The pituitary gland is an endocrine organ located on the undersurface of the brain in a bony pocket called the sella turcica.
It produces or stores hormones that regulate most metabolic processes in the body.
The anterior, middle and posterior lobes of the pituitary gland, located in the sella turcica.
The anterior lobe of the pituitary gland secretes so-called tropic hormones that regulate the functioning of certain glands:
- thyroid-stimulating controls thyroid function;
- adrenocorticotropic - stimulates the adrenal cortex;
- gonadotropic - regulate the formation of follicles in the ovaries, ovulation;
- somatotropic - responsible for protein synthesis and tissue growth;
- Prolactin – ensures lactation and other hormonal processes.
The posterior lobe of the pituitary gland accumulates a number of important hormones, for example:
- vasopressin - regulates kidney function, the amount of water in the body and pressure in blood vessels;
- Oxytocin - promotes uterine contractions and the release of breast milk.
The middle lobe of the pituitary gland produces melanocyte-stimulating hormone, which promotes the production of pigment in the skin, hair and retina.
What is MRI of the pituitary gland?
Magnetic resonance imaging allows you to obtain a three-dimensional image of the gland and detect changes in it that are not detected using other research methods. Scanning based on magnetic resonance technology is safe, since the patient’s body is not exposed to x-ray radiation, is painless and informative, especially when diagnosing diseases of the central nervous system, when examination of small brain structures is required.
MRI of the pituitary gland shows changes in the tissue of the gland, even if the affected areas are very small or their visualization is difficult. The pituitary gland is clearly visible on MRI of the brain
, however, if necessary, a specialist may prescribe a more detailed study.
Why do you need to be tested for pituitary hormones?
Donating blood for pituitary hormones is a test that allows the doctor to identify or confirm the diagnosis for the following diseases:
- gigantism;
- acromegaly (enlargement of body parts in the patient);
- diabetes insipidus;
- pituitary dwarfism;
- Itsenko-Cushing's disease;
- pituitary hypogonadism;
- pituitary hypothyroidism;
- gipyerprolaktinyemiya;
- Sheehan's syndrome.
The timing of blood tests for pituitary substances depends on the laboratory in which the study is carried out. The validity period of hormonal tests should be checked with your doctor.
Pituitary gland: what it is, description and functions
The pituitary gland is a small (up to 1 gram) gland located at the base of the brain. The hormones secreted by the pituitary gland are involved in regulating the functioning of the entire human endocrine system. Disturbances in the functioning of the pituitary gland affect the functioning of the entire body, cause changes in development, and can cause obesity, infertility, and other pathological conditions.
Pituitary tumors, among which adenoma is the most common, are well identified using MRI, which allows timely treatment to begin.
Pituitary adenomas of the brain
Pituitary adenomas are benign tumors that arise primarily from the anterior glandular portion of the pituitary gland (adenohypophysis). Neurohypophyseal tumors (from the posterior lobe) are extremely rare.
What are micro- and macroadenomas?
Microadenoma: pituitary tumor <1 cm in diameter. Larger tumors are considered macroadenomas. Currently, using modern neuroimaging methods, 50% of pituitary tumors at the time of their discovery have Ø<5 mm.
How common are pituitary adenomas?
Pituitary tumors account for ≈10% of intracranial tumors. But taking into account autopsy data, their frequency is slightly higher. They are most often observed in the 3-4 decades of life with equal frequency in men and women. In 10% of cases, adenomas can be detected in children.
Clinical manifestations of pituitary tumors
Pituitary tumors can manifest themselves both as a violation of the patient’s hormonal status and as a volumetric effect on adjacent neural and vascular structures, primarily on the visual pathways
Based on hormonal activity, pituitary tumors are divided into two groups: - secreting (hormonally active) - often have early manifestations in the form of symptoms that cause physiological effects in accordance with the excess of the hormones that they secrete. - non-functioning (hormonally inactive) - which are either non-secreting or secrete gonadotropin, which does not cause endocrinological symptoms). Non-secreting hypertension usually manifests itself as neurological disorders due to its large size and effects on adjacent brain structures. The visual pathways are often the first to be affected. Headaches are common. Seizures with pituitary adenomas are rare. In rare cases, adenomas may present with pituitary apoplexy. Even more rarely, with invasive growth into the base of the skull, they can manifest as rhinorrhea. With predominant growth under the base of the frontal lobes, changes in the psyche are possible. With large adenomas growing predominantly upward, blockage of the interventricular foramen of Monroe is possible, with the development of occlusive hydrocephalus.
Rice. 1. Clinical manifestations at different levels of damage to the chiasmatic-sellar and hypothalamic-physeal regions
What is pituitary apoplexy?
Acute onset neurological deterioration, usually manifesting as headache, visual disturbances, ophthalmoplegia (unilateral or bilateral), and altered mental status. Usually occurs as a result of an increase in the size of the formation within the sella turcica as a result of hemorrhage, or necrosis, or infarction of the tumor and adjacent pituitary tissue.
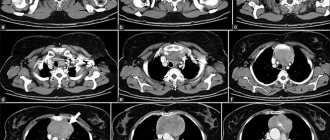
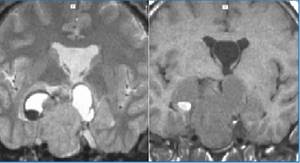
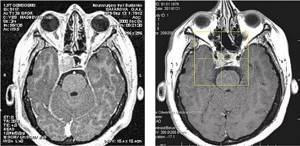
Rice. 2. Pituitary macroadenoma with hemorrhage and occlusive hydrocephalus
Secreting tumors of the pituitary gland;
Most often, hormonally active pituitary tumors secrete one of the following hormones:
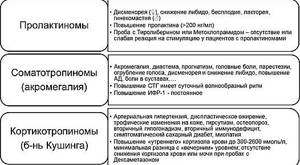
- Prolactinomas secrete prolactin (PRL). They are the most common functioning adenomas. They cause amenorrhea-galactorrhea syndrome in women, impotence in men and often infertility in both.
- Corticotropinomas – secrete adrenocorticotropic hormone (ACTH), leading to Cushing's disease or Nelson's syndrome: hyperpigmentation (due to cross-action of ACTH with melanin-stimulating hormone). Occurs in 10-30% of patients undergoing adrenalectomy for SS
- Somatotropinomas – secrete growth hormone (GH), which causes acromegaly in adults. In prepubertal children (before the epiphyseal growth zones close), it can cause gigantism (this happens very rarely).
Rare types of pituitary adenomas:
- Thyrotropinomas: causes thyrotoxicosis
- Gonadotropinomas: secrete luteinizing hormone (LH) and/or follicle-stimulating hormone (FSH). Usually there are no clinical manifestations
Table 1. Clinical manifestations and diagnostic tests of the main types of secreting pituitary adenomas
What is the best way to diagnose pituitary adenomas?
MRI is the diagnostic method of choice. Provides information about the invasion of the tumor into the cavernous sinus, about the localization and/or involvement of the parasellar part of the internal carotid artery, about the relationship of the tumor to the visual pathways. In 25-45% of cases, an MRI without contrast enhancement may not show the tumor. Microadenomas in 75% have a low signal in the T1 mode and a high signal in the T2 mode (however, in 25% of cases the signals can be any and, in particular, even directly opposite to those indicated above). The accumulation of contrast depends on time. To detect a microadenoma, images must be acquired within 40 seconds of contrast injection. Initially, the contrast enhances the signal of normal pituitary tissue (due to the absence of the blood-brain barrier) rather than the tumor. After 5 minutes, the same signal enhancement is observed in the tumor.
For the diagnosis of macroadenomas, this scanning mode is not decisive
Which treatment method for pituitary adenoma should I choose?
Treatment of pituitary adenomas is a complex task at the intersection of endocrinology and neurosurgery. Unlike most other tumors, it is necessary to resolve the issue of not only the volumetric effect of the tumor on adjacent brain structures, but also to suppress the indirect effect of pathological hormonal activity on other internal organs. Today, the established and generally accepted practice in the treatment of pituitary adenomas is complex treatment, using different methods of influence at different stages of the disease, depending on the clinical manifestations and effectiveness of treatment. In determining treatment tactics, a multidisciplinary approach is always used with the involvement of doctors of specialized specialties
Conservative treatment
The following medications are used (for specific types of tumors): - dopamine agonists: bromocriptine, pergolide, cabergoline (for prolactinomas) - long-acting somatostatin analogues: octreotide (for acromegaly) - serotonin antagonists: cyproheptadine (for Cushing's disease) - cortisol secretion inhibitors: metyrapone , ketoconazole, mitotane (for Cushing's disease) - decongestants: dexamethasone (for pituitary apoplexy)
Surgery
It is carried out in case of ineffectiveness or impossibility of conservative treatment, in the presence of severe symptoms of the volumetric effect of the tumor on the brain, in the development of tumor relapses. Considering the anatomical location of the pituitary gland in the sella turcica, the transnasal transsphenoidal approach is currently most widespread, incl. using neuroendoscopes with different viewing angles. The use of this technique allows operations to be performed with minimal trauma, however, this method has its limitations and capabilities. For giant adenomas involving several areas of the skull base, transcranial (via trepanation) approach is practiced, allowing to remove those parts of the tumor that are inaccessible from the transnasal approach. Total removal of hormonally active tumors allows not only to eliminate compression of neighboring structures, but also to quickly normalize the level of pituitary hormones.
Radiosurgery
It is used in cases where radical tumor removal is impossible, or when tumor relapses develop, incl. hormonally active, if conservative treatment is ineffective or impossible.
A feature of radiosurgery is a gradual, over approximately 2-3 years, reduction of hormones to normal levels. At the same time, radiosurgery of hormonally active adenomas involves the use of significantly higher doses at the edge of the tumor, in comparison with non-secreting tumors.
Clinical example 1. Endosupralatero(D)sellar somatotropic pituitary adenoma. Acromegaly, active stage. Condition after endoscopic removal of pituitary adenoma (2005). Continued tumor growth. On the left - at the time of Gamma Knife radiosurgery. Tumor volume - 5.3 cc. Prolactin - 2300 mU/l (normal is up to 530) STH - 13.7 mU/l (normal is up to 10) On the right - 3.5 years after Gamma Knife. Tumor volume - 1.9 cc. Normalization of the level of pituitary hormones and active factors: prolactin - 214 mU/l (normal up to 530), STH - 1.07 mU/l (normal up to 10), IGF-1 - 292 ng/ml (norm up to 295.5)
BIBLIOGRAPHY:
- Pituitary adenomas. Clinic, diagnosis, treatment\\ed. prof. B.A. Kadasheva, M. 2007
- Stereotactic Radiosurgery for Patients with Pituitary Adenomas//Radiosurgery Practice Guideline Initiative, ISRS 2004
Secreting tumors of the pituitary gland;
Most often, hormonally active pituitary tumors secrete one of the following hormones: 1. Prolactinomas - secrete prolactin (PRL). They are the most common functioning adenomas. They cause amenorrhea-galactorrhea syndrome in women, impotence in men and often infertility in both. 2. Corticotropinomas - secrete adrenocorticotropic hormone (ACTH), which leads to Cushing's disease or Nelson's syndrome: hyperpigmentation (due to the cross-action of ACTH with melanin-stimulating hormone). Develop in 10-30% of patients undergoing adrenalectomy for CC 3. Somatotropinomas - secrete growth hormone (GH), which causes acromegaly in adults. In prepubertal children (before the epiphyseal growth zones close), it can cause gigantism (this happens very rarely).
Rare types of pituitary adenomas: 1. Thyrotropinomas: cause thyrotoxicosis 2. Gonadotropinomas: secrete luteinizing hormone (LH) and/or follicle-stimulating hormone (FSH). Usually there are no clinical manifestations
Hormones secreted by the pituitary gland
Pituitary hormones regulate the functioning of the thyroid gland and adrenal cortex. They are responsible for the growth of the body and reproductive function. Excessive production of somatotropin by the pituitary gland can cause gigantism and acromegaly (excessive growth of limbs, facial changes). The pituitary gland is responsible for the production of prolactin, which regulates lactation in women, and oxytocin, which is responsible for labor.
The normal functioning of the pituitary gland determines the timeliness of the onset of puberty in adolescents.
MRI of the pituitary gland, hypothalamus, area of the sella turcica with and without contrast
A group of glands of the endocrine system regulates the activity of internal departments.
Two main organs - the hypothalamus and pituitary gland - control the concentration of hormones - biologically active substances that affect metabolism, vital activity, body growth, and the performance of departments. The hypothalamus ensures the interconnection of the nervous and endocrine systems, regulates the functionality of the pituitary gland, which controls the underlying parts of the hormonal sphere.
Pituitary hormones control the functions of many body tissues. The gland regulates the efficiency of metabolic processes of other components of the neuroendocrine system.
The hypothalamic-pituitary region occupies the sella turcica (part of the temporal bone).
When is it necessary to do an MRI of the pituitary gland?
MRI of the pituitary gland is prescribed for frequent headaches and progressive disorders in the functioning of the brain, for visual impairment of unknown cause, weight changes (for example, for obesity not caused by excessive food consumption and a sedentary lifestyle) and other painful conditions.
Indications
- Traumatic brain injuries.
- Erectile dysfunction in men.
- Menstrual cycle disorders in women.
- Increased activity of certain groups of hormones, including high levels of prolactin.
- Suspicions of hormone-dependent diseases (acromegaly, Itsenko-Cushing syndrome).
- Infertility.
Contraindications
There are few contraindications to the study. Absolute contraindications:
- The presence of implants or electronic devices in the patient’s body, including a pacemaker, insulin pump, joint endoprosthesis, metal clips on blood vessels.
- Pregnancy (all trimesters – for MRI with contrast, 1st trimester – for MRI without contrast).
- Allergy to contrast agent.
The procedure is not performed if the patient weighs more than 120 kg, which is dictated by the technical requirements of the device.
Patients with heart, kidney, or liver failure should discuss with their doctor the feasibility of the study and possible risks if a contrast agent is to be used.
Indications and contraindications
Indications for MRI of the pituitary gland are:
• recurring headaches of unknown localization; • visual impairment (significant decrease in acuity, narrowed visual fields, increased intraocular pressure); • impaired eye motility; • suspicion of a pituitary tumor; • endocrine disorders; • increased blood levels of prolactin and other pituitary hormones; clinical manifestations of hormonal deficiency of these hormones may be dwarfism or gigantism, diabetes insipidus, acromegaly, etc.; • head injury with brain damage.
Contraindications are divided into absolute and relative.
Absolute:
• presence of a metal foreign body in the eye socket or brain; • ferromagnetic clips applied to intracranial vessels (aneurysm); • electronic devices in the body (pacemaker, etc.); • aplastic anemia, that is, associated with impaired hematopoiesis in the bone marrow (contrast is contraindicated).
Relative:
• external pacemaker; • severe fear of closed spaces (claustrophobia) (there is an option for performing MRI on an open type machine, but they have less resolution); • inappropriate behavior in case of mental disorders; • pregnancy in the 1st trimester, because there is no data on the absence of influence of the magnetic field on the fetus; • intracranial aneurysm with a non-metallic clip applied; • inability to ensure a fixed position; • metal prostheses or clips outside the study area; • extremely serious general condition requiring monitoring of vital functions; • drug and alcohol intoxication; • age up to 7 years (due to the difficulty of ensuring a long-term immobile position); • the patient is overweight (the specific limit depends on the brand of the device).
Titanium implants are not a contraindication.
Advantages of the method
The main advantage of MRI is its high information content, the ability to study tiny structures that are poorly distinguishable with other neuroimaging methods. The small number of contraindications, painlessness and non-invasiveness of the procedure also speak in its favor.
Magnetic resonance imaging can detect pathological changes in the gland at their very beginning, including inflammatory processes, benign and malignant neoplasms, and changes in the vascular bed. High image quality makes it possible to identify microscopic areas of lesions.
How is an MRI examination of the sella turcica performed?
Before entering the room with the MRI scanner, you need to get rid of all metal elements (jewelry, watches, all items of clothing containing metal). In certain diagnostic centers, a person is given the opportunity to change into a robe or a specially designed loose-fitting shirt.
The patient is placed inside the device in a supine position. The diagnostician constantly communicates with the patient using a loudspeaker.
The specific duration of an MRI session of the sella turcica always depends on the equipment model, the size of the area being examined, and the need for a contrast amplifier. The average is about 45 minutes.
During the MRI of the sella turcica, you will need to remain motionless. The pituitary gland area is small, so sections are made every 1-3 mm. The overall scan time takes a long time.
After completing the process of magnetic resonance imaging of the sella turcica, the patient will have to wait a little while the specialist deciphers the information received.
How is MRI of the pituitary gland performed, how long does it take?
Special preparation is required only for MRI of the pituitary gland with contrast.
Before a routine examination, you will need to remove metal jewelry, hairpins, and watches. Wallets with credit cards, pens and glasses will also have to be left outside the room where the device is installed.
The patient is positioned on a movable table, which moves inside the tomograph for the examination. The entire study takes from 30 to 60 minutes, during which time you must lie still so that the results are not distorted (fixing belts may be used).
To make MRI of the pituitary gland more comfortable, it is recommended to use earplugs or special headphones, since the noise of the machine can cause discomfort.
Carrying out tomography
If the scan is performed with contrast enhancement, an iodine-containing drug is administered 10-15 minutes before the start of the study. The dosage is determined individually in each individual case.
The patient is placed on the retractable couch of the device, to prevent spontaneous movements, the arms and legs are secured with special straps. For panic attacks and anxiety, sedatives are used.
During the study, the doctor is in the next room, from where he monitors the study. Communication with the patient is maintained via a microphone. The duration of the tomography is 20-60 minutes.
MRI of the pituitary gland: what does it show with increased prolactin?
Magnetic resonance imaging of the pituitary gland is often prescribed for elevated levels of prolactin in the blood. The fact is that high prolactin can serve as a sign of the development of a pituitary adenoma, a benign tumor that can cause disturbances in the functioning of the entire body, including endocrine diseases.
MRI with elevated prolactin shows the presence or absence of a pituitary adenoma, other pathological changes in the tissues of the gland, and allows us to identify the reasons for the increase in hormone levels. Timely diagnosis of adenoma allows you to avoid such serious consequences as infertility and loss of vision.
Is it possible to do tomography of the temporal region for women during pregnancy and infertility: contraindications
To prepare for scanning, representatives of the fairer sex are required to provide a certificate stating that they are not pregnant. If a woman is pregnant, the test will only be done if absolutely necessary.
The specialist should know about pregnancy. There is no established evidence that MRI is harmful to the fetus, but the session should be avoided during the first three months. The temporary delay is explained by the effect of the device’s force field on the body over a long period of time. MRI with contrast is contraindicated for pregnant women.
Infertility is not a contraindication for MRI of the temporal region. Women who have an excessive amount of prolactin in the blood are sent for an MRI of the brain, which is necessary to verify the presence/absence of a pituitary tumor.
How much do pituitary hormone tests cost?
Tests for pituitary hormones are included in the list of tests for which a discount is provided. The price in the table does not include discounts!
| [13-010] | Antibodies to the TSH receptor (anti-pTTH) | 1825 |
| [13-087] | Antithyroglobulin antibodies (antiTG) | 600 |
| [13-088] | Antibodies to thyroid peroxidase (anti-TPO) | 580 |
| [08-051] | Tireogloʙulin | 940 |
| [08-119] | Follicle stimulating hormone (FSH) | 485 |
| [08-111] | Luteinizing hormone (LH) | 495 |
| [08-122] | prolactin | 525 |
Other prices can be found in the clinic’s price list or from the clinic administrator.
What does magnetic resonance imaging of the pituitary gland show?
- Microadenomas are tumors up to 10 mm in size. Typically, such tumors are characteristic of the anterior pituitary gland. They are accompanied by excessive secretion of prolactin.
- Craniopharyngiomas are tumors of the pituitary gland that usually occur in young children. The characteristic symptoms of such tumors are pressure on adjacent areas of the pituitary gland. Moreover, this type of tumor can cause significant compression on the optic nerve and, as a result, cause visual impairment. Sometimes this leads to intracranial hypertension and severe headaches.

A small pituitary cyst does not manifest itself, but as it grows, it can lead to compression of brain structures and the appearance of increasing headaches.- Pituitary apoplexy - the danger of this neoplasm is associated with the fact that some areas of the pituitary gland begin to bleed. As a result, this leads to the destruction of the pituitary gland as a whole. As a result, endocrinological disorders begin. Due to circulatory disorders, serious dyshormonal abnormalities begin. Such disorders are called pituitary stroke and pose a real threat to life.
To detect small tumors, several images of dynamic MRI using a contrast agent will be the optimal solution. since such images are more informative and allow you to visualize the affected area.
Prices for services
| Name | Time | Price |
| MRI of the brain and examination of the pituitary gland | 7000 | |
| MRI of the pituitary gland | 4000 | |
| MRI of the pituitary gland. | 4000 |
Pituitary hormone analysis: preparation
Rules for preparing for tests may vary depending on which hormone is the object of medical interest.
- If you are planning a blood test for follicle-stimulating hormone (FSH), you must take the biological material on an empty stomach (at least 12 hours without food). Men can undergo this study absolutely on any day, while women are recommended to do this on days 19-21 or 3-8 of the cycle.
- If the object of study is luteinizing hormone, women are recommended to choose the same days of the cycle for the blood test as in the previous version, and men are advised to take it at any time. It is mandatory to refrain from eating for approximately 8 hours before the test.
- Prolactin in women is diagnosed twice a month, in the first two phases of the cycle; blood testing is required in the morning and on an empty stomach. It is also necessary to rest approximately half an hour before collecting biological material.