What is CT brain perfusion: purpose
Perfusion is the process of circulating fluid through a capillary network. The process provides the brain parenchyma with oxygen, without which the functioning of the organ is impossible.
CT brain perfusion is designed to study and analyze the blood flow of the brain parenchyma. Perfusion computed tomography (PCT) is a more detailed and informative type of conventional computer scan of the brain. A contrast agent must be used during the procedure, which allows the vessels to be clearly traced on tomograms.
PCT analyzes the first stage of passage of blood saturated with a contrast agent using a pharmacokinetic model. Normally, the contrast element does not diffuse, is not metabolized, and is not absorbed by brain tissue. With pathology, pathological areas of accumulation appear, allowing the specialist to make a conclusion about the nature of the pathology.
It is convenient to conduct examinations after MSCT of the brachiocephalic arteries in order to fully study the blood supply and oxygen saturation of tissues.
Purpose of perfusion examination of brain tissue
CT brain perfusion is performed to achieve the following goals:
- Study of the condition of tumors after chemotherapy or radiation therapy;
- Analysis of the development of oncological tumors of the brain;
- Determination of areas for puncture sampling for the purpose of subsequent macroscopic examination;
- Study of disturbances in the blood flow process after strokes and injuries;
- Detection of occlusive type diseases (blockade of vascular patency);
- PCT of the brain visualizes the foci of stroke, its extent, and the depth of the lesion.
Retrograde perfusion to protect the heart - what is it?
Retrograde perfusion is not one of the ways to study the brain. The technique is used during surgical interventions in areas of the heart. Initially, it performed a protective function during operations of the cranial cerebral region, the conus arteriosus of the left ventricle, and the aortic arch. The use of the method by surgeons is uncommon. The method was previously used in conjunction with the treatment of blockage of the bloodstream by air particles, and later began to be used as a protective mechanism for targeted cooling of the body for artificial blood supply.
The perfusion technique is used by cardiac surgical medical institutions for the treatment of myocardial hypoxia when installing aortic valve prostheses, surgical correction of combined cardiac defects and correction of cardiac structural defects in infants.
Regional type perfusion is used, which is carried out by using a special device that records the flow of drugs through a catheter into the main vessel of the heart muscle’s own veins, arteries supplying blood to the myocardium. Performed under conditions of artificially created normal and low body temperature. Correction of defects in the structure of the heart is carried out through regional artificial blood supply to the heart while stopping the blood flow of other organs by squeezing the descending aorta. Coronary-carotid perfusion is performed by placing a catheter in the carotid arteries, superior and inferior vena cava, and the largest unpaired arterial vessel (aorta).
Carrying out the process at normal temperatures often leads to the accumulation of under-oxidized particles in the lower region of the body. The return of free radicals nullifies all previously obtained results. Perfusion during hypothermia smoothes the attitude of internal organs to oxygen starvation.
CT perfusion indicators
Cerebral blood flow is assessed based on the following indicators:
- The time it takes for the contrast agent to reach the required point in the brain;
- Availability of the required blood volume in the area of white matter being examined;
- Time of passage of blood flow through the vessels of the diagnosed brain region;
- The rate of blood circulation within tissues per unit of time.
The need for CT perfusion appears in those patients who suffer from cerebral circulatory disorders.
CT perfusion - contraindications
The study is contraindicated if the patient has an allergic reaction to the contrast element. The next contraindication is pregnancy, but if there is an urgent need for an examination, when a person’s life is at stake, perfusion must be done. Additionally, cisternography of the brain is performed if a stroke or intracerebral infarction is suspected.
For the safety of the unborn baby, a lead apron will need to be placed on the pregnant woman's stomach before the scan. The radiation dose will be negligible.
What is the difference between CT and MRI brain perfusion?
The main difference between these two types of brain imaging is tissue imaging. CT perfusion is focused more on determining the structure of dense tissues (bones, solid tumors), while MR perfusion better visualizes soft structures.
Both methods are comparable in the quality of the resulting images, and therefore are carriers of valuable information in the treatment of complex brain diseases. They are used in turn or in combination to obtain maximum information about the pathological area.
They also have an important difference in the principle of their operation. Computed tomography is performed using X-ray radiation, which, even to a small extent, is harmful to the patient’s health. MRI is based on the use of a magnetic field, which does not cause any harm.
The presence of metal objects (prostheses) inside the body will not allow examination on a multislice tomograph, but the use of a computer analogue is permitted.
Results and discussion
When analyzing the results of quantitative measurements of tumor blood flow in 111 patients, the highest values of blood volume (TBV) and blood flow velocity (TBF) compared with other tumor lesions of the CSR and the skull base area were identified in paragangliomas of the pyramid of the temporal bone and juvenile angiofibromas of the nasopharynx (Fig. 1) . These hemodynamic parameters were several times higher than those of most tumors included in the study, amounting to 30 ml/100 g, 709 ml/100 g/min, and 11 and 250, respectively (Table 2). The lowest quantitative values of TBV and TBF were recorded in cholesteatomas and chordomas (8.44 ml/100 g/min, 0.89 ml/100 g).
Table 2. Average values of absolute values of blood flow parameters for tumors and unaffected brain matter
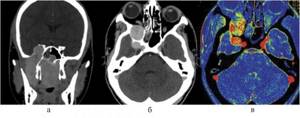
Rice. 1. Juvenile angiofibroma. Contrast-enhanced CT scan in frontal (a) and axial (b) projections, color map of blood flow volume (c). There is homogeneous contrasting of the tumor stroma with a pronounced increase in TBF.
In the largest group of observations with meningiomas, quite high (when compared with quantitative indicators in the white matter of the brain) values of blood flow velocity (109.25 ml/100 g/min) and blood flow volume (5.89 ml/100 g) were also revealed. At the same time, a pronounced increase in the permeability of tumor vessels was also noted at low transit times of the contrast agent (PS = 15.54, MTT = 4.18). The most common tumors in the group of meningiomas were those localized in the posterior cranial fossa and cavernous sinus (Table 3).
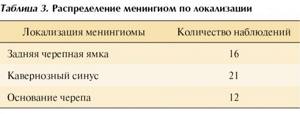
Table 3. Distribution of meningiomas by location
Histologically, the meningoteleomatous variant of the structure of meningiomas predominated (41 cases), while fibroblastic (2), psammomatous (1) and mixed (5) subtypes were also found. There were no statistically significant differences in blood flow parameters between different histological types of meningiomas. Taking into account the MR angiography data, the increased hemodynamic parameters were largely due to the abundance of blood supply to meningiomas - the larger the blood vessels feeding the tumor and the more pronounced the tumor vascular matrix, the higher the speed and volume of blood flow. Meningiomas of the wings of the sphenoid bone, the medial edge of the pyramid of the temporal bone, the petroclival region and the cavernous sinus had the most abundant blood supply. Tumors with minimal perfusion were convexital meningiomas of the occipital region.
Since our series of observations noted both high histological variability of tumors and quite diverse localization in the area of the skull base and CSR, which made it difficult to adequately compare tumors only on the basis of their hemodynamic characteristics (moreover, to a certain extent there was overlap in certain perfusion indicators between tumors and a small number of observations of individual histological variants), we divided the tumors into separate groups depending on the anatomical region and made comparisons taking into account clinical data and the results of structural neuroimaging.
When tumors are localized in the projection of the sella turcica and the perisellar zone, it is most often necessary to make a differential diagnosis between pituitary adenomas and craniopharyngiomas (CP). When analyzing blood flow in 8 cases with CF, we identified blood flow rates that were almost identical to those in the brain (17 ml/100 g/min) and slightly increased values of blood flow volume (up to 1.5 ml/100 g). At the same time, a relative prolongation of MTT and an increase in absolute permeability values were noted. In turn, among CF, SCT perfusion made it possible to differentiate tumors by histological type into adamantine-like (6 observations) and papillomatous (2) variants. Thus, in the subgroup of adamantine-like CF, low TBF and TBV values were detected, while papillomatous CF showed a moderate increase in TBF and high TBV values. The MTT and PS indicators turned out to be similar in both histotypes—prolongation of temporary values and increased permeability, respectively.
For 8 observations with pituitary adenomas, the absolute values of blood flow velocity in the tumor structure were higher compared to K.F. TBV and PS normalized for the brain (see Table 2) were also significantly higher in pituitary adenomas, which allows the use of perfusion in difficult diagnostic cases with atypical growth and localization of the formations presented.
Craniopharyngiomas with atypical growth and an unusual radiological picture also had to be differentiated from chordomas of CSR and, less often, from primary cancerous lesions. The difficulty of differential diagnosis of atypically growing CF, pituitary adenomas and chordomas sometimes lies in the similarity of x-ray semiotics (destruction of bone structures, the presence of petrification (up to 93% for CF [12] and up to 50% for chordomas [13]) and clinical symptoms. With the use of SCT- perfusion, the process of differential diagnosis has become more objective and specific. A distinctive common feature of chordomas in the area of the base of the skull, regardless of location, extent of bone destruction and degree of contrast enhancement, is the low values of all four indicators measured in our study, both absolute and relative ( normalized by brain) (see Table 2).
When tumors are localized in the area of the cavernous sinus, most often the differential diagnosis must be made between meningiomas and neurinomas, less often between cavernous hemangiomas and arterial aneurysms of the internal carotid arteries. In terms of frequency of occurrence in adults, meningiomas come to the fore, and in most cases, the correct diagnosis can be made using standard CT and MRI studies (tumor extent, contrast pattern, presence of “dural tails,” etc.). In case of problems in making a diagnosis, CT perfusion showed high sensitivity and specificity in diagnosing these formations (Fig. 1). According to our data, in 21 patients with cavernous sinus meningiomas, the latter were characterized by a significant increase in TBF and TBV, as well as high PS values (see Table 2), while in neuromas, TBF and TBV showed quite moderate or close to normal brain matter values (TBF=14.45, TBV=1.63 for neuromas), MTT prolongation (10.46 s), as well as an increase in PS (5.90). In arterial aneurysms, perfusion indices were close to those in the great vessels, and in 2 observations with cavernous hemangiomas, low values of hemodynamic indices and almost zero PS indices were revealed.
As daily clinical practice shows, the use of modern MRI and SCT capabilities in the assessment of CSO neoplasms (and these are mainly extracerebral lesions) in many cases makes it possible to fairly well visualize the volumetric process at the base of the brain, and sometimes even suggest a histological diagnosis of the neoplasm based on anatomical details. However, this applies mainly to pituitary tumors and to a lesser extent craniopharyngiomas, which are characterized by typically mid-localization, age-related differences and, in most cases, a clinical picture of hormonal dysfunction. At the same time, in a number of clinical cases, structural and anatomical data obtained on the basis of standard MRI and CT protocols, even with intravenous contrast enhancement, is not enough to judge the histological structure of the tumor and develop further treatment tactics. Some tumors, especially when they reach large sizes and prevalence, change the surrounding anatomical structures and acquire new structural properties, which significantly complicates their preoperative differential diagnosis. Moreover, structural neuroimaging methods do not provide an obvious answer regarding such an important aspect as the degree of vascularization of tumor tissue, necessitating the use of invasive interventions such as direct intraarterial angiography. Some CSR tumors, on the contrary, even with small primary sizes initially have similar clinical and diagnostic (including anatomical and radiological) signs. In these conditions, a minimally invasive SCT perfusion study with assessment of both structural and functional information about hemodynamic changes in tumor tissue can be considered the method of choice for non-invasive assessment of the histology of pathological processes in an area that is difficult to access for both direct surgery and stereotactic biopsy. The technique can also be used as an important additional diagnostic marker in the differential diagnosis of tumor and non-tumor lesions of the CSR and the skull base area.
The sensitivity and specificity of the SCT perfusion method in our study of space-occupying formations in the area of the skull base were 100 and 81.2%, respectively.
Radionuclide perfusion study
The basic principle of operation of radionuclide diagnostics of oncological diseases is the accumulation of certain radiopharmaceuticals in the tumor in a quantity greater than in healthy tissues. Saturation is explained by the penetration of these substances into the endothelium of unhealthy vessels, movement through the vascular wall into the interstitial (intercellular) area of the affected sector, as well as metabolism of the labeled compound by tumor cells.
After a computer study, the resulting images are examined and a conclusion is made about the existence or absence of a pathological formation at the molecular and cellular levels. Radionuclides are administered to the patient intravenously in small quantities, the radiation dose is comparable to the background radiation of the environment.
The methods are non-invasive and there are no side effects. The harm from radiotherapy during cancer search is secondary. Early verification of the tumor is more important.
Diagnosis of acute ischemic stroke using perfusion (information for doctors)
The perfusion screening technique makes it possible to detect and study in detail the smallest changes within the capillary blood flow that occur at different levels of the brain during the development of ischemic stroke. Performed after MSCT of the brain showing pathological areas.
The diagnosis was carried out on 18 patients (10 women, 8 men, average age 63 years) suffering from hemispheric ischemic stroke with moderate to severe neurological impairment. At the initial stage, these people performed a set of exercises to increase cerebral microcirculation. On the first day, the results of native CT without contrast injection and PCT were assessed. Re-evaluation was carried out on the third and tenth days. The section with the maximum area of perfusion disturbances was subjected to measurement of the area of sectors with altered bleeding parameters.
Treatment process
Treatment included standard reperfusion and antiplatelet therapy. Dynamics of growth in neurological parameters was observed on the stroke scale. The median area of the area of decreased CBV was 1386.73 mm2, decreased CBF - 2492.17 mm2, increased MTT - 2068.16 mm2. The time period from the onset of symptoms to the initial PCT was about 20 hours. The severity of the stroke at the first stage was 11 points according to NIHSS.
An exact decrease in the severity of neurological impairment was found on the 10th day after the onset of the disease to 8 points (Friedman test; p = 0.002). Attention was drawn to a significant drop in the sector of reduced CBF (to 1443.46 mm2; p=0.008), the area of the areas of corrected MTT and CBV remained the same (2117.69 mm2; p=0.497 and 1129.89 mm2; p=0.273).
After the first diagnosis, the parameters of the zone of reduced CBF were larger than the zone of impaired CBV, but subsequently, their sizes became comparable (p=0.059 and p=0.113, respectively).
The detected changes indicate the existence of an area of reversible blood circulation defects at the site of ischemia damage during the initial 24 hours after the onset of the disease. It is similar to an area of reduced CBF in the absence of CBV and MTT impairment. Regression of perfusion deviations of the ischemic focus occurs due to the stabilization of blood supply in this area, but the lack of circulation in the zone of altered MTT and CBV remains with the same parameters.
conclusions
PCT is a valuable tool for analyzing the development of pathophysiological features of ischemic stroke at an early stage, when other methods fail to obtain valuable diagnostic information.
Clinical experience shows that, at little cost, it is possible not only to diagnose ischemic stroke in the first hours of symptom onset, but also to determine the difference between the presence of viable tissue and irreversibly affected areas.
Subsequently, this makes it possible to determine the likelihood of undergoing systemic thrombolytic therapy, not based solely on data on the rate of disease progression.
conclusions
SCT perfusion is a minimally invasive, clinically accessible imaging tool that provides additional information about the degree of vascularization of tumor tissue, making it a good assistant in the differential diagnosis of neoplasms of the skull base. Compliance with certain hemodynamic criteria with a comprehensive assessment of structural and functional information allows us to make the correct histological diagnosis at the preoperative level with a high degree of confidence, making this technology an “ in - vivo”
-histology". I would like to note the important role of this technique in the assessment of tumors located in an area of the intracranial space that is difficult to access for both direct surgery and stereotactic biopsy. The integrated use of CT and MRI technologies allows not only to improve the differential diagnosis of neoplasms, but also to bring to a higher level of reliability the assessment of the treatment performed, as well as postoperative and post-radiation pathomorphosis.