankles;
- decrease in intellectual activity.
Signs and symptoms of chronic renal failure are nonspecific, meaning they can occur in other diseases.
General information about the disease
Chronic kidney failure is a condition characterized by gradual deterioration of kidney function over months or years.
CRF is an important medical problem. Millions of people around the world suffer from this disease, and the number of cases is steadily increasing every year. There are 300-500 patients with chronic renal failure per million adults.
The kidneys are the main organ of the human excretory system. Normally, they maintain the ratio of water and active substances in the body, regulate the volume and composition of blood plasma. In addition, they produce a number of hormones - biologically active molecules.
Filtration of blood in the kidneys is carried out due to the functioning of the renal glomeruli. Each kidney contains a million glomeruli. Each renal glomerulus is a plexus of capillaries, in the form of a glomerulus, surrounded by a capsule. Passing through the glomeruli, the liquid part of the blood is filtered, after which primary urine is formed. The glomeruli normally allow only the liquid portion of the blood to pass through—proteins and other large molecules do not pass through the kidneys.
Next, primary urine enters the renal tubules - thin tubes in the kidneys. In the renal tubules, most of this fluid is reabsorbed (a process called reabsorption), and a small portion passes as urine into the renal pelvis, and then into the ureter and bladder. When enough urine has accumulated in the bladder, it is expelled from the body during urination.
About 150 liters of fluid pass through the kidneys per day, from which 1.5-2 liters of urine are formed. This is how the composition and volume of plasma is regulated.
In chronic renal failure, due to various reasons, the kidney tissue is replaced by scar tissue, the structure of the kidneys changes, the area of healthy tissue decreases, as a result of which the volume of filtered blood gradually decreases. At the same time, the remaining glomeruli and tubules hypertrophy, enhancing their function to compensate for this condition. Losing 75% of kidney tissue results in only a 50% reduction in blood filtration volume.
As a result, the volume of blood filtration decreases, the ratio of water and salts (electrolytes) in the body is disturbed, which is manifested by nausea, vomiting, muscle twitching, fluid accumulates in the tissues, which is manifested by edema, shortness of breath (due to the accumulation of fluid in the lungs). The density of urine decreases, it becomes lighter, and the patient begins to be bothered by frequent night urination.
Over time, the concentration in the blood of nitrogenous wastes (urea and creatinine) - the main end products of protein metabolism - increases significantly, which only serves as a sign of deterioration in kidney function, but does not manifest itself in any symptoms. An increase in urea leads to nausea, abdominal pain, and headache. Other nitrogenous wastes lead to persistent skin itching.
Symptoms of chronic renal failure do not appear immediately due to the large compensatory capabilities of the kidneys. Even with moderate kidney failure, there may be no symptoms.
Kidney failure can develop after a variety of diseases that damage the kidneys. The most common reasons for this are:
- diabetes mellitus type 1 or 2;
- high blood pressure (arterial hypertension);
- atherosclerosis – deposition of cholesterol in the walls of the renal arteries, preventing normal blood flow in them;
- glomerulonephritis is a group of diseases that have different causes, common to which is inflammation at the level of the renal glomeruli;
- urolithiasis – the appearance of kidney stones;
- chronic pyelonephritis – chronic inflammation of the kidney tissue;
- tuberculosis;
- polycystic kidney disease is a hereditary disease manifested by the formation of cavities in the kidney tissue (cysts);
- long-term blockage of the urinary tract, which can occur with adenoma or prostate cancer.
In recent years, instead of the term “chronic renal failure,” the term “chronic kidney disease” has increasingly been used, which implies a decrease in kidney function for three months or more. Chronic kidney disease is classified into five stages depending on the degree of impairment of glomerular filtration. The first 2 stages indicate mild renal dysfunction. The third, fourth and fifth stages correspond directly to renal failure itself. The last stage is called the terminal (final) stage. The final stage of chronic renal failure, when kidney function is critically reduced and the patient is bothered by many complaints, is called uremia.
Chronic renal failure can lead to the development of a wide range of different complications:
- Anemia. Normally, the kidneys produce the hormone erythropoietin, which stimulates the formation of red blood cells (the main blood cells that carry oxygen from the lungs to organs and tissues) in the bone marrow. As the area of healthy kidney tissue decreases, the production of erythropoietin and red blood cells decreases, anemia occurs (decrease in the level of red blood cells and hemoglobin in the blood), which is manifested by weakness and fatigue.
- Pericarditis is the accumulation of fluid in the lining surrounding the heart (pericardium). This condition can threaten the normal contractions of the heart and lead to the death of the patient.
- Encephalopathy. The term encephalopathy refers to a condition associated with the toxic effects of nitrogenous waste on the brain. In severe cases, this can lead to coma.
- Ulcers of the gastrointestinal tract, which can lead to spontaneous bleeding.
- Bone damage. Almost all patients with chronic renal failure have impaired calcium and phosphorus metabolism, which leads to softening of the bones and an increased risk of fractures.
- Heart or pulmonary failure. Fluid retention in the body with chronic renal failure can lead to the development or aggravate heart or lung failure, manifested by shortness of breath and edema.
- Myocardial infarction, stroke. CRF accelerates the progression of atherosclerosis, a condition in which cholesterol plaques are deposited in the walls of arteries, which can restrict blood flow through the vessel. If this occurs in the heart arteries, damage to the heart muscle occurs (myocardial infarction), and blockage of the brain vessels leads to a stroke - an acute circulatory disorder in the brain.
- Increased levels of potassium in the blood (hyperkalemia) can lead to arrhythmia, an abnormal heart rhythm that threatens the patient's life.
- A decreased immune response makes the patient more vulnerable to infections and other diseases.
- Restless legs syndrome. A condition associated with unpleasant sensations in the legs, which force a person to constantly move them.
- Complications of pregnancy that are dangerous for the fetus and mother.
In most cases, chronic renal failure progresses steadily and irreversibly until the terminal stage. The rate of this progression varies between patients. The disease progresses more quickly in individuals with a very low level of glomerular filtration, in young men, as well as in those who excrete a lot of protein in their urine.
A timely diagnosis and adequate treatment can significantly prolong the life of patients with chronic renal failure.
Who is at risk?
- Suffering from diabetes.
- Suffering from arterial hypertension - high blood pressure.
- Elderly.
- Suffering from any chronic kidney disease.
- Persons with high cholesterol levels.
- Obese people.
- Smokers.
- Having relatives suffering from chronic renal failure.
Diagnostics
The diagnosis is made on the basis of elevated levels of nitrogenous wastes - creatinine and urea. An ultrasound examination of the kidneys is also required. To clarify the condition of the body and the degree of damage to organs and systems of the body, a wide range of laboratory tests are performed.
Laboratory research
- Urea and creatinine in blood serum. These are nitrogenous wastes (protein breakdown products) that can only be excreted by the body through urine. A progressive increase in creatinine is the main diagnostic sign of chronic renal failure. The level of urea, unlike creatinine, does not always correspond to the severity of renal dysfunction. Recently, to more accurately assess the degree of renal dysfunction, a special indicator has been used - glomerular filtration rate. It is determined using different formulas taking into account the patient’s height, weight and gender.
- General blood analysis.
- Hemoglobin and red blood cells. The level of hemoglobin and red blood cells in chronic renal failure is usually reduced, characterizing the development of anemia.
- Hematocrit Hematocrit is an indicator characterizing blood viscosity and is the ratio of the volume of blood cells to the total volume of blood. In chronic renal failure, the hematocrit is usually significantly reduced.
- Platelets. The number of platelets (blood platelets) is often reduced in chronic renal failure, reflecting an increased tendency to bleed.
- Density of urine. Renal failure is characterized by a significant decrease in urine density.
- Red blood cells. An increase in the level of red blood cells in the urine may indicate glomerulonephritis as a cause of chronic renal failure.
- Leukocytes. A significant number of white blood cells in the urine is a sign of a urinary tract infection.
- Protein. The more protein is excreted in the urine during chronic renal failure, the faster the disease progresses.
- Cylinders. Casts of fragments formed in the lumen of the renal tubules. A characteristic sign of chronic renal failure are waxy casts.
- Triglycerides. In patients with chronic renal failure, the level of triglycerides, a type of fat found in the blood, is especially common.
- Cholesterol. Total cholesterol may be normal, but the content of “good” cholesterol—high-density lipoprotein cholesterol (HDL)—is often reduced and the content of “bad” cholesterol—low-density lipoprotein cholesterol (LDL) is increased.
- Serum calcium and phosphorus. Chronic renal failure is characterized by decreased serum calcium, while phosphorus levels are usually elevated.
- Alkaline phosphatase. Alkaline phosphatase is an enzyme that is found in large quantities in the bile ducts and bone tissue. With chronic renal failure, bone tissue is destroyed, so the amount of alkaline phosphatase in the blood increases due to its bone fraction
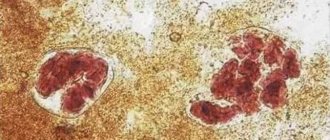
- Kidney biopsy. In diagnostically difficult cases, a kidney biopsy may be required - the removal of a small piece of kidney tissue, which is examined under a microscope, which makes it possible to identify the characteristic signs of chronic renal failure - replacement of the kidney glomeruli with scar tissue.
Other research methods
- Ultrasound examination (ultrasound) of the kidneys. With chronic renal failure, there is a decrease in the kidneys (wrinkling) along with thinning of their outer layer. Ultrasound can also be used to detect kidney tumors, stones or cysts.
- Computed tomography (CT) and magnetic resonance imaging (MRI) of the abdominal cavity. The studies are more sensitive than ultrasound. They allow you to detect tumors, cysts and stones up to 5 mm in size.
Treatment
Chronic renal failure cannot be cured, but its progression can be slowed or even stopped. Treatment is given to relieve symptoms and prevent complications.
Strict blood pressure control is indicated for all patients with chronic renal failure; patients with diabetes need to maintain blood glucose levels within normal limits. Typically, lowering cholesterol levels with statin drugs is required.
It is recommended to limit the intake of salt and proteins, foods rich in potassium.
To treat anemia, erythropoietin is prescribed, an artificial analogue of the hormone that stimulates the formation of red blood cells, sometimes together with iron supplements. Red blood cell transfusions are rarely required.
It is usually necessary to prescribe vitamin D to improve bone metabolism, as well as calcium salts, which bind excess phosphates in the blood.
Typically, most patients also receive diuretics.
The dose of drugs excreted through the kidneys in the urine requires adjustment in chronic renal failure.
If there is a significant decrease in kidney function, hemodialysis is performed - mechanical filtration of the patient’s blood using an “artificial kidney” apparatus.
Prevention
- Losing excess weight.
- Normalization of cholesterol levels in the blood.
- To give up smoking.
- Observation by a doctor and strict adherence to prescriptions if you have diabetes, high blood pressure or kidney disease.
Recommended tests
- General blood analysis
- General urine analysis with microscopy
- Serum creatinine
- Urea in serum
- Biochemical parameters - lipid profile
- Serum iron
- Iron binding capacity of serum
- Ferritin
- Total alkaline phosphatase
- Rehberg test (endogenous creatinine clearance)
- Potassium, sodium, chlorine in serum
- Serum calcium
- Serum phosphorus
- Erythropoietin
- Parathyroid hormone, intact
- Vitamin D, 25-hydroxy (calciferol)
Literature
- Corey Foster, Neville F. Mistry, Parvin F. Peddi, Shivak Sharma, The Washington Manual of Medical Therapeuticts (33rd ed.). Lippincott Williams & Wilkins Philadelphia, 2010.
- Dan L. Longo, Dennis L. Kasper, J. Larry Jameson, Anthony S. Fauci, Harrison's principles of internal medicine (18th ed.). New York: McGraw-Hill Medical Publishing Division, 2011.
- K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, classification and stratification. Am J Kidney Dis 39 (suppl 1), 2000.
- Meyer TW et al: Uremia. N Engl J Med 357:1316, 2007.
Kidney failure in children - how to notice and treat
In a healthy body, the kidneys filter the blood from excess fluid, salts and other substances, which are then excreted in the urine.
Kidney failure is a condition where the kidneys do not function well, causing substances that should be excreted from the body to flow back into the bloodstream. The disease is rare in children. It mainly affects adults who already have other kidney problems.
Kidney failure develops throughout life and goes through several stages. At the last stage, the kidneys may stop working completely. But if you identify the disease in time and start treatment, you can control its development and avoid complications.
What are the symptoms of the disease?
In the early stages, the disease may have no symptoms at all. As the condition worsens, you may notice that:
- urination has changed - the child goes to the toilet too much or, conversely, too little;
- swelling appeared on the body;
- blood pressure increased;
- the child has no appetite, feels sick or is vomiting;
- the child feels tired;
- bone fractures occur more often;
- the child may appear pale due to anemia. Anemia occurs because in a healthy body, the kidneys help produce red blood cells (red blood cells). And due to illness, this process is disrupted.
Is there any test I can take to detect the disease?
If your doctor discovers problems with your kidneys before your baby is born, or you notice symptoms of kidney failure in childhood, you will need to undergo testing:
- First, your doctor will order a blood test to measure your kidney function. This is an indicator called the “Reberg-Tareev Test” - with its help you can find out how much blood the kidneys filter per minute. In a healthy body, this figure should not be lower than 90 ml/min;
- urine test to see if there is blood in the urine or if the protein content is high.
Other tests, such as ultrasound, MRI, and CT scans, may be needed to evaluate what the kidneys look like and whether there is any obvious damage. Sometimes a biopsy is needed, a procedure in which part of the kidney tissue is removed for testing in a laboratory.
How to treat kidney failure?
Treatment depends on the stage of the disease and the severity of symptoms. Mild forms of the disease are monitored by a pediatrician. In more severe cases, you will need the help of other specialists - a pediatric nephrologist and a nutritionist.
In the early stages (stages 1 to 3), treatment is usually aimed at controlling blood pressure and following a diet. The doctor may prescribe medications and recommend:
- eat less salt, sugar and fatty foods. Include vegetables and fruits in your diet;
- exercise;
- no smoking;
- stop taking ibuprofen.
After stage 3, you will have to control the amount of fluid consumed and the quality of food. The doctor may also increase the dose of medication or prescribe additional medications to control symptoms. For example:
- ACE inhibitors are usually prescribed to control blood pressure;
- Statins are prescribed to control cholesterol levels;
- for edema, diuretics are prescribed - tablets that help remove excess fluid from the body;
- If anemia has developed due to kidney problems, you will need to inject the hormone erythropoietin under the skin or into a vein - it helps the body produce more red blood cells. For iron deficiency anemia, iron supplements are prescribed;
- For bone diseases, medications containing calcium and vitamin D are prescribed.
In rare cases, the disease reaches the final stage, when the kidneys stop working completely. Then a donor kidney transplant or dialysis is required - a machine that filters blood outside the body.