Gastroscopy in its traditional sense is a visual examination of the upper gastrointestinal tract (esophagus, stomach, duodenum). The examination is performed using a flexible probe that has an optical camera at the end. The patient must swallow this tube. Using a gastroscope, you can also carry out a number of procedures: take a biopsy, inject a drug exactly into the affected area, remove polyps. However, despite all the advantages, gastroscopy is a rather unpleasant procedure. This frightens many patients and makes them refuse the necessary research.
Performing gastroscopy without swallowing the probe
To conduct this study, some preparation is necessary. Three days before the procedure, it is necessary to exclude spicy, fatty, poorly digestible foods, as well as foods that lead to increased gas formation, from the diet. It is preferable to eat boiled, light food, porridges, pureed dishes. The patient must be on a fasting diet for 12 hours before the test; he can drink.
Before the procedure begins, electrodes and a receiver device are attached to the patient’s body. The patient then swallows the video capsule. The capsule moves through the gastrointestinal tract at a natural speed and takes pictures 2 times per second. The transmitting device with which it is equipped sends images to a receiver attached to the patient’s body. This process lasts about 8 hours. There is no need for medical supervision at this time; you can lead a normal lifestyle, excluding sudden movements and heavy physical activity.
The capsule is disposable and comes out naturally. At the end of the shoot, you need to come back for an appointment. The doctor reads the information from the receiving device, processes the images, analyzes them and makes a diagnosis.
How is the examination carried out at the Gorbakov Clinic and what does it show?
An examination using a gastropanel involves taking blood from a vein from the patient on an empty stomach. After this, the patient drinks a gastrin-17 secretagogue, which is a drink with a very high soy protein content. If the patient has previously had a food allergy to soy, eggs, chocolate, or dairy products, he should inform the doctor about this. In this case, he will be offered food protein as a stimulant. Twenty minutes later, the blood sample is taken again. The determination is carried out in the laboratory.
With the help of such an examination, the patient is diagnosed with or refuted a diagnosis of Helicobacter pillory infection and a diagnosis of atrophic gastritis. Doctors also determine the risk of developing cancer and peptic ulcers. The gastropanel allows the doctor to draw conclusions about the severity of the localization of gastritis (antrum, body or both sections), and also makes it possible to understand from which section of the stomach material should be taken for histological studies.
The level of pepsinogen I, gastrin-17, antibodies to Helicobacter pillory is determined in plasma or serum. The analysis is completed within 5 days.
Advantages and disadvantages of gastroscopy without swallowing a probe
The advantages of video gastroscopy are obvious:
- painlessness;
- safety;
- ease of preparation and use;
- All parts of the gastrointestinal tract are examined, including parts of the small intestine (with conventional gastroscopy - only the esophagus, stomach and duodenum);
- High quality shooting, a large number of photographs;
- fewer contraindications.
However, gastroscopy without swallowing the probe also has disadvantages:
- inability to target pathology (ulcers, neoplasms, etc.);
- lack of possibility of manipulation: taking a biopsy, administering medications, removing polyps;
- insufficiently detailed filming of the stomach walls;
- the high cost of the study, mainly due to the disposable capsule.
Why does capsule endoscopy not replace gastroscopy and colonoscopy?
09/28/2016 Despite the fact that the capsule passes through the entire gastrointestinal tract, it, unfortunately, cannot replace standard endoscopic examinations (fibrogastroscopy and colonoscopy), since it only fully examines the small intestine. But some clinics and Internet portals position capsule endoscopy as an alternative to FGDS and FCS, with which you can check both the stomach and large intestine at once. And in some cases, patients themselves decide that in this way they can save themselves from undergoing unpleasant colonoscopy and gastroscopy. In fact, this is a misconception and it can literally cost the patient dearly, because the average price for capsule endoscopy is about 40 thousand rubles, and most importantly, due to the lack of information, a possible serious pathology may go unnoticed.
The capsule is a miniature device with a built-in video camera that the patient swallows. While passing through the intestines, the video camera captures an image at a frequency of 2 frames per second and transmits it to an external storage device, after which the doctor uses a special program to view and analyze the resulting images.
During a standard FGDS, an endoscopist, using a flexible controlled probe, examines in detail the condition of the mucous membrane of the esophagus, stomach and duodenum. To straighten the walls of the gastric mucosa, which is necessary for a full examination, a little air is pumped into the stomach through a tube. If necessary, the doctor can take a biopsy and test for Helicobacter pylory. The same thing happens at the FCC. To straighten the folds of the large intestine, in which polyps, tumors, etc. may be hidden, air is also pumped into it during the examination. This is what causes the main pain during colonoscopy, since the intestine stretches when air is introduced into it, but this mandatory measure allows you to carefully examine the condition of the mucous membrane.
These functions are not available to the capsule. It is impossible to control its movement, therefore, once in the stomach, it can take a picture of only part of one of the walls of the stomach, from which it will in no way be possible to judge its condition as a whole. And since during capsule endoscopy the large intestine is not straightened, and the capsule moves uncontrollably through the colon, which is large enough to be viewed, the images it transmits from this section of the intestine are absolutely uninformative and cannot in any way be analyzed by a doctor. Capsule endoscopy is intended only for examining the small intestine. FGDS and FCS are quite unpleasant and even painful procedures, which is what pushes people to look for alternative diagnostic methods. In some cases, they can indeed be replaced, but not by capsule endoscopy, but by X-ray with barium, for example, or CT and MRI, which should be discussed with a doctor. But no other diagnostic will provide such detailed information about the condition of the mucous membrane of the esophagus, stomach and large intestine, which these standard endoscopic studies provide. This problem can be solved by performing FGDS and FCS under medicinal sleep. This is a shallow anesthesia that lasts about half an hour during the examination. And within an hour the patient will be ready to leave the clinic on their own. To conduct endoscopic examinations under anesthesia, you just need to first do an ECG and consult with an anesthesiologist. You can get advice on capsule endoscopy, FGDS, FCS and their possible alternatives in Clinical Hospital No. 122 from an endoscopist, gastroenterologist, Ph.D. Titov Alexey Nikolaevich.
Make an appointment with a gastroenterologist
or for endoscopic examinations
you can call:

Contraindications to video gastroscopy
Gastroscopy without swallowing the probe has fewer contraindications than conventional gastroscopy, but they still exist. As with conventional gastroscopy, the procedure is contraindicated in cases of narrowing and diverticula of the esophagus, mental disorders, epilepsy, pregnancy, increased gag reflex and in children under 12 years of age.
However, due to the fact that video gastroscopy uses electrodes, as well as an electronic receiver, this study is contraindicated in patients with pacemakers, neurological electrical stimulators, or any electrical implants. Due to the fact that the capsule passes through all parts of the gastrointestinal tract, there are contraindications associated with narrowing and obstruction of the intestine in any part of it.
Advantages of the gastropanel for the patient
In most cases, a gastropanel is sufficient to make a diagnosis and prescribe treatment. Thus, the patient does not need to think about where gastroscopy can be done and whether it is needed at all. If such intervention is necessary, doctors prescribe gastroscopy with biopsy.
Another indisputable advantage of the gastropanel is safety and convenience. If necessary, such examination can be done every three months. This is especially true for people over 45 years of age, for whom annual endoscopic examination is recommended, and in the presence of aggravating factors - every six months.
How to properly prepare for the procedure?
- During the day before taking blood, the patient should refrain from taking alcohol, medications, physical activity, and also not change their diet.
- The night before you need to go to bed at your usual time and get up no later than an hour before the examination.
- Before the examination, refrain from smoking.
- During the week before the gastropanel, refrain from taking medications that affect gastric secretion (Zantac, Somac, Ranil, Pepcidin, etc.).
- The day before the test, do not take medications that neutralize hydrochloric acid produced by the stomach (Librax, Prepulsid, Alsucral, etc.).
If the patient has difficulty stopping medications, he should definitely inform the doctor about this. It is very important to follow these recommendations, since otherwise it will not be possible to obtain valuable research results and you will have to do a gastroscopy or re-prepare for drawing blood from a vein.
Indications and contraindications of techniques
Gastroscopy and FGDS are indicated in the following cases:
- pain in any part of the abdomen;
- discomfort in areas of the gastrointestinal tract;
- sour taste in the mouth;
- frequent occurrence of heartburn;
- burning sensation in the esophagus;
- frequent nausea and vomiting;
- sudden unfounded decrease in body weight;
- violation of the swallowing process (dysphagia);
- the need for analysis to detect the Helicobacter bacteria;
- suspicion of gastritis;
- suspected peptic ulcer of the stomach or duodenum;
- stomach bleeding;
- to control the treatment process
Gastroscopy and FGDS examination are not recommended in the following situations:
- in the general serious condition of the patient;
- during hypertensive crisis;
- if blood clotting is impaired;
- for burns of the esophagus;
- for bronchial asthma during exacerbation;
- for acute cardiovascular diseases;
- in cases of severe parenchymal bleeding;
- for severe mental disorders
Indications for MRI and CT scan of the stomach:
- control of the development of the pathological process;
- suspicion of the presence of a benign or oncological formation;
- suspected gastric or duodenal ulcer;
- suspicion of the development of any abnormal process in the organ;
- calculating the stage of cancer and sites of metastasis
MRI of the stomach has a number of contraindications:
- the presence of foreign metal objects in the patient’s body;
- built-in electronic devices such as pacemaker, defibrillator, etc.;
- first three months of pregnancy;
- allergy to a contrast agent (with MRI of the stomach with contrast);
- severe renal failure
Contraindications to CT:
- renal and liver failure;
- diabetes;
- allergy to contrast agents;
- the entire period of pregnancy
Methodology
Gastroduodenoscopy is performed on an outpatient basis or in a hospital, including in the intensive care unit, when the study is prescribed for the purpose of hemostasis and for other emergency indications. The patient lies on the couch on his left side. After local anesthesia, a plastic ring is placed between the patient’s teeth. The specialist inserts the endoscopic tube under visual control along the anatomical axis of the oropharynx. When the endoscope is inserted into the esophagus, air (and sometimes water) is insufflated, as a result of which it becomes possible to pass the first bottleneck of the esophagus in its proximal part. After reaching the gastroesophageal sphincter, the subject is asked to inhale while insufflating air.
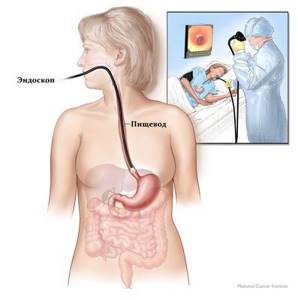
Once in the stomach cavity, the endoscopic tube, under the control of a physician, passes along the lesser curvature, after which the distal section of the endoscope bends, and the specialist is able to examine the area of the greater curvature. If indicated, the study includes a visual examination of the duodenal bulb and post-bulb section. To conduct endoscopy with examination of the entire length of the intestine, it is necessary to use a special duodenoscope with lateral optics. Also in this case, special preparation of the patient in the form of premedication is required, since the passage of an endoscopic tube from the stomach into the duodenum can be painful even in the absence of stenosis and other pathologies of the pylorus.
The duration of gastroduodenoscopy depends on the purpose of the study and is partly determined by the results obtained during the examination. The minimum time allotted for the procedure is about 2-5 minutes. If a biopsy sample is required for further histological examination, the duration of endoscopy increases.
Endoscopic examinations during sleep without pain are a common practice for modern medical institutions. The NIIEKM clinic has created all the conditions for high-quality, safe diagnostics and a comfortable stay for patients.
| Esophagogastroduodenoscopy (abbreviated as GASTROSCOPY or EGDS) | 2500 ₽ |
| Urease test for Helicobacter Pylori | 500 ₽ |
| Esophagogastroduodenoscopy under anesthesia with the provision of a bed, without taking into account the Helicobacter Pylori urease test | 6500 ₽ |
For detailed information, call the toll-free number 8 (800) 222-60-86.
Advantages of stomach diagnostic techniques
The main advantages of gastroscopy and FGDS are the ability to thoroughly examine the digestive tract centimeter by centimeter and carry out surgical treatment during the study.
The advantages of CT and MRI are the same, but the main difference is that MRI is a completely safe procedure and does not expose the patient to radiation, unlike CT:
- the ability to calculate tumor location;
- differentiation of formation features;
- diagnostics of organs of the entire abdominal cavity and assessment of their functioning;
- determining the stage of the disease;
- non-invasive and painless diagnostics;
Magnetic resonance imaging, unlike CT, is widely used to monitor the postoperative condition and the dynamics of the development of the clinical picture. To the question: “What is better for monitoring treatment, gastroscopy or MRI of the stomach?” You can give a positive answer in the direction of MRI.
Purpose of procedures
Gastroscopy is prescribed when the doctor suspects the presence of stomach diseases (gastritis, peptic ulcer), as well as the presence of neoplasms and parenchymal bleeding. Gastroscopy makes it possible to examine the stomach and esophagus in detail, and check the structure of the mucous membranes. In addition, the procedure is prescribed to take scrapings from the walls of the stomach or to collect gastric contents for a biopsy. To check the organs of the digestive tract using a gastroscope, there is a more informative alternative to gastroscopy of the stomach as FGDS.
The purpose of FGDS has similar prerequisites as standard gastroscopy. However, the suspicion of a duodenal ulcer is added to the indications of the procedure, since an elastic “hose” is also inserted into the duodenum area.
CT scan is prescribed mainly for diagnosing neoplasms of various types. As a rule, CT, like MRI, is an accurate and expensive research method, which is most often used to confirm the diagnosis established during gastroscopy or FGDS, as well as in cases where standard endoscopic examinations turned out to be not entirely informative. Computed tomography is valuable in identifying anomalies in the structure of an organ, guarantees their detailed study and differentiation, and allows obtaining high-quality images that display the physical condition of the organs.
MRI of the stomach is the main way to diagnose cancer. The information value of the method is difficult to overestimate, since the MRI scanner distinguishes not only the presence of tumors, but also their nature. Magnetic resonance imaging is often prescribed to determine the stage of the oncological process, identify the exact localization of cancer metastases, to assess the condition of the organ and tissues after surgery and in the presence of persistent pain in the gasrum and duodenum of an uncertain nature. MRI is used in almost the same cases as CT, since both methods are highly informative. But if you have to choose what is better to use, CT or MRI of the stomach, then you should give preference to magnetic resonance imaging. MRI does not expose the patient to radiation, while the principle of CT is based on scanning with x-rays, and due to this fact, CT is not allowed to be performed frequently.
More information about MRI of the stomach can be found here
Types of stomach diagnostics
- Gastroscopy. This procedure is a standard technique aimed at examining the esophagus and stomach. During the procedure, the doctor inserts a special gastroscope, which is an elastic tube made of a fiber optic system, through the patient's esophagus. The manipulation is carried out on the basis of characteristic indications, and the patient must refrain from eating 8-10 hours before the study. The insertion of an endoscope can cause a gag reflex and a number of other unpleasant sensations, therefore, in order to reduce discomfort, the patient's throat is treated with lidocaine. To avoid intense discomfort, the patient is advised to breathe deeply and relax the throat. Despite the invasiveness, the procedure is quite safe and painless if you fully follow the doctor’s instructions. Thanks to the air flow supplied through the endoscope, it is possible to examine the walls of organs in detail, as the air flow straightens them. If necessary, while the device is not removed, it is possible to perform a biopsy and other therapeutic measures.
- FGDS. The full explanation of the name is fibrogastroduodenoscopy. Essentially, this is the same gastroscopy, since the technique for both diagnostic procedures is identical. The only difference between FGDS and gastroscopy is the possibility of examining not only the epigastric part, but also the duodenal part, namely, the diagnosis of the duodenum.
- CT. Computed tomography is a modern way to diagnose the stomach and nearby organs. Thanks to CT technology, the doctor can examine the stomach cavity in a “section”. The procedure is non-invasive and painless. CT accurately determines the stages of cancer, the location of tumors and metastases, differentiates organs and tissues, and also contributes to the correct prescription of treatment. Computer diagnostics has many advantages, but has a significant disadvantage - a certain dose of radiation to the patient, which, with repeated use, can lead to changes in DNA cells. One-time use does not pose a major health hazard.
- MRI. Magnetic resonance imaging of the stomach is the safest and most painless examination method. The principle is the same as for CT scanning: the patient lies down on a sliding table, then slides inside the tomograph. However, there is a difference in these types of diagnostics. Magnetic resonance imaging, due to the influence of strong magnetic fields, does not provide the slightest dose of radiation, and therefore can be performed repeatedly. According to the opinions of radiologists, MRI provides the highest information content for diagnosing the stomach as a parenchymal organ. But in comparing magnetic resonance imaging with the endoscopic method, it is impossible to say for sure what is better: MRI of the stomach or gastroscopy. FGDS or gastroscopy are prescribed as the initial diagnosis, and if these are not possible, MRI is prescribed. In terms of comfort, MR imaging prevails.