If a gynecologist has diagnosed you with an ovarian cyst, do not be alarmed: as a rule, these formations are benign and do not pose a danger; surgery is not required. Often they do not need to be treated at all and disappear on their own within a few months. It is enough to periodically visit a gynecologist and undergo an ultrasound examination.
- What types of ovarian cysts are there?
- When is laparoscopy performed?
- When is laparoscopy not performed?
- Benefits of laparoscopy
- Preparation
- How is laparoscopy performed?
- Postoperative period
- Complications
- Is it possible to get pregnant after removing an ovarian cyst?
Sometimes ovarian cysts still have to be removed. Operations can be performed without an incision, through several punctures in the abdominal wall - laparoscopically. Euroonco employs expert-level gynecological surgeons who have extensive experience in performing such interventions. Come for a consultation with our specialist: he will tell you whether surgery is necessary in your case, and prescribe an examination that will help distinguish a benign neoplasm from a malignant one.
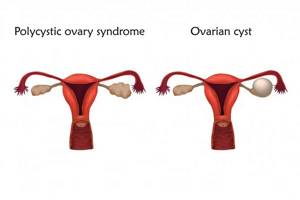
A cyst is not a specific disease. This term refers to any pathological cavity with fluid. The reasons for its formation are different. According to statistics, ovarian cysts are diagnosed in every tenth woman. They most often occur during puberty and menopause. Some girls have them from birth.
What types of ovarian cysts are there?
All ovarian cysts are divided into two large groups: functional , which occur in most cases, and pathological , which doctors have to deal with much less frequently.
Functional cysts are the result of disturbances during the menstrual cycle. Usually they do not cause complications and disappear on their own. They come in three types:
- Follicular . follicle matures in a woman’s ovaries . Normally, it should open and release the oocyte. If this does not happen and the follicle continues to grow, it turns into a cyst.
- Corpus luteum cysts . After the follicle releases the egg, it turns into a special gland - the corpus luteum . It produces the hormones estrogen and progesterone. If pregnancy does not occur, the corpus luteum atrophies. And if fluid accumulates in it, it turns into a cyst.
- Theca-luteal cysts often develop as a side effect of infertility treatment with hormonal drugs.
Pathological ovarian cysts are not associated with the menstrual cycle. They are always characterized by the appearance of “wrong” cells that should not be present normally. The most common types of pathological cysts:
- Endometrioid . This is a form of endometriosis, a condition in which endometrial tissue (the lining of the uterus) gets into unusual places and grows there. In the ovaries, it can form cavities with fluid. They often appear as “chocolate” cysts filled with dark blood.
- Dermoid cysts , or teratomas , are a special type of benign tumors made from embryonic cells. There may be different tissues inside them, for example, skin, hair, nails. Dermoid cysts become malignant very rarely.
- Cystadenomas are benign neoplasms of epithelial cells. Usually they are filled with contents of a mucous or watery nature.
For more information about malignant cysts, please visit the ovarian cancer page on our website.
When is laparoscopy performed?
If the ovarian cyst is small, does not cause symptoms and does not look cancerous, it can be left alone. No surgery needed. The gynecologist will prescribe periodic examinations and control ultrasounds. Moreover, postmenopausal women will have to do this more often, because they have a higher risk of malignant tumors.
Are there effective medications?
In some cases, hormonal contraceptives may be helpful. They help prevent the formation of new cysts in the ovaries, but do not affect the growth of existing ones. If a woman is bothered by pain, the doctor may prescribe drugs from the group of nonsteroidal anti-inflammatory drugs (NSAIDs). But this is only symptomatic treatment. The only way to get rid of the formation is surgery.
If the cyst is “problematic,” then the doctor will definitely say that it needs to be removed. Indications for surgery:
- Large size of formation. In most cases, ovarian cysts have a diameter of 1–3 cm. Very rarely they reach 15–30 cm.
- Presence of symptoms: abdominal pain, pelvic pain, bloating, feeling of heaviness in the abdomen, heavy periods, vaginal bleeding not associated with the menstrual cycle. A large cyst can compress the intestines and bladder. This leads to problems with stool and urination.
- Suspicion of a malignant nature of the cyst - the risks are increased in postmenopausal women.
- Continued growth over 2–3 menstrual cycles.
- Pathological ovarian cyst.
What happens if the cyst is not removed?
If the doctor said that the cyst needs to be removed, then delaying the operation is primarily dangerous for postmenopausal women. They, as we have already mentioned, have a higher risk that the formation may turn out to be malignant. And with cancer, time is critical. The later treatment is started, the lower the chances that it will be successful and that remission will be achieved. The prognosis worsens and survival rate decreases.
At the Euroonko clinic you can receive treatment for ovarian cancer according to modern standards. Our doctors perform operations of any complexity; we have access to all the latest generation antitumor drugs registered in Russia. We work according to modern European, American, Israeli treatment protocols. For ovarian cancer complicated by peritoneal carcinomatosis, we use an innovative technique - hyperthermic intraperitoneal chemotherapy (HIPEC).
With benign ovarian cysts, serious complications can also occur, although they are rare. Large cysts may rupture. In this case, severe bleeding develops into the abdominal cavity, and severe abdominal pain occurs.
As the cyst grows, the risk of ovarian torsion increases. Due to compression of the blood vessels, it stops receiving blood supply, severe abdominal pain, nausea, and vomiting occur. The result may be necrosis (death) of the ovary, and it will have to be removed urgently.
If you experience symptoms such as severe abdominal pain, nausea, vomiting, or a fever of more than 38 degrees, you should immediately seek medical help.
Indications for removal.
Most often, functional cysts do not require surgical removal. They do not tend to become malignant, which means they do not carry cancer risks. Functional cysts go away on their own, or patients are prescribed hormonal therapy with oral contraceptives, which stop the cycle, and the neoplasms associated with it are reduced. However, if conservative therapy is unsuccessful and is not suitable for any reason, surgical removal of the cyst is performed.
Surgical treatment is indicated when any ovarian tumor is detected during menopause, conservative therapy is ineffective for more than 3 months, in the case of functional cysts and if there is a risk of malignancy. The development of any of the complications (suppuration, hemorrhage, rupture, torsion of the leg) is an indication for emergency surgery.
The extent of resection and the choice of access are determined individually together with the patient before surgery. Also, before the intervention, it is necessary to discuss the resection options that may be available if a malignant tumor is detected.
Currently, most elective operations are performed using laparoscopic access, which reduces tissue trauma, severity of pain and rehabilitation time.
Preparation
Ovarian cysts are usually detected during an ultrasound examination. In order to better assess the size, location and internal structure of the neoplasm, the condition of the ovary, they usually resort to not only transabdominal (through the abdominal wall), but also transvaginal (using a special sensor inserted into the vagina) ultrasound.
In rare cases, usually when a malignant nature of the formation is suspected, computed tomography and diagnostic laparoscopy are prescribed. of cancer antigen 125 (CA 125) in the blood testifies in favor of cancer . But this analysis is unreliable, since a positive result can be obtained for uterine fibroids, endometriosis and inflammatory processes in the pelvic organs.
Based on the examination results, the doctor advises the woman and explains which treatment tactics will be optimal in her case. If laparoscopic surgery is indicated, a date for hospitalization is set. You need to undergo a preoperative examination. It usually includes the following diagnostic methods:
- General and biochemical blood tests.
- General urine analysis.
- Blood test for hormone levels.
- Tests for infections.
- Cervical smears - cytological, flora.
- Blood clotting study.
- Determination of blood group AB0, Rh factor.
- Electrocardiography.
- X-ray of the lungs.
Laparoscopic removal of ovarian cysts is performed under general anesthesia - endotracheal anesthesia. The woman is hospitalized in the hospital the day before surgery. You can’t eat anything for 8 hours before surgery, and you can’t drink anything in the morning. Some time before anesthesia, premedication : the woman is given drugs that help her relax and calm down.
How is laparoscopy performed?
Laparoscopic intervention is performed through several punctures in the abdominal wall. Through one of them, in the navel area, a laparoscope - an instrument with a miniature video camera. It broadcasts an enlarged image onto the screen. For better visualization during surgery, the abdominal cavity is filled with gas.
Special laparoscopic instruments are inserted through additional punctures, and the cyst is removed with the help of them.
Depending on the specific situation, the scope of the operation varies:
- Often it is possible to remove only the cyst, preserving the ovary.
- In some cases, it is necessary to remove the entire ovary - to perform an oophorectomy (oophorectomy) - while the second ovary can be saved. This has to be done if a malignant tumor is suspected, or if the cyst is in an “inconvenient” location, when it is difficult to remove it separately.
- In rare cases, both ovaries may have to be removed. This operation is performed only in extreme cases, especially in women of reproductive age, since menopause occurs after removal of both sex glands. The levels of female sex hormones decrease, and this can lead to symptoms such as headaches, dizziness, nausea, hot flashes, etc.
Don't hesitate to ask your doctor questions before surgery. Ask what is the likelihood that during the operation you will have to remove both ovaries, what negative consequences this threatens, and how to cope with them.
2. How to prepare and how is the procedure performed?
How to prepare for laparoscopy?
Tell your doctor if you have:
- allergies to medications, including anesthesia.
- bleeding problems or if you are taking any blood thinners (such as aspirin or warfarin (Coumadin).
- pregnancy.
Before laparoscopy:
- Follow the instructions exactly about when to stop eating and drinking, or your surgery may be cancelled. If your doctor has recommended that you take medications on the day of surgery, please take them with only a sip of water.
- Leave your decorations at home. Any jewelry you wear should be removed before your laparoscopy.
- Remove your glasses, contact lenses, and dentures before laparoscopy. They will be returned to you as soon as you recover from the operation.
- Arrange to be driven home after your laparoscopy.
- You may be asked to use an enema or suppository several hours before or on the day of surgery to cleanse your colon.
- Most importantly, discuss with your doctor all the questions that concern you before the procedure. This will reduce risks and will be an important point in the success of the operation.
How is laparoscopy performed?
Laparoscopy is performed by a surgeon or gynecologist. General anesthesia is usually used
, but other types of anesthesia (for example, spinal) can also be used. Discuss with your doctor which method is right for you.
You will need to empty your bladder about an hour before surgery, as you will subsequently receive large amounts of fluid and medications intravenously. You will also be given sedatives to help you relax.
During laparoscopy, several of these procedures may be done after you have received anesthesia, are relaxed or asleep:
- A breathing tube is placed down your throat to help you breathe if general anesthesia is used.
- A thin, flexible tube (urinary catheter) may be inserted through the urethra and into the bladder.
- Some pubic hair may be shaved off.
- Your stomach and pelvic area will be treated with a special cleansing composition.
- For women: Your doctor may do a pelvic exam before inserting thin tubes (cannulas) through the vagina into the uterus. The cannula allows the doctor to move the uterus and ovaries to better view the abdominal organs.
During laparoscopy, a small incision is made in the abdomen. If other means are used during surgery, additional incisions may be made. A hollow needle is then inserted through the incision and a gas (carbon dioxide or nitrous oxide) is slowly injected to inflate the abdomen. The gas lifts the abdominal walls so that the doctor can clearly see the internal organs.
A thin, lighted tube is inserted through the incision to view organs. Other instruments may be used to take tissue samples, repair damage, or remove a cyst. A laser attached to a laparoscope may be used to assist in the operation. After the operation, all instruments will be removed and the gas will be released. The incisions will be closed with small stitches and covered with a bandage. The laparoscopy scar will be very small and will disappear over time.
Laparoscopy takes from 30 to 90 minutes, depending on the complexity of the operation, but may take longer (for example, with endometriosis). After laparoscopy, you will be placed in a recovery room for 2-4 hours. Usually the next day you will be able to resume your normal activities without heavy loads. Full recovery takes about a week.
Visit our Microsurgery page
Complications
Laparoscopic operations are associated with a low risk of complications. As after any surgical intervention, in rare cases, infection and suppuration in the area of surgical sutures and bleeding are possible. If you are concerned about severe pain, vaginal bleeding, or increased body temperature, you should immediately consult a doctor.
Adhesions may occur after surgery. Very rarely, during surgery, damage to neighboring organs (intestines, bladder) is possible.
At the Euroonko clinic, operations are performed by experienced gynecological surgeons. Our operating room is equipped with modern equipment, multifunctional laparoscopic stands from leading manufacturers. This helps to minimize risks and perform the operation as safely as possible.
After removal, the cyst may recur, in the same ovary or on the other side. Only removal of both ovaries helps to completely eliminate relapse. But such an operation leads to menopause and undesirable consequences, so it is resorted to only in extreme cases.
Is it possible to get pregnant after removing an ovarian cyst?
You can get pregnant even with an ovarian cyst. Most often, they do not interfere with pregnancy, but they can make it difficult to conceive a child.
If during surgery only the cyst is removed or at least one ovary is left, the woman’s fertility is preserved. She may become pregnant in the future. Of course, you need to understand that reproductive function is affected not only by surgery. The ovarian reserve (the number of eggs in the ovaries - it constantly decreases with age) and concomitant diseases play a role.
Get a consultation with a doctor at the Euroonko clinic. Our doctor will tell you whether treatment is needed in your case, what type of surgery is indicated for you, and what is the likelihood that you will be able to conceive and carry a pregnancy in the future.
Book a consultation 24 hours a day
+7+7+78
3.Feelings during laparoscopy
With general anesthesia, you will sleep and not feel anything. After your laparoscopy and when you wake up, you will feel sleepy for several hours. You may experience fatigue and some pain for a few days after laparoscopy. You may have a slight sore throat from the breathing tube. Use lozenges and gargle with warm salt water.
With other types of anesthesia, slight pain may occur for several days.
About our clinic Chistye Prudy metro station Medintercom page!









