Full text of the article:
After reading the article, you will learn:
- What are the indications for performing a colonoscopy without anesthesia?
- How unpleasant is the procedure without anesthesia?
- How to reduce the intensity of discomfort during the procedure.
Nervous stool
I'm not an exception. No matter how much the gastroenterologists tried to convince me to decide on a colonoscopy, they didn’t succeed. I started having problems with my intestines about 7 years ago. As soon as I got nervous or disrupted my usual diet, I got “bear sickness.” There were times when, due to diarrhea that started at the wrong time, I could not leave the house without taking a fixative drug.
Article on the topic To break. Why does intestinal injury occur and what can be done about it?
Doctors just shrugged: similar symptoms accompany many diseases of the gastrointestinal tract, including serious ones (ulcerative colitis, Crohn's disease, benign or malignant tumors). In order to find out the truth, I was advised to undergo examinations, among which one of the first places is a colonoscopy.
Preparations for colon cleansing before colonoscopy
The drugs used to prepare for colonoscopy contain macrogol (polyethylene glycol) and have different names and different manufacturers. The most common are:
- Moviprep (UK),
- Fortrans (France),
- D-Forzhekt (Belarus),
- Forddrive (Belarus).
The release form is powder. Depending on the drug, it is necessary to prepare from 2 to 4 liters of solution for preparation.
Preparation with Moviprep
If you are preparing with Moviprep , then you need to drink 2 liters of solution and 1.5-2 liters of drinking water (or clear, approved liquid). Only 4 liters of liquid. Each sachet dissolves in one liter of boiled or drinking water at room temperature.
If the colonoscopy is in 1 shift, then, starting from 18-19 pm and until 20-21 pm, you drink two liters of liquid - 1 liter of Moviprep solution and 1 liter of water - at a rate of one liter per one or one and a half hours. A glass in fifteen, twenty minutes. That is, not the entire volume at once, but gradually. You can alternate glasses - a glass of solution - a glass of water - a glass of solution - etc. The drug will begin to work, in most cases, within an hour or an hour and a half. You will want to go to the toilet. It is necessary that there is a toilet nearby, that is, it is better to cancel guests, visits or a visit to the theater that evening.
And usually by midnight that liter or two will be out. You will see how at first the water comes out cloudy, and then clearer and clearer, almost transparent by night. Sometimes there may be a delay in the effect of the drug for 2-3 hours. In this case, you should pause the preparation and wait until the amount you have already drunk begins to take effect. As a rule, you rest at night.
Early in the morning on the day of the study, you drink the remaining one liter of Moviprep and a liter of water, calculating the intake of the last glass of liquid 3-4 hours before the time of the study (for example, from 4 to 6 am, if the study is at 9.00), so that this liquid has time to leave at home, before you leave the house. The morning portion comes in easier and comes out faster.
If the colonoscopy is in the 2nd shift (after 15.00), then you drink the entire volume of liquid - 2 liters of Moviprep solution and 2 liters of water - in the morning on the day of the examination, starting from 7-8 am until 12.00 and later (depending on the time of the examination), in the same way, alternating the solution and water and taking breaks between glasses for 15-20 minutes. In any case, the last sip of the prepared solution should be taken at least 3-4 hours before the scheduled time of colonoscopy, regardless of whether it is performed under general anesthesia or not.
Preparation with Fortrans, D-Forzhekt or Fordrive
If you are preparing with Fortrans , D-Forject or Fordrive , then you need to drink 4 liters of solution. The principle is the same. Each sachet dissolves in one liter of boiled or drinking water at room temperature.
If the colonoscopy is in 1 shift, then, starting from 18-19 pm and until 20-22 pm, you drink two to three liters of solution - at a rate of one liter per hour or one and a half hours. A glass in fifteen to twenty minutes. That is, not the entire volume at once, but gradually. The drug will begin to work, in most cases, within an hour or an hour and a half.
Early in the morning on the day of the study, you drink the remaining one or 2 liters of the drug, calculating the intake of the last glass of liquid 3-4 hours before the time of the study (for example, from 4 to 6 am, if the study is at 9.00), so that this liquid has time to leave at home, before you go outside. The morning portion comes in easier and comes out faster.
If the colonoscopy is in the 2nd shift (after 15.00), then the entire volume of liquid - 4 liters of the drug solution (Fortrans, D-Forzhekt or Fortrans) - you drink in the morning on the day of the study, starting from 7-8 in the morning until 12.00 and later, in the same way taking breaks between glasses for 15-20 minutes. In any case, the last sip of the prepared solution should be taken at least 3-4 hours before the scheduled time of colonoscopy, regardless of whether it is performed under general anesthesia or not.
No, no, not this!
After interviewing friends and acquaintances who had undergone this diagnostic procedure, I firmly decided for myself: I would only go for it on pain of death. The prospect of writhing in pain for 15-30 minutes while a long tube was pushed into your anus was not at all exciting to me. Articles on the Internet added fuel to the fire of my fears, telling about the complications of this invasive (with penetration into organs and tissues. - Ed. ) procedure, up to infection and intestinal perforation.
Safety
Colonoscopy today is a routine procedure, so complications after it are quite rare. One of the most dangerous – intestinal perforation – is observed in less than 1% of cases.
There is no need to worry about possible infection during a colonoscopy. In self-respecting clinics, endoscopic equipment is disinfected in compliance with all modern standards. The leading position is occupied by the processing of endoscopes using automatic washing and disinfecting machines.
Article on the topic
Colonoscopy and intestinal biopsy: how to prepare for the study
The main thing is preparation
I decided not to use pain relief, and decided to undergo the frightening diagnostic procedure only when it became completely unbearable. I chose the doctor by word of mouth. But it was still necessary to prepare for the upcoming execution...
How dangerous are polyps in the intestines? More details
There are no analogues
No existing method can completely replace colonoscopy. X-ray methods (irrigoscopy, CT, MRI, virtual colonoscopy) can only complement the overall picture of some pathological processes. Colonic capsule, as an alternative to traditional colonoscopy, has a number of disadvantages. It provides for mandatory gastroscopy before the study. In addition, some patients cannot swallow the capsule on their own - it is quite large. And with reduced motor function, it is not always possible to examine all parts of the colon. The capsule does not allow us to examine pathological formations in detail. With this method, it is not possible to take a biopsy.
Of course, science does not stand still, and it has not just stepped forward, but has made a real breakthrough: equipment has appeared with high resolution, which allows you to magnify the areas under consideration. With such high-tech technology, the doctor will examine the microrelief and vascular pattern of the formation. Which is very important for the early diagnosis of cancer and precancerous diseases.
In addition, the colonoscopy technique itself is being improved. Nowadays, the Japanese technique is considered generally accepted, in which the colon is collected using a device with minimal distention of the intestine with air. The use of carbon dioxide instead of air, which is absorbed more quickly without causing bloating of the intestine, also reduces pain during the examination.
False alarm
I entered the endoscopy room on my legs stiff from fear. But my fears were not justified. The doctor I chose turned out to be a true professional: during the examination I never felt pain. Except that sometimes there were unpleasant, but quite tolerable sensations.
Article on the topic
A new risk factor for heart attacks has been found. And a cure has been found
I flew out of the office like a bird. All my fears were behind me. And most importantly, they didn’t find anything serious about me! It was necessary to decide on this procedure at least for this reason.
The source of my suffering turned out to be irritable bowel syndrome, a functional disorder that occurs in some people in response to stress and is quite successfully treated.
Indications for colonoscopy without anesthesia
If the patient wishes, the procedure can be performed with additional anesthesia, even if there is no indication for this. But there are certain categories of subjects for whom anesthesia is strictly contraindicated, these include:
- Patients with acute infectious diseases.
- Patients with peritonitis or suspected inflammation of the peritoneum.
- Patients with serious pulmonary and heart failure.
- Pregnant women, people allergic to anesthetics.
- Patients with severe mental and neurological disorders.
For these diseases, it is not necessary to completely abandon pain relief. How to do a colonoscopy - without anesthesia or with anesthesia is decided by the patient and the endoscopist on an individual basis. Only a specialist can take into account all the advantages and risks of research without anesthesia and help you choose the right option.
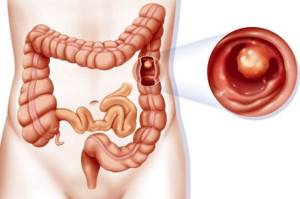
What is a colonoscopy?
Photo: © depositphotos.com/ @ kot36
A special status in coloproctology now belongs to endoscopic examination of the colon - colonoscopy, the popularity of which continues to grow throughout the world. This procedure provides high diagnostic accuracy with a low invasiveness of the method. Considering the total length of the colon (1-1.5 m), during colonoscopy it is possible to assess the condition of the intestinal mucosa, identify various benign neoplasms and remove them. In addition, this type of examination provides accurate and early diagnosis of precancerous diseases of the colon and colorectal cancer in the early stages.
During a colonoscopy, an endoscopist examines and evaluates the condition of the colon mucosa using a special probe - an endoscope. Using special forceps, he can remove tissue for subsequent examination under a microscope. This is one of the important advantages of colonoscopy compared, for example, with irrigoscopy or MRI.
Colonoscopy in a dream
Pain during the examination can be reduced by using a special technique for performing colonoscopy—small distention of the intestine with air, and only the use of anesthesia can completely remove pain and discomfort. The anesthesia used for colonoscopy is not quite the same as that used for major abdominal operations, since deep, long sleep is not required, and tracheal intubation is not required for patients to breathe during the examination. A sedative is administered intravenously, and the patient falls asleep and does not experience any discomfort.
Unfortunately, not all medical institutions in Nizhny Novgorod have the opportunity to undergo an endoscopic examination under anesthesia, but now in some private clinics, for example, in the medical one, such a service exists. It should be added that in the same way you can examine not only the colon, but also the upper parts of the gastric tract; this study is called esophagogastroduodenoscopy.
Many patients refuse to undergo endoscopic examinations for fear of unpleasant or painful sensations, thereby dooming themselves to late diagnosis of life-threatening diseases, while there is a simple and painless way to perform endoscopic examinations in their sleep.
Before the procedure, an examination by an anesthesiologist is necessary: he determines the indications and contraindications for the use of a sedative drug, possible risks of its use, selects the dose of the drug and the length of time the patient remains asleep. This procedure uses a modern drug that has minimal side effects.
How long does the procedure take?
The time spent on the procedure is purely individual. It all depends on the length of the colon, on what and how many bends it makes, on concomitant pathology (presence of ascites, tumors of the pelvic and abdominal organs, adhesions).
As a rule, the procedure takes 30-50 minutes, of which 5-10 minutes are spent passing the large intestine to its “end” (this is the place of transition of the large intestine to the small intestine - the so-called Bauginev valve and the dome of the cecum), the rest of the time the doctor examines the colon mucosa on the way back and collects material for histological examination.







