When to get tested
Lupus erythematosus is one of the common autoimmune diseases of an inflammatory nature. It mainly affects women - they account for up to 90% of all identified cases. The disease is detected after the onset of childbearing age.
The disease is divided into several types - systemic, discoid and tuberculous. The reasons for the development are different - damage to the body by infectious and viral diseases, taking certain types of medications, prolonged and frequent exposure to the sun without the use of protective equipment.
Among the signs in the presence of which doctors prescribe such a study:
- Increased fatigue.
- Pain in the joints, swelling, feeling of stiffness.
- Periodic occurrence of fever.
- High skin sensitivity to ultraviolet radiation.
- Feeling of dryness in the eyes.
- Pain of different localization in the chest area.
- Decreased body temperature, appearance of a bluish tint to the skin of the extremities.
Another common principle is the appearance of rashes on the face. The rash is shaped like a butterfly and covers the cheeks and bridge of the nose. Some people may also complain of vomiting and nausea.
LE cells
LE cells (Lupus erythematosus)
- these are leukocytes destroyed by a special type of human immunoglobulin (LE factor), which appears in the blood during autoimmune diseases. Interacting with healthy leukocytes (neutrophils and monophages), the LE factor destroys their nuclei and absorbs the nuclear material contained in them. In 80% of cases, LE cells are detected in the blood of patients with SLE (systemic lupus erythematosus) and autoimmune diseases such as rheumatoid arthritis, dermatomyositis, systemic scleroderma.
The formation of LE cells is a consequence of a violation of the immune system, evidence of its autoaggression and is caused by the presence of the LE factor in the blood.
LE factor
LE factor is a complex of specific circulating immune complexes (CIC) with antinuclear activity, which destroy not only the nuclear material of protective cells, but also settle on articular surfaces, vascular walls, are retained in the kidneys (lupus nephritis) and have a damaging effect on these fabrics.
In patients with SLE, LE cells are found in the blood, synovial and cerebrospinal fluids, and pleural effusion.
LE cells appear in the blood early in the disease or during an exacerbation. As the patient's condition improves, the number of LE cells may decrease or disappear completely.
Indications
Analysis for the presence of LE cells is carried out both for diagnosis and for monitoring the effectiveness of treatment of systemic lupus erythematosus. Cells are detected at an early stage of the disease and during exacerbation. They can be found not only in the blood, but also in the urine and red bone marrow. After therapy is prescribed, the number of these cells decreases until they disappear completely. Analysis for LE cells is an indicator of the severity and activity of the process, as well as the success of SLE treatment.
In other systemic diseases, the percentage of detection of LE cells is very small, so this analysis has a secondary auxiliary value.
Preparation
No special preparation is required. It is recommended that blood be taken no earlier than 4 hours after the last meal.
Interpretation of results
Reference values: not found.
Positive result:
- systemic lupus erythematosus;
- rheumatoid arthritis;
- scleroderma;
- drug-induced lupus-like syndrome;
- periarteritis nodosa;
- thrombocytopenic purpura;
- hemolytic anemia;
- acute leukemia;
- pernicious anemia;
- miliary tuberculosis;
- erythroderma;
- active hepatitis;
- plasmacytoma.
Systemic LE cell erythematosis or Systemic lupus erythematosus
Systemic lupus erythematosus is an autoimmune disease characterized by damage to the skin, musculoskeletal system, heart, kidneys and other internal organs.
Normally, cells of the immune system detect and destroy various foreign objects in the body (for example, infectious agents). In autoimmune processes, the immune system aggressively attacks the body's own cells and tissues, causing their inflammation and destruction.
The exact causes of the development of this disease are unknown, although researchers have identified some risk factors: genetic predisposition, exposure to certain infections (for example, Epstein-Barr virus), environmental factors (for example, exposure to sunlight, smoking).
Symptoms of systemic lupus erythematosus are varied. The disease may have an acute onset or progress slowly with mild clinical manifestations. The most common and characteristic symptom is damage to the skin and mucous membranes. In this case, red spots form on the face in the area of the nose and cheeks, shaped like a butterfly.
Along with the skin, joints, kidneys, lungs, heart, and nervous system can be involved in the pathological process with the development of corresponding symptoms.
Synonyms Russian
Libman-Sachs disease.
SynonymsEnglish
Systemic Lupus Erythematosus, Libman-Sacks Disease.
Symptoms
- Increased body temperature;
- general weakness, fatigue;
- pain, swelling, limited mobility in joints;
- erythema (intense redness of the skin) in the nose and cheeks;
- erythematous rashes that may be slightly raised above the surface of the skin (lesions on the skin may appear or enlarge when exposed to sunlight);
- ulceration of the mucous membrane of the nasal cavity, mouth;
- hair loss;
- chest pain;
- dyspnea;
- paleness, coldness, feeling of numbness in the fingers and toes in the cold;
- headache;
- disturbance of consciousness;
- memory loss;
- convulsions.
General information about the disease
Systemic lupus erythematosus is an autoimmune disease characterized by damage to various internal organs. It is based on autoimmune mechanisms. Cells of the immune system begin to destroy body structures, mistaking them for foreign objects. Complexes of immune cells (antibodies) and antigens (body cells) are formed in the blood, which spread throughout the body, causing inflammation in the affected organs. The vessels of the microvasculature (microscopic blood vessels: arterioles, venules, capillaries) are exposed to the aggressive effects of the immune system.
The exact causes of the disease are unknown. There are a number of factors that contribute to the development of systemic lupus erythematosus.
- Genetic predisposition. According to researchers, in the case of maternal disease, the risk of developing systemic lupus erythematosus in a girl child is 1:40, and in a boy child – 1:250.
- Infectious agents (for example, Epstein-Barr virus) can provoke autoimmune reactions that occur in systemic lupus erythematosus.
- Medicines (for example, some anticonvulsants, antihypertensives) can cause manifestations of systemic lupus erythematosus. As a rule, symptoms disappear after discontinuation of drugs.
- Exposure to sunlight in individuals predisposed to SLE may trigger the development of the disease.
- Hormonal changes in women. Scientists have found that the administration of estrogens during the postmenopausal period may increase the risk of SLE.
The most common syndrome with systemic lupus erythematosus is damage to the skin and mucous membranes. On the face in the area of the nose and cheeks, erythema (intense redness formed as a result of the inflammatory process in the blood vessels) forms in the shape of a butterfly. In other areas of the body, erythematous spots may appear that are slightly raised above the surface of the skin. Ulcerations are found on the mucous membranes. Damage to small blood vessels causes trophic (caused by impaired tissue nutrition) changes in the skin. The consequence of this is brittle nails and hair loss.
From the musculoskeletal system, joint pain and manifestations of arthritis occur. Deformities in the affected joints rarely occur.
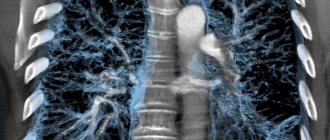
Involvement of the lungs in the pathological process can lead to pleurisy (inflammation of the membrane lining the chest cavity from the inside and the lungs from the outside), inflammation of the pulmonary vessels, the formation of blood clots in the pulmonary vessels, and pulmonary hemorrhages.
Sometimes myocarditis (inflammation of the heart muscle), endocarditis (inflammation of the inner lining of the heart involving the valve apparatus) develops. Vasculitis of the coronary arteries is also a serious complication.
Kidney damage can occur at any stage of the disease. The activity of the pathological process varies from asymptomatic to severe, rapidly progressive forms of glomerulonephritis (inflammation of the renal glomeruli), which lead to renal failure.
Foci of lesions form in the nervous system as a result of the involvement of its various parts in the pathological process. This is accompanied by headaches, seizures, deterioration of memory, thinking and other neurological disorders. The consequence of lupus vasculitis of the cerebral vessels can be severe complications in the form of strokes.
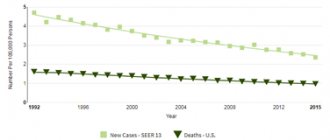
Systemic lupus erythematosus occurs with periods of exacerbations and remissions (time periods without signs of the disease). Considering the lack of treatment methods that can achieve a complete cure, the main goal is to reduce the severity of individual symptoms, slow down the progression of the disease, and achieve stable remission.
Who is at risk?
- Systemic lupus erythematosus is more common in women.
- Persons aged 15-45 years.
- African Americans, Latinos, Asians.
- Persons whose close relatives suffer from systemic lupus erythematosus.
Diagnostics
Diagnosis of systemic lupus erythematosus consists of identifying the characteristic symptoms of the disease, markers of autoimmune reactions specific to it, and conducting a series of studies.
Laboratory research
- Antinuclear antibodies, IgG (anti-Sm, RNP, SS-A, SS-B, Scl-70, PM-Scl, PCNA, CENT-B, Jo-1, histones, nucleosomes, Ribo P, AMA-M2), immunoblot . The study allows you to detect specific antibodies to various components of cell nuclei (antigens) of the body. For systemic lupus erythematosus, the presence of antinuclear antibodies anti-Sm, SS-A, PCNA, and antibodies to histones (a type of protein) is specific.
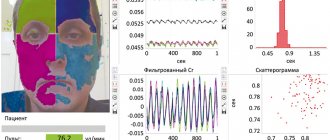
- Antinuclear factor on HEp-2 cells. This is one of the main methods for detecting antinuclear antibodies - cells of the immune system that aggressively affect the components of the cell nuclei of their own body. Their formation is characteristic of various autoimmune diseases.
- Anti-double-stranded DNA antibodies (anti-dsDNA), screening. They are found in autoimmune diseases such as systemic lupus erythematosus, scleroderma, and Sjogren's syndrome. In SLE, their level correlates with the severity of the disease and the likelihood of complications.
- Antibodies to cardiolipin, IgG and IgM. These antibodies are formed against cell phospholipids (one of the components of cell membranes). Although their presence is more specific for antiphospholipid syndrome, they can be observed in lower concentrations in SLE.
- General blood analysis. Allows you to quantify the main blood parameters. In SLE, the level of red blood cells, platelets, and leukocytes is reduced.
- Erythrocyte sedimentation rate (ESR). Nonspecific indicator of various pathological processes. In SLE, ESR is elevated due to an autoimmune inflammatory process.
- Microscopy of a blood smear. Examination under a microscope of a preparation made from a drop of blood. In SLE, altered neutrophils (a type of white blood cell) are found in it.
- General urine analysis with sediment microscopy. The basic physicochemical properties of urine and the presence of physiological and pathological impurities in it are assessed. When the kidneys are damaged, protein and red blood cells are found in the urine due to the development of lupus glomerulonephritis.
- C-reactive protein, quantitative (method with normal sensitivity). Sensitive marker of active inflammation and tissue damage. In SLE, its level is elevated.
Damage to various organs in SLE requires a comprehensive laboratory examination to assess various vital signs (for example, determination of parameters of kidney and liver function).
Other studies
- Computed tomography (CT). Allows you to obtain highly accurate layer-by-layer images of internal organs, which has great diagnostic value in identifying the extent of damage to internal organs in SLE (for example, when diagnosing lesions in the brain).
- Radiography. Can be used in SLE to detect pathological changes in the lungs and joints.
- Echocardiography. A method for studying the heart muscle based on the properties of ultrasound. This study allows you to visualize the functioning of the valvular apparatus of the heart, identify signs of myocarditis, pericarditis, which is necessary for diagnosing cardiac complications of SLE.