Leptothrix is a gram-negative anaerobic rod.
Refers to bacteria.
Has some affinity with mushrooms.
This is a representative of transit microflora.
Leptothrix often penetrates the genitourinary tract or oral cavity.
Can live there for a long time.
In this case, no pathological symptoms arise.
But symptoms are possible due to decreased immunity.
In this case, the disease is treated with antibacterial drugs.
Leptothrix in a smear - what is it?
Leptothrix can be detected in urogenital or oropharyngeal smears.
This bacterium can be seen under a microscope.
It consists of thin threads with segmented ends.
During microscopy, the laboratory technician notices long chains in the form of dots and dashes.
Leptothrix does not always cause inflammation.
But in some cases they are possible.
The bacterium exhibits pathogenicity most often in the presence of other microorganisms.
It intensifies inflammatory processes against the background of sexually transmitted infections.
It is also one of the causative agents of bacterial vaginosis.
When it enters the oral cavity, leptothrix provokes inflammation of the gums, tonsils, and tongue.
May lead to darkening and destruction of tooth enamel.
Causes of leptothrix
Leptothrix is very easy to become infected with.
The bacterium can spread from person to person through sexual contact.
But in men, leptothrix does not live in the genitourinary system.
Accordingly, partners of different sexes can become infected from each other only through oral sex.
However, after infection, the pathological process does not develop in most people.
Leptothrix exists peacefully on the mucous membrane of the genitourinary system.
It does not cause any problems for a long time.
Provoking factors are needed for bacteria to reach a large population and become pathogenic.

Such factors could be:
- decreased immunity;
- long-term uncontrolled antibiotic therapy (if those groups of drugs are used to which leptothrix is not sensitive);
- HIV;
- diabetes;
- bacterial vaginosis (leptothrix against the background of this disease is often found in association with other microorganisms);
- infection with sexually transmitted infections.
Leptothrix is not only transmitted from person to person.
It can also exist in the external environment for a long time.
Leptothrix can be contracted in a swimming pool or through poorly disinfected tap water.
How can you prevent infection?
To prevent Leptotrix infection, you should follow these recommendations:
- Observe applicable hygiene standards, especially after visiting public places (sauna, baths, swimming pool, beach).
- At least twice a day for genital hygiene.
- Avoid getting water into the paragraph.
- Pregnancy must be planned. This means that you must first undergo a comprehensive study, which includes testing.
- Do not drink tap water without passing through a filter.
- Because the disease may be asymptomatic, it is recommended to give a routine gynecological examination at least twice a year.
- If you do not have a regular sexual partner, use protection and contraception.
Leptothrix in the mouth
Very often, leptothrix filaments are detected when taking a swab from the mouth.
This bacterium is normally present in the oral cavity during childhood.
It is detected in 40% of children under 1 year of age.
But adults should not have leptothrix in their mouths.
Because its presence provokes inflammatory processes and negatively affects the condition of the teeth.
Leptotrichosis usually develops against the background of immunodeficiency.
It is considered a disease close to opportunistic mycoses.
Often develops in HIV-infected people at the AIDS stage.
Also, leptothrix of the tongue can occur against the background of chronic diseases of the oral cavity and gastrointestinal tract.
In most cases, the patient himself does not feel anything when this disease occurs.
He has no complaints or complains of a slight burning sensation.
It is noted on the tongue and the inner surface of the cheeks.
Upon examination, the doctor finds areas of white or gray plaque.
They cover all structures of the oral cavity.
There are no obvious signs of inflammation.
Leptothrix clusters can be seen with the naked eye.
They look like small (pinhead-sized) white dots.

Plaque cannot be removed easily.
When scraped, the plaque is removed, but underneath it reveals inflamed, loose, sometimes bleeding mucosa.
What symptoms may be observed?
Lactobacilli begin to predominate in the vaginal microflora after puberty. But why Leptothrix infection occurs is not known exactly.
There is an opinion that bacteria often appear after self-diagnosis and improper treatment of candidiasis. Anti-thrush medications are readily available, and women often skip gynecological appointments.
Leptothrix is often combined with the following pathogens:
- 1Trichomonas.
- 2Gardnerellas.
- 3 Candida.
- 4Chlamydia.
Manifestations of infection are nonspecific; in Western literature it is sometimes called the term “lactobacillosis.” It is not sexually transmitted and does not cause any symptoms in men.
The most common symptoms women experience are:
- 1 Copious, white or clear vaginal discharge without an unpleasant odor or lumps, sometimes resembling water.
- 2Itching and burning in the vagina and vulva area.
- 3The acidity of the vaginal environment remains normal.
- 4Sometimes a woman complains of discomfort and burning when urinating.
- 5During examination, the doctor, as a rule, does not see redness of the vaginal walls and swelling - obvious signs of inflammation.
Complaints often appear in the second phase of the cycle, when menstruation approaches. There is evidence that high concentrations of hydrogen peroxide and lactic acid in the vagina lead to damage to epithelial cells and nerve endings, which can cause the development of vulvodynia.
During pregnancy, the detection of leptothrix is also accompanied by copious liquid discharge, which constantly wets the underwear.
Leptotrichosis, that is, an infection caused by leptotrichia , is characterized by slightly different symptoms:
- 1Increase in the amount of vaginal discharge, change in color (gray, white-gray).
- 2The appearance of an unpleasant odor, typical of bakvaginosis.
- 3Shift of acidity to the alkaline side.
- 4Pain during sexual intercourse (dyspareunia).
- 5Itching and burning in the vagina.
One of the types of leptotrichia - Leptothrix amnionii - can cause the following complications:
- 1Premature termination of pregnancy.
- 2Choriamnionitis.
- 3Low fetal weight at birth.
- 4Postpartum sepsis in immunosuppressed women in labor.
- 5Infection of a newborn.
Identification of this pathogen is extremely rare.
Clinical course of leptotrichosis
Oral leptotrichosis is difficult to treat.
The disease can last for months and years.
Especially in patients who have reduced immunity.
Sometimes after a course of antibacterial drugs, bacteria die.
All symptoms disappear.
But after some time, when taking the smear again, leptothrix was again detected.
This may be due to:
- re-infection;
- preservation of the source of infection in hard-to-reach areas of the oral cavity;
- no use of systemic therapy (only local treatment).
Leptothrix may spread to the pharynx.
In this case, the person complains of pain when swallowing.
Upon examination, the doctor may detect reddened mucous membranes.
Leptothrix: what complications to expect
Leptothrix is a disease that may not show any signs of itself for a long time.
In this case, the pathogenic microorganism will cause harm to the body, which will be extremely difficult to resolve in the future.
Any inflammatory process in the genitourinary system, first of all, negatively affects reproductive functions.
Both women and men face infertility.
Infertility is difficult to treat, especially if its cause is opportunistic microorganisms.

In addition to infertility, the patient may face:
- impotence, which can be caused by both prostate and testicular damage
- decreased libido in the fair sex, which is explained by discomfort during sexual intercourse, lack of pleasure
- damage to the child’s body if the disease is diagnosed in a woman during pregnancy
- if the oral cavity is affected, tooth decay, inflammatory diseases of the gums and oropharynx are possible
Leptothrix in women and the stronger sex is not a harmless infection that can be ignored.
Adequate therapy for exacerbation of the disease is mandatory!
Leptothrix in gynecology
Leptothrix is often found in the urogenital system in women.
This bacterium lives in the vagina.
It may be part of an opportunistic flora.
But it is contained in small quantities.
In an ideal state of the vaginal biocenosis, the number of all anaerobic bacteria does not exceed 1% of their total number.
Among these anaerobes there is also a place for Leptothrix.
With such a small amount, these bacteria are not detected in a smear by microscopy and do not cause pathological processes.
Most often, leptotrichosis of the vagina is detected against the background of bacterial vaginosis.
The disease is manifested by discharge and the appearance of gray or white spots on the walls of the vagina.
The doctor discovers them during examination.
It is from these areas of the mucosa that smears are taken, in which leptothrix is detected.
An increase in the number of anaerobes can be caused by:
- taking antibiotics
- decreased immunity
- suffered serious illnesses
- lack of sufficient vaginal hygiene, or, on the contrary, excessive hygiene with frequent use of detergents containing antibacterial components
When lactobacilli die, anaerobic microorganisms take their place.
The vaginal pH shifts.
Lactic acid and hydrogen peroxide are not produced.
Therefore, the female genitourinary system becomes vulnerable to infections.
A woman easily becomes infected with sexually transmitted diseases through sexual intercourse.
Nonspecific inflammation is often associated.
Bacterial vaginosis associated with Leptothrix occurs without treatment for years.
Self-healing is unlikely.
Anaerobes occupy most of the biocenosis and do not allow lactobacilli to recover.
Therefore, only antibacterial treatment helps to normalize the composition of the vaginal microflora.
After it is carried out, probiotics are prescribed to populate the vaginal environment with “useful” microbes.
Tests for leptothrix
Leptothrix is not at all difficult to detect.
This bacterium is visible under microscopy.
In most cases, targeted testing for leptotrichosis is not carried out.
The pathogen is identified during a bacterioscopic examination.
A swab is taken from the mouth or vagina of women.

Gram-negative rod-shaped bacteria are found in the clinical material.
They form chains in the form of alternating dots and dashes.
In turn, the detection of leptothrix is the reason for a more in-depth examination of the patient.
Because the presence of this microorganism is an indicator of other diseases.
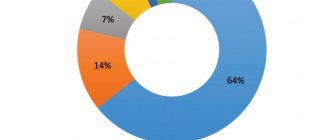
Against the background of leptotrichosis, the following are very often detected:
1. Sexual infections.
In approximately 60% of cases, along with leptothrix, a thorough examination of the patient reveals candida, ureaplasma, trichomonas, chlamydia or other pathogens.
Therefore, all women diagnosed with leptotrichosis are prescribed a smear from the urethra, vagina and cervix for sexually transmitted diseases.
PCR is mainly used for diagnosis.
2. Bacterial vaginosis.
It can be diagnosed by microscopy alone, which is supplemented by an amino test.
Bacterial vaginosis is said to occur when leptothrix and other anaerobic flora significantly outnumber lactobacilli.
Vaginal dysbiosis is considered a condition when the number of lactobacilli is less than 90%.
To clarify the state of the biocenosis, seeding or PCR may be prescribed.
3. Immunodeficiency states.
Leptothrix is considered an indicator of reduced immunity.
This is because in most patients, Leptothrix does not cause symptoms and does not multiply to the point of being detected by microscopy.
If this happens, it is likely that the immune system has failed.
It cannot inhibit the proliferation of the microorganism.
Therefore, patients diagnosed with leptothrix are often tested for HIV.

All patients are recommended to consult an immunologist.
The doctor may order an immunogram.
Based on this, the presence or absence of immunodeficiency is determined.
If necessary, immunocorrection is carried out in the future.
Occasionally, PCR or tank culture is used to detect leptothrix.
Leptothrix during pregnancy
Leptothrix rarely causes complications during pregnancy.
Nevertheless, such cases do occur.
There is now evidence that leptotrichosis increases the risk of:
- chorioamnionitis
- spontaneous abortion
- birth of underweight children
- bacteremia of newborns
The likelihood of postpartum endometritis increases.
Immunosuppressed women may develop sepsis after childbirth.
Some of these complications develop as a result of the direct pathogenic effect of Leptothrix.
Some are associated with decreased immunity.
In this case, leptothrix is not so much a cause as a marker.
After all, the presence of this bacterium indicates that not everything is in order with the woman’s immune system.
Leptothrix in men
A woman cannot infect a man with leptotrichosis through vaginal intercourse.
This bacterium is not adapted to live in the male urethra.
Therefore, men can have sex without fear with a woman who has vaginal leptotrichosis.
However, you should be aware of the possibility of infection from other bacteria.
After all, leptothrix often talks about bacterial vaginosis.
And with this disease, many other anaerobes are present in the vagina.
Some of them can cause anaerobic balanoposthitis in a man.
It occurs mainly in people with immunodeficiency.
The most common pathogen is gardnerella.
In addition, leptothrix is often detected in those who suffer from sexually transmitted diseases that occur in a latent form.
Therefore, a man can become infected with trichomoniasis, ureaplasmosis, chlamydia or other pathology.
For these reasons, it is better to avoid unprotected sexual contact with a woman until she is fully examined and treated.
In addition, a man's leptothrix can live in his mouth.
Therefore, it can become infected through oral sex.
At the same time, he himself also becomes a source of infection for his partners.
Features of the pathogen
Leptothrix are gram-negative, filamentous bacteria that do not form spores and prefer an anaerobic environment with very little oxygen (such bacteria are called microaerophilic).
Their name comes from Latin words meaning “fine hair”. In a smear, leptothrix looks like long thin or thick rods, which are arranged in chains resembling hairs. The external resemblance to actinomycete fungi initially led to a classification error: for a long time leptothrix was classified as a fungus.
They are usually grouped under the general name of the genus Leptothrix species (spp.).
Some researchers attribute Leptothrix to a special variety of lactobacilli, modified under the influence of environmental conditions.
They noticed that some women who go to gynecologists with complaints of heavy discharge have bacteria in their smears that form long chains.
In women who do not have symptoms of infection, lactobacilli are grouped in chains ranging from 5 to 15 microns in length. In women with complaints of heavy discharge, the length of one chain can reach 40-75 microns.
Until now, in the medical literature, the names of bacteria leptothrix and leptotrichia are considered synonymous. This is due to the confusion and difficulty of cultivating them.
Attention! In the new classifications, these are two different genera - Leptothrix and Leptotrichia! Be careful, bacteria cause completely different diseases!
Treatment of leptothrix
Leptothrix is a bacterium.
Like any other bacteria, this pathogen can be destroyed by antibiotics.

However, it should be taken into account that the pathogen is not sensitive to most antibacterial drugs.
It is not susceptible to aminoglycosides, macrolides (josamycin, azithromycin), fluoroquinolones (ciprofloxacin, levofloxacin).
The following groups of drugs are mainly used for treatment:
- nitroimidazoles (metronidazole, ornidazole)
- lincosamides (clindamycin)
Theoretically, tetracycline or chloramphenicol could be used.
Leptothrix is also sensitive to them.
But in practice, these antibiotics are used much less frequently.
They are unsafe and often cause side effects.
Local treatment is also used.
Women are prescribed vaginal tablets or suppositories for leptothrix.
They may contain metronidazole, miconazole, clindamycin.
Terzhinan is often prescribed for leptothrix.
It contains two antibiotics and an antifungal component.
Leptothrix is affected by all three substances:
- neomycin
- ternidazole (metronidazole analogue)
- nystatin
If leptothrix affects the oral cavity, rinsing the mouth with antiseptics is indicated.
For this purpose the following can be used:
- Lugol's solution diluted three times
- 0.12% solution of chlorhexidine bigluconate
- potassium permanganate solution 1:5000
- 1% boric acid
During systemic antibacterial therapy, antiseptics are used 2-3 times a day.
Growth should be rinsed after eating.
If a high probability of recurrence of leptotrichosis of the tongue is predicted, then maintenance treatment is carried out.
After a course of antibacterial therapy lasting from 7 to 10 days, oral antibiotics are stopped.
But antiseptics remain in the scheme.
They are used at least once a week.
Such supportive treatment is necessary primarily for patients who:
- HIV or diabetes diagnosed
- immunodeficiency states were detected
- severe somatic diseases were identified (elderly and debilitated patients)
- cases of relapse of leptotrichosis have been reported
Enzymes may be used during the use of systemic antibiotics.
They improve their penetration into tissues.
By increasing tissue concentration, they provide a more effective antibacterial effect.
In most cases, leptotrichosis responds well to treatment.
However, relapses occur quite often.
To prevent them, it is recommended to do the following:
- restore the patient's immunity
- cure concomitant infectious processes, including sexually transmitted diseases
- for vaginal leptotrichosis - normalize the composition of the vaginal biocenosis, populate it with lactobacilli (they protect the genital tract from opportunistic and pathogenic bacteria)
Therefore, the patient requires a full examination.
At the second stage of treatment, probiotics are prescribed.
In parallel with antibacterial therapy, immunomodulators are prescribed.
Management of patients with vulvovaginitis of mixed etiology during pregnancy
The “gold standard” for diagnosing diseases associated with disturbances of the vaginal biotope includes: microscopic examination of native and/or Gram-stained biological materials obtained from the upper third of the lateral vaginal vaults, pH-metry of vaginal discharge, as well as real-time polymerase chain reaction time [15].
The fundamental principle of managing patients with vulvovaginal infections of mixed etiology during pregnancy is to target all etiologically significant microorganisms, taking into account the balance of benefit and risk for the patient/fetus. In this regard, the clinician, when choosing a drug, must take into account the route of administration, dosage regimen, its composition, the nature of side effects, the presence of this drug in current clinical recommendations for treatment during pregnancy, taking into account laboratory confirmation of the pathogen, as well as the phasing of therapy and the expected patient adherence to treatment
Indications for treatment of VV are the presence of clinical manifestations with laboratory confirmation of the diagnosis, as well as asymptomatic carriage in women during pregnancy. VV is subject to treatment in pregnant women with symptoms, if the diagnosis is confirmed by the detection of Candida spp
.
When identifying Candida spp.
In women without clinical symptoms, treatment is not carried out.
Treatment of trichomoniasis is indicated for all patients with a positive result of any laboratory test for the presence of T. vaginalis
, regardless of the presence of symptoms [15].
Domestic regulatory documents give preference to the use of topical forms of drugs for the treatment of uncomplicated forms of mixed genital infection during pregnancy [1, 15]. The vaginal route of administration of topical drugs with the ability to create high concentrations of the active substance on the surface of the mucous membrane, ensure rapid delivery of the drug directly to the site of the disease and the entry of absorbed substances into the bloodstream, bypassing the liver, is most convenient and, in addition, does not lead to the formation of bacterial resistance C on the other hand, drugs used to achieve an exclusively local effect should have minimal effect on local immunity and the natural biocenosis of the vagina [19].
A pilot comparative study of the use of vaginal suppositories containing metronidazole (750 mg) and miconazole (200 mg) 2 times a day for 7 days and oral administration of metronidazole at a dose of 2 g once for the treatment of vaginal trichomoniasis with evaluation of the effect on the 12th–15th and Days 30–35 showed no significant difference in cure rates, with overall cure rates of 90% and 80%, respectively (p=1.00). High doses of intravaginal metronidazole in combination with miconazole provide good tolerability of treatment, which avoids the systemic side effects of nitroimidazoles in the treatment of trichomoniasis [20].
Currently, when managing patients with vulvovaginal infections, a two-stage treatment method is postulated, in which the goal of the first stage is the eradication of pathogens from the vagina, the second stage is the restoration of the optimal biochemical environment of the vagina with a sufficient number of lactobacilli [1, 15, 21]. Despite the generally accepted therapeutic guidelines, the literature also presents data proving the effectiveness of the simultaneous use of an antibiotic and a probiotic [22, 23]. A study examining regimens for the use of a probiotic with vaginal administration in patients with BV in combination with a course of antibacterial therapy with clindamycin (vaginal cream 2%) demonstrated comparable effectiveness of two regimens: 1) combined use from the first day of antibacterial therapy (clindamycin + probiotic for 7 days , then only a probiotic for 7 days) and 2) a sequential course of probiotics for 14 days, immediately after finishing taking the antibiotic (clindamycin for 7 days). The total assessment of clinical and laboratory effectiveness was 66.7% and 63.0%, respectively, with a reduction in the duration of the overall course of treatment by 1.5 times [22].
The drug of choice for the treatment of urogenital trichomoniasis and BV is a drug from the 5-nitroimidazole group. The mechanism of action is the integration of the nitro group of the molecule into the respiratory chain of protozoa and anaerobes, which disrupts the respiratory processes and causes cell death. The drug substance is active against protozoa: T. vaginalis
,
Entamoeba histolytica
;
anaerobic gram-negative ( Bacteroides spp.
,
Fusobacterium spp.
,
Veillonella spp.
,
Prevotella
) and gram-positive (
Clostridium spp.
,
Eubacterium spp.
,
Peptostreptococcus spp.
) microorganisms, as well as facultative anaerobe
G. vaginalis
. Aerobic microorganisms are insensitive to metronidazole, but in the presence of mixed flora (aerobes and anaerobes), metronidazole acts synergistically with antibiotics against common aerobes with a positive result. Treatment of BV in pregnant women with metronidazole is possible using the following regimens: orally (250 mg 3 times a day or 500 mg 2 times a day for 7 days) or vaginally (5 g once or for 5 days) in the II and III trimesters . Studies and meta-analysis have not established a relationship between the use of metronidazole during pregnancy and the occurrence of teratogenic complications in newborns [24], however, the use of the drug in the first trimester is contraindicated [15].
For the treatment of VVC, the drugs of choice are azole derivatives, in particular miconazole, the fungicidal and fungistatic effects of which are due to inhibition of the biosynthesis of ergosterol in the fungal membrane and plasma membranes, changes in the lipid composition and permeability of the cell wall, which causes the death of the fungal cell. The drug is effective in pathology caused by Coccidioides immitis
,
Cryptococcus neoformans
,
Petriellidium boydii
,
Paracoccidioides brasiliensis
,
C. albicans
,
Trichophyton
,
Epidermophyton
,
Malassezia furfur
, some gram-positive bacteria.
Since the most common causes of the infectious and inflammatory process in the lower genital tract are microbial associations, in treatment preference is given to combination drugs with proven effectiveness and a wide range of antimicrobial, fungicidal and antiprotozoal effects with the possibility of affecting aerobic, anaerobic microorganisms and representatives of the genus Candida
[12]. However, the use of certain drugs is limited during pregnancy, as indicated in the instructions for medical use. Thus, up to 12 weeks of pregnancy and during lactation during breastfeeding, the drugs of choice are antiseptics and natamycin. After 12 weeks pregnancy, intravaginal use of miconazole, itraconazole, ketoconazole, clotrimazole, sertaconazole, tioconazole, ciclopirox, econazole is possible [15, 25]. Among the recommended agents in the practice of an obstetrician-gynecologist, combination drugs (neomycin + nystatin + polymyxin B, metronidazole + miconazole, nystatin + nifuratel, butoconazole + clindamycin, neomycin sulfate + nystatin + prednisolone + ternidazole) and antiseptics (povidone-iodine, chlorhexidine, dequalinium chloride) [13, 26].
A study of the effectiveness of differentiated correction of vaginal microbiocenosis in women with nonspecific cervicovaginitis in the first trimester of pregnancy showed that the use of an antiseptic (dequalinium chloride) at the first stage of treatment for cervicovaginitis reduced the frequency of relapses of cervicovaginal infections by 26% compared to the control group, where restoration of vaginal microbiocenosis was carried out without taking into account the nature of the microflora after the first stage of treatment (p = 0.037) [27]. Interesting data were obtained by N. Yu Katkova et al. [17] on the duration of treatment depending on the recurrent or newly identified pathological condition. Thus, an analysis of a comparative assessment of the clinical and laboratory effectiveness of the use of a complex drug (tinidazole + tioconazole) for short (3 days: 1 suppository 2 times a day) and long ( 7-day: 1 suppository per day) treatment regimens for pregnant women diagnosed with “newly diagnosed BV” or a combination of BV with VVC and patients with a diagnosis of “recurrent BV” or a combination of BV with VVC showed that with new-onset dysbiosis and VVC in pregnant women In the second and third trimesters, both short and long treatment regimens are equally effective. For recurrent inflammatory and dysbiotic lesions of the vagina in patients in the second and third trimesters of pregnancy, a 7-day course of therapy is advantageous.
One of the currently well-studied combinations of drugs in the treatment of vulvovaginitis of mixed etiology in women both at the preconceptional stage and during pregnancy is the combination of metronidazole and miconazole, which has antibacterial, antiprotozoal and antifungal effects. A study to study local preconception preparation of patients with mixed vaginal dysbiosis using four treatment regimens (group I - metronidazole 500 mg + miconazole 100 mg, 1 suppository 2 times a day for 7 days intravaginally; group II - intravaginal applications of clotrimazole (2% cream ) 1 time per day for 6 days; Group III - intravaginal applications of clindamycin phosphate (2% cream) 1 time per day for 6 days; Group IV - complex drug ternidazole 200 mg + neomycin sulfate 100 mg + nystatin 100,000 units + prednisolone 3 mg, 1 vaginal tablet at night for 10 days) revealed high clinical and microbiological efficacy and high compliance on the Morisky-Green scale of the drug with the composition metronidazole + miconazole The use of clindamycin phosphate subsequently required concomitant antimycotic therapy. After completing the course of treatment for 6 months. the patients became pregnant and ended in the birth of a child [28].
Different authors use different dosing regimens for drugs containing a combination of metronidazole and miconazole. Earlier publications evaluating the efficacy and tolerability of a drug containing 750 mg metronidazole and 200 mg miconazole used daily intravaginally for 7 days for the treatment of vaginitis due to the most common pathogen associations revealed a clinical cure rate of 87.7% of cases with good tolerability [29]. A prospective study with a similar design to evaluate the effectiveness and safety of the use of a local drug (750 mg of metronidazole and 200 mg of miconazole) in the treatment of BV and VVC in pregnant women in the second trimester was conducted by O.V. Bitsadze et al [30]. The study included 122 pregnant women (mean age 29.6±2.5 years) at a gestational age of 18–22 weeks. with confirmed diagnoses of BV (n=51) and VVC (n=71). The authors showed the high therapeutic effectiveness of this combination of drugs on the 14th and 28th days from the start of the study in the group of pregnant women with BV - 96% (48/51) and 94% (47/51) and in the group with VVC - 94.2 % (65/71) and 91.3% (63/71) respectively
Domestic researchers have proven a positive effect when assessing subjective and laboratory parameters in patients with BV during treatment and 14 days after therapy with a combination drug (500 mg metronidazole + 100 mg miconazole). The results of the study indicate the high effectiveness of treatment (clinical data were normalized in 92% of cases, microscopic examination - in 94.2% of cases) against the background of good tolerability of the drug [31]. Similar data were obtained in foreign studies by E. Ozyurt et al. [32] proved the high effectiveness of 7-day treatment with a combination drug (metronidazole 500 mg + miconazole 100 mg) assessed 8–10 and 21–23 days after the start of therapy: relief of symptoms of vaginitis was noted in 91% of patients (67/74) and another 7% (5/74) improved. Microbiological cure rates were observed in 97.3% of cases of trichomonas vaginitis, in 86.6% of bacterial and 81% of candidal vaginitis with relapse rates of 2.7, 3.8 and 16.1%, respectively. The overall microbiological cure rate for mixed infections was 86% (of which 93% are trichomoniasis + BV and 73% are BV + VVC). The combination of metronidazole and miconazole is effective in the treatment of vaginitis, regardless of the isolated or combined etiology of the infection.
L.M. Nebyshinetz et al. [33] presented a study examining the use of lower doses of the combination metronidazole 100 mg + miconazole 100 mg (Gynocaps®) 1 capsule intravaginally for 10 days in the treatment of patients with a clinically verified diagnosis of VVC in comparison with a drug of similar composition and dosage regimen in form of vaginal tablets. The effectiveness of therapy was assessed based on the dynamics of clinical symptoms and data from a gynecological examination, microscopy and the degree of safety of the drug according to the UKU questionnaire (Udvald for Kliniske Undersogelser Scale). The authors noted positive dynamics on days 2–3 of treatment and the absence of clinical manifestations of VVC on day 5 in patients of both groups (p=0.23). Microbiological sanitation as a result of pharmacotherapy was achieved in women of both groups and did not have significant differences (p>0.05), which indicated the effectiveness of low doses of the combination of metronidazole 100 mg + miconazole 100 mg against the background of good (100%) tolerability and ease of use the drug in the form of vaginal capsules. Similar data [34] were obtained in a prospective study using the combination of metronidazole 100 mg + miconazole 100 mg (Gynocaps®) in the treatment of patients with mixed nonspecific infectious diseases of the vagina (in the regimen: vaginal capsules 1 time per day at night for 10 days, followed by contamination therapy with probiotic intravaginally for 14 days) with evaluation of effectiveness after 10 days and after 1 month. after the end of therapy The results obtained indicated a decrease in the severity of subjective symptoms of the inflammatory process and objective research data 10 days after the end of complex therapy in 95.6% of women, after 1 month - in 94.2%, with positive dynamics of the average pH value of vaginal secretion from 6.1±1.4 to 3.9±0.6 10 days after the end of therapy and maintaining the effect a month after the end of the course of treatment - 4.0±0.4 Experience of local therapy using the combination of metronidazole 100 mg + miconazole 100 mg in women with vulvovaginitis of mixed etiology showed high efficiency and safety of low concentrations of drugs and satisfactory compliance due to them.