- Types of pancreatic cancer
- Localization of pancreatic cancer
- Stages of pancreatic cancer
- Causes of pancreatic cancer
- Can pancreatic cancer be prevented?
- Symptoms of pancreatic cancer
- Diagnosis of pancreatic cancer
- Pancreatic cancer: ICD-10 code
- Pancreatic cancer treatment
- Nutrition for pancreatic cancer
- Prevention of pancreatic tumors
- Pancreatic cancer: life expectancy
- Prices for treatment of pancreatic cancer
Pancreatic cancer is one of the most insidious and dangerous cancer diseases. It is asymptomatic for a long time, and when it makes itself felt, as a rule, it turns out to be incurable. But even if the diagnosis is made at an early stage, the five-year survival rate is no more than 15%. Due to the fact that the gland is located deep and surrounded by other abdominal organs, operations on it are complex and require great skill from the surgeon. There is a high risk of serious and sometimes fatal postoperative complications.
Malignant tumor of the pancreas in facts and figures:
- It ranks sixth in frequency among other cancers in adults.
- According to American statistics, pancreatic malignancies account for about 3% of all cancers and cause 7% of mortality from all types of cancer.
- Most often, the tumor occurs in people over 60–65 years of age.
- Men and women get sick equally often.
- In 50–60% of cases, the tumor affects only the head of the pancreas, in 10% the body, and in 6–8% the tail. In 25–30% of cases, the entire pancreas is affected.
Types of pancreatic cancer
The pancreas contains exocrine tissue, which produces digestive enzymes, and endocrine tissue, whose function is the production of certain hormones. Accordingly, depending on the origin, exocrine and endocrine malignant tumors of the pancreas are distinguished. The former are much more common. When people talk about pancreatic cancer, in most cases they mean exocrine tumors.
Adenocarcinoma , a tumor of glandular cells, is the most common type of exocrine cancer. It occurs in 80–95% of cases. In most cases, the tumor originates from the cells lining the pancreatic ducts - ductal adenocarcinoma. Less common are neoplasms from cells that produce digestive enzymes in the acini. This type of cancer is called acinar cell cancer.
Separately, intraductal papillary and cystic mucinous tumors associated with invasive cancer . These tumors are benign, but over time they can transform into cancer. People diagnosed with these pathologies should be seen by a doctor. Cystic tumors are usually removed surgically due to the risk of malignancy. Papillary operate under certain conditions, for example, if the tumor is in the main duct.
Rarer types of malignant tumors of the pancreas: squamous cell, undifferentiated, adenosquamous carcinoma, cystadenocarcinoma, signet ring cell carcinoma.
Less than 5% of all pancreatic tumors are tumors that develop from endocrine cells - neuroendocrine tumors , or islet cell tumors. These include gastrinomas, insulinomas, glucagonomas, and somatostatinomas. Most often they are benign, but they can turn out to be malignant, and even a biopsy does not always help to establish the correct diagnosis in time.
Book a consultation 24 hours a day
+7+7+78
Treatment
For pancreatic cancer, treatment directly depends on the stage of the disease.
- Surgery is the main method in the first or second stage, after which chemotherapy is prescribed to destroy residual malignant cells. Depending on the degree of damage, the organ is removed completely or partially.
- Chemotherapy is the first step in a long-term treatment regimen for stage three. If it helps reduce the spread of the tumor, surgery is performed to remove the gland. Together with the pancreas, the duodenum, part of the small intestine and/or stomach, and the gallbladder with ducts can be removed.
- Radiation therapy is prescribed to the patient if chemotherapy is unsuccessful and surgery is considered impossible.
- At the fourth stage, the tumor is usually inoperable, so the patient is prescribed only chemotherapy to reduce the growth rate of malignant cells and prolong the patient's life.
- Patients with neuroendocrine tumors are operated on at any stage, after which courses of chemotherapy are prescribed.

Localization of pancreatic cancer
A malignant tumor can be located in the head, body or tail of the pancreas. Depending on the location, it will have some features.
Pancreatic head cancer
The most common cancer is the head of the pancreas. For example, about 75% of ductal adenocarcinomas are localized here. Malignant tumors removed from the head are on average 2.5–3.5 cm in size, while those in the body and tail are usually larger. However, due to the close location of the bile duct, even small neoplasms of the head can compress it and lead to obstructive jaundice. Other typical complications include duodenal stenosis and bleeding from disintegrating cancer.
Pancreatic body cancer
The body of the pancreas is the second most common site of cancer in the organ. Ductal adenocarcinomas occur here in 18% of cases. If the tumor is located in the body or tail, then complications such as thrombophlebitis, phlebothrombosis, and diabetes mellitus are more common than cancer of the head. Apparently, this is due to the fact that the neoplasms of the body and tail are larger in size. If jaundice occurs, it usually indicates advanced cancer.
Pancreatic tail cancer
Cancer of the tail of the pancreas is the least common. Only 7% of ductal adenocarcinomas have this localization. Due to the proximity of the stomach, colon and lung, such tumors are more difficult to detect during ultrasound.

Treatment at various stages
Specialists at our Oncology Center in Moscow develop treatment regimens for pancreatic cancer on a strictly individual basis. Doctors take into account the histological type of tumor, its location, the patient’s general health, etc. But the most important parameter is the stage of development of the oncological process.
The most effective method of treatment at the moment remains surgery. It is almost always supplemented with pharmacological and radiation therapy. In the early stages of the existence of a malignant neoplasm, it can be eliminated by operations of various scales:
- Whipple operation - removal of the head of the gland;
- segmental resection - removal of the body of the gland with subsequent connection of its remaining parts;
- distal resection – removal of the body and tail of the gland;
- total resection – removal of the entire gland.
These interventions will be effective on:
- stage zero (the tumor is represented by only a certain number of malignantly degenerated cells in one place);
- first stage (the tumor is entirely in the gland, without affecting either the lymph nodes or other organs):
- second stage (the tumor has spread to the tissues and lymph nodes surrounding the gland, but has not yet grown through the walls of neighboring large vessels).
Also, all nearby lymph nodes are often removed for preventive purposes. In addition, at the second stage, those parts of other organs into which the malignant process has managed to spread are also subject to excision: areas of the duodenum, stomach, gall bladder, etc.
At the third (tumor growth through the walls of large vessels) and fourth (metastases in distant organs) stages, palliative surgical interventions are mainly performed. Their goal is to improve the patient’s quality of life and eliminate the most severe symptoms of a pancreatic tumor. These can be operations on:
- removal of those parts of the tumor that put pressure on surrounding organs, disrupting their functions, or compress blood vessels and nerve pathways;
- removal of the largest metastases, often in combination with HIPEC (Hyperthermic Intra Peritoneal Chemotherapy), an innovative method of hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis.
- elimination of obstruction of the biliary tract or intestines, including by applying stents and anastomoses;
- suturing pathological holes in the walls of adjacent hollow organs.
Stages of pancreatic cancer
Classification of pancreatic cancer by stages is based on the generally accepted TNM system.
The letter T denotes the characteristics of the primary tumor. T1 - a tumor that is located within the pancreas, has a size of up to 2 cm (T1a) or more (T1b) and does not grow into the capsule, vessels, or neighboring organs. Stages T2 and T3 indicate varying degrees of cancer growth into different structures.
The letter N indicates that cancer cells have spread to the lymph nodes. N0 - there are no foci in the lymph nodes. N1,2,3 - spread of cancer to various groups of lymph nodes.
M is the presence (M1) or absence (M0) of distant metastases.
Depending on combinations of different T, N and M values, pancreatic cancer is divided into four stages with substages:
| N0 | N1 | N2 | N3 | |
| T1a | I | II | III | Iva |
| T1b | I | II | III | Iva |
| T2 | III | III | Iva | IVb |
| T3 | IVa | IVa | IVb | IVb |
| Any T and N, M1 | IVb | |||
Pancreatic cancer with metastases
Pancreatic cancer with metastases (stage IVb), unfortunately, is common: it is diagnosed in 45–55% of patients. Typically, secondary lesions are located in various parts of the abdominal cavity, liver, lungs, and bones. Radical treatment in such cases is impossible, but doctors can relieve pain and other painful symptoms and prolong the patient’s life.
Metastases in the pancreas
Sometimes a tumor found in the pancreas is actually a metastasis of cancer in another organ. This happens rarely: metastatic cancer accounts for only 2% of all malignant pancreatic tumors. The primary tumor is most often located in the lungs, mammary gland, kidneys, gastrointestinal tract, and prostate gland. Sometimes melanoma, osteosarcoma, leiomyosarcoma, and Merkel carcinoma metastasize to the pancreas.
Stages
Oncologists distinguish four stages of pancreatic cancer.
- A small tumor does not spread beyond the organ, without metastases.
- Malignant cells extend beyond the gland, but large vessels are not involved in the process. Metastases in regional lymph nodes are possible.
- The tumor grows into large vessels, affects most regional lymph nodes, but does not metastasize to other organs.
- The size of the tumor does not matter; the tumor actively metastasizes through large blood arteries to the lungs, liver, spine and bones, through the lymph flow to distant lymph nodes, as well as to the intestines, stomach and other peritoneal organs.
Causes of pancreatic cancer
There are risk factors that provoke the development of malignant tumors in the pancreas. The main ones:
- Diabetes. For unknown reasons, the risk of the disease is increased in people with type 2 diabetes. The risks in patients with type 1 diabetes have not been studied.
- Cholelithiasis.
- Chronic pancreatitis. The risk is especially high in smokers. However, not all people have chronic inflammation in the pancreas tissue that leads to the development of a tumor.
- Cirrhosis of the liver. There is some evidence that this disease causes pancreatic cancer.
- Some hereditary factors: family history of pancreatic carcinoma, BRCA2 mutation, Lynch syndrome, multiple dysplastic nevi syndrome.
- Associated with melanoma.
- Tobacco smoking. One of the main risk factors. It is known that about 20–30% of cases are associated with smoking cigarettes, pipes, and cigars.
- Frequent drinking of alcohol. A direct cause-and-effect relationship between alcohol intake and pancreatic cancer has not been established. But it is known that frequent drinking increases the risk of chronic pancreatitis and cirrhosis - diseases that, in turn, are risk factors.
- Excess body weight. It has been found that obese people have a 20% increased risk. Excess fat deposits in the abdominal area pose a particularly high risk, even if the person is of normal weight.
- Age over 60–65 years. Almost all patients are over 45 years old. Two thirds are over 65 years of age. Most often, the disease is found in people over 70 years of age.
- Pancreatic cysts and adenomas are considered precancerous diseases.
Heredity as a cause of cancer
Every 50th patient with chronic pancreatitis has a hereditary form of inflammation of the pancreas, with it the likelihood of malignant degeneration of the pancreas increases 50 times, and the disease is diagnosed in four out of ten patients suffering from pancreatitis. If you also smoke with such a genetic background, then a malignant neoplasm will appear at a younger age. And the culprit is a gene that is unable to stop the synthesis of the enzyme trypsin, which is produced in excess and causes the digestion of pancreatic cells, which leads to the formation of neoplasia.
Every 20th patient with pancreatic cancer has a hereditary tumor. When a parent has cancer, the likelihood of his offspring getting sick doubles; when both parents are sick, it increases sixfold; if three first-degree relatives are sick, it increases 30 times. But which genes regulate family transmission have not yet been precisely determined.
In the United States, the incidence of pancreatic cancer in African Americans is half that of whites, which may be related to genes.
Can pancreatic cancer be prevented?
Not all risk factors can be controlled, but some effective prevention measures exist. First of all, you should stop smoking - this will help reduce the risk of several types of cancer. It's never too late to quit; there will be health benefits anyway. Try to maintain a healthy weight and avoid alcohol—some studies suggest there is no safe dose. If at work you have to come into contact with harmful chemicals, follow safety rules and use personal protective equipment.
Symptoms of pancreatic cancer
Often, the first symptoms appear already in the later stages, when the tumor compresses neighboring organs, leads to obstruction (blocking the lumen) of the ducts, and intoxication of the body with decay products.
Get a consultation with an oncologist
Pancreatic cancer pain
The first sign of the disease is usually pain. Its appearance indicates that the tumor has grown into the nerve endings. The intensity of pain varies, from a feeling of discomfort to acute attacks. The localization of pain depends on which part of the organ is affected:
- head - under the right rib,
- tail - in the upper abdomen on the left,
- the entire pancreas - pain of a girdling nature.
The pain intensifies when the patient lies on his back, after eating fatty, spicy foods, or alcoholic drinks. Often these symptoms are mistaken for manifestations of pancreatitis or other diseases, and are attributed to errors in diet and addiction to alcohol. Many people do not go to doctors for a long time, while the tumor progresses.

Thrombosis
Sometimes the first manifestation of pancreatic cancer is deep vein thrombosis of the leg. This condition is manifested by the following symptoms:
- pain,
- edema,
- redness,
- increased temperature of the skin of the leg.
If a piece of a blood clot breaks off, migrates into the vessels of the lungs and blocks their lumen, a complication develops - pulmonary embolism.
Obstructive jaundice
This complication develops when a tumor compresses the bile duct. Symptoms are typical:
- the skin, mucous membranes and sclera of the eyes become icteric;
- urine darkens, looks like dark beer;
- stool becomes colorless;
- the stomach increases due to the enlargement of the liver and gall bladder;
- Itchy skin bothers me.
Jaundice increases slowly. At first the skin has a bright yellow color, then gradually acquires a greenish tint. Over time, kidney and liver failure develops, intense bleeding occurs, and the patient dies.
Intoxication
When a tumor disintegrates, substances are released into the blood that lead to intoxication of the body. The following symptoms occur:
- sudden weight loss;
- decreased appetite, especially in relation to fatty foods and meat;
- weakness, increased fatigue;
- increased body temperature;
- frequent depression;
- lethargy, apathy.
Other manifestations and symptoms
If the tumor grows into the intestine, symptoms of intestinal obstruction occur. Damage to the endocrine islets leads to diabetes mellitus. When the splenic veins are compressed, the spleen increases in size. If the tumor grows into any organ, it may begin to bleed.
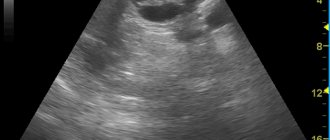
Ultrasound of the pancreas for acute pancreatitis
Acute pancreatitis is a serious disease that can be diagnosed by ultrasound. Acute pancreatitis has a number of stages of development. At each stage, an ultrasound scan of the pancreas visualizes the corresponding picture. Acute pancreatitis can be total, segmental and focal. Accordingly, changes that are detected by ultrasound of the pancreas may concern the entire organ as a whole or its individual parts. Most often, an ultrasound of the pancreas during acute pancreatitis in the first phase of the disease reveals an increase in the size of the gland, blurring of its contours (with the spread of edema to adjacent tissues), and an expansion of the pancreatic duct. Also, during an ultrasound of the pancreas, changes can be detected in other organs associated with compression of them or blood vessels by the enlarged pancreas. For example, compression of the portal vein and its branches, the inferior vena cava, may occur. These changes in the vessels can be monitored using duplex scanning. Also, during an ultrasound of the pancreas in acute pancreatitis, signs of biliary tract obstruction can be detected - an enlargement of the gallbladder and an expansion of the common bile duct.
If the disease enters the necrotic stage, the formation of pseudocysts can be observed on ultrasound of the pancreas. Pseudocysts arise at the site of destruction of pancreatic tissue. Also, in severe cases of acute pancreatitis, the formation of abscesses in the abdominal cavity and omental bursa can be visualized. Ultrasound of the pancreas in chronic pancreatitis makes it possible to detect changes in the contour of the pancreas, heterogeneity of the internal structure, unevenly dilated pancreatic duct and thickening of its walls. Changes can be total, focal or segmental in nature. Sometimes an ultrasound of the pancreas shows calcifications in the pancreatic tissue or in the Wirsung duct (calculi). It is also possible to identify foci of acute inflammation of the pancreas against a changed background - signs of recurrent pancreatitis.

Diagnosis of pancreatic cancer
It is very difficult to detect pancreatic cancer in time, in the early stages. Signs occur when the tumor manages to grow into neighboring organs, metastasize, and the prognosis becomes unfavorable. During the examination, the doctor can feel the enlarged liver, gall bladder, and spleen. In later stages, ascites, an accumulation of fluid in the abdomen, can be detected.
All these signs are nonspecific; they are also found in other diseases.
Usually, if pancreatic cancer is suspected, the examination begins with an ultrasound. This is the simplest, most accessible and inexpensive diagnostic method, and in most cases it helps to detect a tumor.
Endosonography (endoultrasound) is more informative. During this study, a special probe is inserted into the duodenum, at the end of which there is a miniature video camera and an ultrasound sensor. Due to the fact that the sensor is brought as close as possible to the pancreas, it allows you to get a more detailed picture.

Computed tomography and MRI help assess the size and location of the tumor, the spread of cancer to other organs, and determine whether the tumor can be removed surgically.
Cholangiopancreatography is a study that helps evaluate the condition of the pancreatic and bile ducts. It can be done in three different ways:
- Endoscopic retrograde cholangiopancreatography (ERCP) . The doctor inserts a probe into the duodenum, finds the opening through which the bile duct enters, and injects a radiopaque contrast agent through it. Then x-rays are taken: the “painted” ducts become clearly visible in the photographs.
- Percutaneous transhepatic cholangiography is indicated if ERCP fails. A radiopaque substance is injected through a needle.
- Magnetic resonance cholangiopancreatography (MRCP) is essentially a conventional magnetic resonance imaging scan. This is a non-invasive test; no instruments need to be inserted into the patient's body. But during MRCP, unlike ERCP, it is impossible to perform a biopsy or perform therapeutic manipulations.
Biopsy is an examination of a sample of pancreatic tissue under a microscope. This is the most accurate diagnostic method in oncology; it helps to definitively confirm or exclude the presence of cancer cells.
To determine whether radical surgery can be performed, angiography is often necessary. This is an x-ray examination during which blood vessels are “stained” using a contrast solution.
PET scanning helps detect distant metastases in the diagnosis of pancreatic malignancies with metastases.
In a biochemical blood test for pancreatic cancer, increased levels of enzymes (amylase, lipase, etc.), bilirubin, liver transaminases (AlAt, AsAt), and bile acids are detected. In advanced cases, protein levels decrease.
Questions and answers
How long do people live with pancreatic cancer?
After the appearance of distant metastases in pancreatic cancer, most patients live for one to two years. Therefore, it is extremely important to detect the disease in time at stages preceding metastasis, when the chances of successful treatment remain quite high.
What does pancreatic cancer look like?
At the initial stage, the tumor develops asymptomatically. Since the pancreas is a small organ located deep in the abdominal cavity, the presence of a neoplasm cannot be noticed externally. When the liver is damaged, many patients develop a yellowish tint to the skin and whites of the eyes, and people noticeably lose weight due to impaired digestive function and general intoxication.
Is there a cure for pancreatic cancer?
If the tumor is detected early and the operating surgeon is highly qualified, as well as with careful professional care after surgery, the chances of a cure are quite high. Therefore, if symptoms reminiscent of pancreatitis or diabetes appear, it is necessary to undergo a preventive examination by an oncologist. This is especially important for older people who are at risk.
Attention! You can cure this disease for free and receive medical care at JSC "Medicine" (clinic of Academician Roitberg) under the State Guarantees program of Compulsory Medical Insurance (Compulsory Medical Insurance) and High-Tech Medical Care. To find out more, please call +7(495) 775-73-60, or on the VMP page for compulsory medical insurance
Pancreatic cancer: ICD-10 code
In the International Classification of Diseases, Tenth Revision (ICD-10), pancreatic cancer is coded C25 - “malignant neoplasms of the pancreas.” It identifies eight clarifying diagnoses - subheadings:
- C25.0 - tumors of the head of the pancreas;
- C25.1 - malignant tumors of the body of the pancreas;
- C25.2 - tumors of the tail of the pancreas;
- C25.3 - pancreatic duct tumors;
- C25.4 - neoplasms from islet cells;
- C25.7 - tumors of other parts of the organ;
- C25.8 - tumor lesion of several parts listed above;
- C25.9 - unspecified tumor lesion of the pancreas.
Diagnostics
Detection of a pancreatic tumor at the first stage is extremely rare. This is due to the absence of characteristic symptoms. Most often, cancer in the early stages is diagnosed during examination for another disease. At the Yusupov Hospital, research is carried out using modern equipment. It allows you to accurately and quickly determine the type and stage of tumor development. This is important for clarifying further treatment tactics.
Comprehensive diagnosis of pancreatic cancer includes:
- General and biochemical blood test. It is prescribed to identify the inflammatory process in the body. Pay attention to such indicators as ESR, leukocyte formula, ALT, AST, bilirubin, lipase, amylase and alkaline phosphatase;
- Coagulogram. Determined to assess the degree of blood clotting disorder;
- Determination of the level of tumor markers in the blood. CA-242 and CA-19-9 are considered specific tumor antigens for pancreatic cancer. An increase in their concentration indicates a high risk of tumor formation;
- Ultrasound examination (ultrasound) of the abdominal organs. Allows you to evaluate the structure of the pancreas, its size, as well as the location of the pathological focus;
- Computed tomography (CT) and magnetic resonance imaging (MRI). Layer-by-layer examination of the pancreas makes it possible to assess the location, size and degree of tumor invasion into adjacent tissues;
- Positron electron computed tomography (PET-CT). A contrast agent is used for the study. After the labeled isotope accumulates in the pancreas, the organ is examined for the presence of tumor formation;
- Endoscopic retrograde cholangiopancreatography. The head of the pancreas is examined using an endoscope. A contrast agent is injected through it, which stains the organ. A series of x-rays allows you to determine the location and size of the tumor;
- Laparoscopy is a high-tech and informative research method. During the procedure, it is possible to perform a biopsy for histological analysis of the tissue samples obtained from the pathological focus;
- Biopsies. Pancreatic cancer must be confirmed by histological examination. A biopsy can determine the type and stage of cancer. This is necessary to determine treatment tactics.
Diagnosis of pancreatic cancer in the early stages of the disease (before the lumen of the bile ducts closes and penetrates the duodenum) is difficult. Therefore, doctors at the Yusupov Hospital are especially attentive to patients who complain of prolonged pain that occurs without any reason in the left upper quadrant of the abdomen.
Evaluation with barium contrast X-ray is only useful if the tumor is large. An x-ray may show displacement of the stomach cavity and the posterior wall of the abdominal cavity. The tumor can affect the mucous membrane of the duodenum and stomach. When barium suspension is used, the structures have an irregular shape.
The use of ultrasound and computed tomography makes it possible to detect small tumors, including neoplasms of the body and tail of the pancreas. If the results of the study are negative, endoscopic ultrasonography is performed. Using computed tomography, tumor lesions of the pancreas and its penetration into the surrounding area, cancer metastasis to the liver and neighboring lymph nodes are determined. A puncture biopsy allows for histological examination and confirmation of the diagnosis.
Patients with obstructive jaundice undergo transhepatic cholangiography and endoscopic retrograde cholangiopancreatography. Transhepatic penetration reveals the proximal site of obstruction and helps distinguish pancreatic malignancy from cancer of the gallbladder, bile duct, or papilla of Vater. Using endoscopic retrograde cholangiopancreatography, narrowing of the common pancreatic duct and compression of the common bile duct by a neoplasm can be detected.
Endoscopic ultrasound is useful in cases where resection is contemplated. Before surgery, surgeons prescribe angiography to exclude involvement of draining veins in the tumor process. In approximately 60% of cases, cancer occurs in the head of the pancreas. Tumors are usually poorly demarcated.
Closure of the lumen of the pancreatic duct with an upstream dilation, as well as signs of chronic pancreatitis, create a “double-barreled shotgun” symptom when both ducts (pancreatic and common bile ducts) are dilated. These changes are detected by imaging. By the time doctors detect pancreatic cancer, the tumor has usually spread to nearby structures. In most cases, jaundice develops not just as a result of compression of the bile ducts, but as a result of tumor growth.
The diagnosis is confirmed in 75% of cases either cytologically (using fine-needle aspiration biopsy) or histologically (using internal biopsy under ultrasound guidance or computed tomography).
Ductal adenocarcinoma is detected in 80% of patients suffering from pancreatic cancer. They vary in the degree of differentiation, the presence of mucin, and the presence or absence of giant cells or squamous elements. Less commonly, malignant neoplasms have predominantly acinar characteristics or a main mucous (colloid) component. Oncologists at the Yusupov Hospital establish the final diagnosis and stage of the tumor process based on an analysis of the results of the studies.

Pancreatic cancer treatment
Since the disease is most often diagnosed in late stages, its treatment poses a major challenge. They resort to surgical methods, radiation therapy, chemotherapy, and hormonal therapy.

Surgery
Surgical removal of the tumor is possible only in 10–15% of cases. In this case, three conditions must be met:
- pancreatic cancer should not grow into neighboring organs;
- there should be no metastases;
- The patient's health must allow him to undergo major surgery (therefore, surgical treatment is more often performed in young people).
Whipple operation for pancreatic cancer (pancreaticoduodenectomy)
During the operation, part of the pancreas or its entirety is removed, sometimes with part of the duodenum, stomach, common bile duct, and nearby lymph nodes if they are affected by the tumor process. Most often it is necessary to resort to Whipple's operation - pancreaticoduodenectomy.
Euroonco clinics employ experienced surgeons and have well-equipped operating rooms. We carry out operations of any complexity.
In some cases, an anastomosis is surgically established between the gallbladder and the jejunum, which allows direct flow of bile. When the tumor cannot be removed due to deep germination, doctors resort to a number of manipulations to facilitate the removal of bile and improve the patient’s well-being.
Most often, the Whipple procedure is performed openly, through an incision. Some large cancer centers practice laparoscopic interventions through punctures in the abdominal wall. This is a complex operation, it requires appropriate equipment, qualifications and experience of the doctor.
Distal pancreatectomy
If the tumor is in the tail or body of the pancreas, only these can be removed. This operation is called distal pancreatectomy. Most often, the spleen is also removed. Unfortunately, this type of surgical intervention can be performed only in rare cases, because at the time of diagnosis, cancer of the body and tail of the pancreas has already spread greatly beyond the organ and becomes inoperable.
Total pancreatectomy
During this intervention, the pancreas is completely removed, as well as the gallbladder, spleen, part of the stomach and small intestine. Total pancreatectomy is possible in cases where the malignant tumor affects all parts of the organ, but does not extend beyond its boundaries. Such situations are extremely rare.
After radical treatment, the patient must take enzymes and insulin for life.
Pancreatic cancer grows very quickly. If radical treatment is not possible, it is not advisable to remove part of the tumor, especially in older people with concomitant diseases. The risks of major surgery greatly outweigh the potential benefits.

One of the most common and serious complications of pancreatic cancer is obstructive jaundice. In order to restore the flow of bile, they resort to palliative interventions:
- An anastomosis between the jejunum and the gallbladder.
- Placement of a drainage catheter during endoscopic retrograde cholangiopancreatography (ERCP). Periodically, the catheter becomes clogged and needs to be changed every 3–4 months.
- Placement of a stent (a rigid metal frame with a mesh wall that widens the lumen of the duct) during percutaneous transhepatic cholangiography.
Nanoknife in the treatment of pancreatic cancer
If a malignant tumor of the pancreas is inoperable, or the operation carries high risks, a modern technology called nanoknife , or irreversible electroporation . The essence of the procedure is that, under ultrasound or CT guidance, electrodes are placed in or around the malignant tumor and a series of high-voltage electrical pulses are applied to them. As a result, the tumor cells are destroyed and then eliminated from the body naturally.
Scientific research data show that nanoknife is an effective method for the palliative treatment of inoperable malignant tumors of the liver and pancreas. It helps prolong the life of patients by 2 times or more. Moreover, the technique is minimally invasive and does not carry the same risks as classical surgical interventions.
Chemotherapy
Chemotherapy drugs for pancreatic cancer have little effect. Most often they are prescribed in combination with radiation therapy, especially for inoperable tumors, to prolong life and improve the patient's well-being.
Hormone therapy shows good results, since tumor cells in the pancreas often contain estrogen receptors, which stimulate their growth. In some cases, hormonal drugs help prolong the patient's life.
Radiation therapy for pancreatic cancer
Radiation therapy is most often given after surgery to kill any remaining cancer cells in the body. Sometimes preoperative (neoadjuvant) radiation therapy is given to make tumor removal easier. For inoperable cancer, radiation therapy can be the main treatment method; it helps relieve the patient of pain.
Treatment of malignant pancreatic tumors with liver metastases
For metastatic lesions, in addition to systemic chemotherapy, intra-arterial chemotherapy can be used. The antitumor drug solution is injected directly into the artery feeding the malignant tumor. This allows you to use high doses without fear of serious side effects, since the chemotherapy drug practically does not enter the systemic circulation.
Another specific treatment for pancreatic cancer with liver metastases is radiofrequency ablation (RFA). It can be used if there are no more than 5 tumor foci, the size of each of them is no more than 4 cm, and they are clearly visible during ultrasound and computed tomography. A needle-electrode is inserted into the lesion and destroyed using high-frequency current.
Pancreatic cancer that has metastasized to the liver tissue can lead to ascites , a condition in which fluid accumulates in the abdominal cavity. Because of this, the functioning of internal organs is disrupted and the patient’s condition worsens. Ascites is an indication for laparocentesis - removal of fluid from the abdominal cavity through a puncture. For its constant outflow, peritoneal catheters .
Suspicious but not proven risk factors
A diet rich in animal proteins and poor in plant components has long been suspected as the cause of the pathology, but clinical studies have not yielded convincing evidence. It is believed that the effect of meat is aggravated by coffee, but no scientific basis has been found for this hypothesis.
However, immigrants who come from regions with low incidence and live long enough in a country with high incidence have a comparable risk of getting sick to the local population. And the reason is the inevitable change in diet.

A connection between the pathology and obesity is assumed, but this is also an unconvincing hypothesis.
Infectious diseases have also contributed to the causes of pancreatic neoplasms, similar to the fundamental role of the hepatitis virus in the initiation of liver cancer. But the role of Helicobacter pylori infection has not yet been proven for the development of pancreatic tumors.
There is an assumption that the removal of the stomach or gallbladder does not leave a permanent mark on the pancreas.
Diagnosis of pancreatic cancer should confirm or reject the malignant nature of the disease, determine its prevalence and exact localization in the gland. In case of an unconditionally resectable tumor, verification - morphological confirmation of cancer can be carried out during surgery.
Review of the treatment of obstructive jaundice
The patient was admitted with severe signs of jaundice. During hospitalization, his condition stabilized. For this purpose, drainage of the bile ducts was carried out, as well as exposure to medications. After receiving the results of the histochemical study, further treatment tactics will be determined. Read full review
“They have golden hands”...
The patients are being treated at the international clinic Medica24. During the treatment, they managed to become friends and this time decided to record a joint review. They thank all the clinic staff for the high organization of all processes and the effectiveness of the procedures. Read full review
Chemotherapy - review by Olga Stepanovna
The patient is hospitalized for the third time. During a comprehensive examination, a puncture of the tumor was performed. Histological analysis made it possible to verify the diagnosis and determine treatment tactics. At the first stage of treatment, surgery was performed. The tumor was radically removed. Drug treatment is now being carried out to prevent the possibility of relapses. To date, the first course of chemotherapy has been completed. The patient was discharged home in satisfactory condition. Read full review
“You are the only clinical organization that brings benefits to people”...
The patient was admitted for treatment of cancer. The hospitalization lasted a week. The patient notes that they immediately responded to all his problems and provided assistance in a timely manner. He compares the international clinic Medica24 with other medical institutions. Patient about... Read full review
Review of the attending physician M.Kh. Mustafaeva
The patient was hospitalized in serious condition. Complex treatment was carried out. A positive effect has been achieved. The patient’s wife thanks her husband’s attending physician Milana Khanlarovna Mustafaeva. She says: “From the first day, from the first minute, as soon as we came to you, we immediately felt and understood each other. You understood the patient, you understood me. You have defined to the depth of the volume that we need. Although I couldn’t explain how... Read full review
Feedback on the treatment of breast disease
The patient was hospitalized with breast disease. By decision of the council, surgery was performed at the first stage of treatment. It was successful. On the third day the patient was discharged home. After histological examination, further treatment tactics will be determined. Read full review
Feedback on the treatment of ascites
The patient contacted the Medica24 international clinic for treatment of ascites and pleurisy. These conditions are characterized by abnormal accumulation of fluid in the abdominal and pleural cavities, respectively. This happens with cancer. A laparocentesis procedure was performed, during which the fluid was evacuated. The patient's condition improved markedly. Read full review
Nutrition for pancreatic cancer
Many people with pancreatic cancer have poor eating habits. Because of this, they lose a lot of weight, constantly experience weakness, develop anemia and other complications. Therefore, it is always important to assess the nutritional status of such patients and carry out its correction. Nutrition should be as complete as possible, taking into account the physiological capabilities of the patient.
Many patients must regularly take pancreatic enzymes in tablet form. If a person cannot eat properly on his own, he is fed through a nasogastric tube - a thin catheter inserted through the nose into the stomach.
Ultrasound of the pancreas for nonspecific non-tumor lesions
Many pathological conditions in the body can lead to changes in the structure of the pancreas. Almost all of these changes occur through the occurrence of acute or chronic pancreatitis. Injuries to the pancreas, peptic ulcer of the stomach and duodenum, intoxication, diabetes mellitus, amyloidosis, lipomatosis of the pancreas - lead to its changes. These changes are nonspecific and the cause of the disease cannot be determined from them. Rather, we can say this: the changes observed during ultrasound of the pancreas provide additional information about the underlying disease.
Prevention of pancreatic tumors
As with other cancers, there are no reliable measures that can guarantee the prevention of pancreatic cancer. However, there are some ways to reduce the risks:
- Stop smoking . This is one of the most significant risk factors.
- Maintain a normal weight . The two main measures are a healthy diet and regular physical activity.
- Limit your alcohol intake . Although the connection of this factor with the risk of developing pancreatic cancer has been poorly studied, doctors recommend refraining from frequent and excessive drinking of alcohol.
- Follow occupational hygiene rules and use protective equipment . This recommendation applies to people who work in manufacturing and deal with hazardous chemicals.
Conservative treatment
In the treatment of this malignant pathology, the administration of traditional cytostatic drugs is widely used. In addition, oncology today offers more effective means for the treatment of pancreatic cancer. This is, first of all, targeted therapy, in which the active substances of drugs act on specific target molecules of tumor cells, disrupting the processes of their growth and reproduction. Targeted treatment is highly selective, practically without affecting healthy tissue, and therefore produces much fewer side effects. In addition, radiation therapy also demonstrates some effectiveness for pancreatic tumors.
Before surgery, conservative therapy can be prescribed in order to slow down the growth of the tumor as much as possible and reduce its size, destroying as many malignant cells as possible. After surgery, the main point of using these methods is to combat possible metastases and relapses. And in the later stages of the development of the oncological process, when radical operations seem inappropriate, conservative therapy becomes the basis of treatment.
Pancreatic cancer: life expectancy
Pancreatic cancer has relatively low five-year survival rates. In the early stages they are 5-14%, in the later stages - 1-3%.
Even if cancer is diagnosed late and the prognosis is clearly unfavorable, this does not mean that nothing can be done to help the patient. Euroonco doctors know how to relieve pain and other painful symptoms, prolong life, and ensure a decent quality of life. We undertake the treatment of pancreatic cancer at any stage.
Symptoms

The initial symptoms of pancreatic cancer are nonspecific and can easily be attributed to poor health, but they should never be neglected. In the early stages the disease manifests itself:
- discomfort in the upper abdomen;
- extreme thirst, frequent urination and other signs of diabetes;
- weakening of stools up to liquefaction, frequent urge to defecate;
- fatigue, decreased performance, loss of appetite.
As the tumor grows and the disease progresses, more serious symptoms develop:
- pain in the upper abdomen, often radiating to the back;
- yellowing of the sclera of the eyes and skin due to disturbances in the outflow of bile;
- nausea, periodic vomiting;
- digestive disorders due to decreased production of digestive enzymes;
- body weight loss.
Prices for treatment of pancreatic cancer
- Consultation with an oncologist— RUB 5,100.
- Consultation with a chemotherapist— RUB 6,900.
- Gastropancreaticoduodenal resection - RUB 318,100.
- Distal resection of the pancreas - 168,800 rubles.
- Pancreaticoenteroanastomosis - RUB 114,900.
- Total pancreatectomy - RUB 284,600.
- Carrying out intrapleural chemotherapy (infusion, without the cost of drugs) - 19,100 rubles.
- Immunotherapy (without the cost of medications) - RUB 15,000.
Make an appointment with an oncologist
Book a consultation 24 hours a day
+7+7+78