- Why do cancer patients experience pleurisy?
- What symptoms occur with pleurisy?
- How is pleurisy diagnosed?
- Treatment of pleurisy in malignant tumors
- Chemotherapy for exudative pleurisy
- What is pleurodesis?
- Immunopreparations for pleurodesis
- Efficiency of treatment in cancer patients with exudative pleurisy
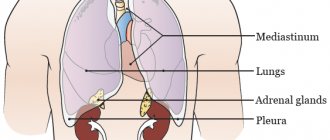
Pleurisy is an inflammation of the pleura, a thin membrane of connective tissue that covers the lungs (visceral pleura) and the inner surface of the chest wall (parietal pleura).
The narrow gap between the parietal and visceral layers of the pleura is called the pleural cavity. Normally, it contains a small amount (10 ml) of liquid - it acts as a lubricant, reducing friction during lung movements during breathing.
There are two types of pleurisy:
- Exudative pleurisy is accompanied by the accumulation of fluid in the pleural cavity (this condition is called hydrothorax).
- With dry pleurisy, fibrinous deposits form on the pleura and it thickens.
In cancer, the most common form is the first form - exudative pleurisy.
Why do cancer patients experience pleurisy?
There are many reasons why inflammation occurs in the pleura. For example, pleurisy can become a complication of pneumonia, heart failure, liver cirrhosis and other diseases.
The main cause of pleurisy in cancer is metastasis of cancer cells into the pleura and lymph nodes, which are located in the chest. As a result, the outflow of lymph is disrupted and the permeability of the capillary walls increases. Fluid leaks into the pleural cavity.
Most often, pleurisy occurs with cancer of the lung, breast, and ovaries. Less commonly, the cause is malignant tumors of the stomach, colon, pancreas, pleural mesothelioma, and melanoma.
Causes of pleural effusion
| Transudate | Exudate |
| Congestive heart failure Nephrotic syndrome Liver cirrhosis Pericardial diseases Myxedema | Tuberculosis Viral infections Fungal infections Rheumatoid arthritis Parasitic infections SLE Meigs syndrome Chylothorax Hemothorax Pleural mesothelioma Dressler's syndrome Metastatic lesions of the pleura Actinomycosis |
In most cases, pleurisy is a complication of an underlying disease, for example, congestive heart failure, nephrotic syndrome, liver cirrhosis, sarcoidosis, tuberculosis, viral, fungal infections, rheumatoid arthritis and many other various nosologies. The most important aspect of differential diagnosis is the division of pleural effusion into exudate or transudate, taking into account the concentration of protein, LDH and cellular components.
The Light criteria are considered generally accepted in the diagnosis of exudative pleurisy: 1) The ratio of protein in pleural effusion to protein in blood plasma is >0.5. 2) The ratio of LDH in pleural effusion to plasma LDH is >0.6. 3) LDH in the pleural effusion >2/3 of the upper limit of normal for plasma LDH.
What symptoms occur with pleurisy?
The fluid that accumulates in the pleural cavity compresses the lung and prevents it from expanding. The greater the volume of fluid, the more severe the symptoms of pleurisy:
- Weakness, poor health.
- Inability to take a deep breath, feeling that the lungs are not fully expanding.
- A dry (sometimes with a small amount of sputum) cough that occurs due to irritation of nerve receptors in the pleura.
Subsequently, shortness of breath becomes more and more noticeable, and heaviness occurs in half of the chest. The patient tries to lie on the sore side (if the pleurisy is unilateral), this allows the healthy lung to expand better.
The patient's skin becomes pale. If there is a lot of fluid in the pleural cavity, the outflow of blood from the neck veins is disrupted, they swell, this becomes noticeable upon external examination. The diseased half of the chest “lags behind” during breathing, its movements are limited.
These symptoms can also be caused by other diseases. The causes of pleurisy are also different. For an accurate diagnosis, consult a doctor.
Treatment:
A pulmonologist selects an individual treatment program based on the results of laboratory tests, diagnosis and severity of the disease. The doctor may prescribe antibiotics, may suggest some non-steroidal anti-inflammatory drugs, painkillers, and cough suppressants. Among other things, reclining on the sore side with a soft pillow under your head will help you feel better. Immunosuppressive and immunomodulatory therapy is recommended. To relieve pain from dry pleurisy, bandaging the chest with elastic bandages is used. If there is a significant accumulation of fluid in the pleural cavity, diuretics are prescribed. In severe cases of pleurisy, intravenous infusion therapy is performed. Physiotherapeutic procedures can include warming compresses and chest massage, electrophoresis and ultraphonophoresis, paraffin therapy, infrared irradiation and aerotherapy. If effusion is observed, drainage of the pleural cavity may be necessary, which involves installing a tube that drains the fluid. As well as anti-inflammatory, antiviral drugs, vitamin therapy, diet.
How is pleurisy diagnosed?
When you see your doctor, you will need to talk about your symptoms, how and when they began, and how they have changed over time. The doctor will ask you to list the diseases that you have suffered during your life, especially recently. An inspection will then be carried out. The doctor will examine and feel your chest and listen to your lungs and heart using a phonendoscope.
X-rays will help identify pleurisy, assess the amount of fluid in the chest, and sometimes detect tumor metastases in the pleura and lymph nodes.
Computed tomography helps to more accurately identify the cause, extent of tumor pleurisy and the specific changes that caused it. In some cases, the doctor may prescribe an ultrasound.
The mandatory diagnostic method is diagnostic pleural puncture. It is performed if there is not much fluid in the pleural cavity and there is no life-threatening condition. The doctor inserts a needle into the chest, removes some fluid and sends it to the laboratory for testing.
If there is a lot of fluid in the pleural cavity and there is a life-threatening condition, the patient needs urgent help. A thoracentesis is performed, a procedure during which as much fluid as possible is removed from the chest. Part of it is sent for analysis.
If after the examination the diagnosis remains unclear, the oncologist and anesthesiologist-resuscitator may decide to perform video thoracoscopy. A special instrument with a video camera - a thoracoscope - is inserted into the chest and the chest is examined from the inside. During videothoracoscopy, a biopsy can be performed - a fragment of a tumor or suspicious area can be obtained and sent to the laboratory for examination under a microscope. Usually after this it is possible to establish an accurate diagnosis.
Diagnosis of pleurisy
If there is sufficient accumulation of pleural fluid, an experienced oncologist will suspect a problem even when talking with the patient, noticing cyanosis - blue discoloration of the skin of the nasolabial triangle against the background of pallor of the face and “shortness of breath” of the patient’s speech. Listening with a stethoscope and tapping the chest wall will allow you to determine the location, including bilateral pleurisy and the approximate volume of fluid.
X-ray reveals a little more than a glass of exudate, and CT or MRI makes it possible to assess the condition of the pleural layers and lung tissue and determine the size of metastases.
Treatment of the disease, especially with punctures, will require repeated and frequent monitoring of the condition of the pleural cavity using x-ray or, which is harmless, ultrasound (ultrasound). When collecting fluid, ultrasound of the chest cavity allows you to identify a point for optimal puncture.
In case of primary effusion, when the cause is not clear, the exudate obtained during puncture is necessarily subjected to microscopy for verification - confirmation of its malignant nature.
Treatment of pleurisy in malignant tumors
First of all, with sufficiently pronounced exudative pleurisy, it is necessary to perform thoracentesis - evacuation of fluid from the pleural cavity. Typically, this helps reduce shortness of breath, pain, and improve the patient’s well-being and quality of life.
Thoracentesis is performed using a kit that includes:
- special syringe with connector,
- sterile bag for collecting liquid,
- closed system that does not allow air to pass through,
- connecting tube.
During the procedure, the doctor injects an anesthetic solution into the intercostal space at the level where the fluid is located, then inserts a needle into the pleural cavity and removes the fluid. At the end of the procedure, a catheter is left in the pleural cavity connected to a bag, into which the fluid gradually flows.
You can learn more about the procedure from a separate article about thoracentesis on our website.
At Euroonko, unlike many other clinics, thoracentesis is performed using a modern Pleurocan device (USA) and exclusively under ultrasound control, which makes the intervention as fast, effective and safe as possible.
Doctors at our clinic perform thoracentesis on dozens of patients every month. We perform cytological examination of exudate, administer drugs intrapleurally, and provide comprehensive treatment for cancer of almost any type, location, stage.
Chemotherapy for exudative pleurisy
Thoracentesis for exudative pleurisy in a cancer patient is a symptomatic treatment. The procedure helps relieve compression of the lung and improve the patient's condition, but does not eliminate the cause of the disease. After the laboratory has studied the cancer cells that are in the removed exudate, the oncologist will decide on further tactics.
If tumor cells are sensitive to chemotherapy, systemic chemotherapy is prescribed. According to statistics, systemic chemotherapy in combination with other treatment methods helps eliminate pleurisy in approximately 60% of patients sensitive to chemotherapy.
Classification of pleurisy
- Based on the reason that caused the formation of exudate, they are divided into inflammatory (infectious), aseptic, traumatic, malignant (tumor or metastatic).
- According to the localization of the effusion: encysted (limited) and diffuse.
- According to the nature of the resulting fluid: serous, hemorrhagic, purulent, chylous, mixed.
- By fluid volume: basal (supradiaphragmatic), subtotal, total.
Only the gradation due to the formation of effusion always remains unchanged, all other characteristics may change: basal effusion grows to total and vice versa with effective treatment; serous becomes hemorrhagic over time; diffuse is gradually absorbed and encysted.
We will call you back, leave your phone number
Message sent!
expect a call, we will contact you shortly
What is pleurodesis?
If, after a cytological examination of the fluid from the pleural cavity, it turns out that the tumor cells are insensitive to chemotherapy, and if all types of systemic treatment have been exhausted, they resort to pleurodesis - a procedure during which the layers of the pleura stick together and fluid stops accumulating between them.
There are different types of pleurodesis (mechanical, chemical, physical); for exudative pleurisy in cancer patients, chemical is used. A drug is injected into the pleural cavity, which glues the layers of the pleura.
For chemical pleurodesis, different groups of drugs are used:
- Nonspecific sclerosing drugs: antibiotics-tetracyclines, talc. Currently, these drugs are rarely used, as they are poorly tolerated and severe pain occurs after their administration.
- Cytostatics: bleomycin, doxorubicin, cisplatin, etoposide, 5-fluorouracil, etc. These drugs belong to the group of chemotherapy drugs; they are capable of destroying tumor cells, but with exudative pleurisy, their ability to glue the layers of the pleura comes to the fore.
- Drugs for immunotherapy. At the same time, they provide pleurodesis and destroy cancer cells that are in the pleura. Pleurodesis with immunodrugs for exudative pleurisy in cancer patients is the most progressive technique. According to some data, its effectiveness reaches 90–94% (for other methods it is rarely higher than 60%). Immunotherapy is effective for tumors that are resistant to chemotherapy and after intrapleural chemotherapy. The main and most common side effect of this type of therapy is fever and flu-like symptoms, which can be easily managed with nonsteroidal anti-inflammatory drugs (NSAIDs).

Immunopreparations for pleurodesis
Before administering immunotherapy, it is necessary, if possible, to remove all fluid from the pleural cavity, otherwise immunotherapy may be ineffective. The average course of treatment is 14 days (5 days of therapy, then a 2-day break - the cycle is repeated twice).
Drugs that are used for immunotherapy of exudative pleurisy:
- Recombinant interleukin-2. The drug is administered at a dosage of 1 million IU daily for 14 days (ten working days). The method is effective in approximately 90% of patients.
- LAK cells. 50–100 million cells are injected daily, usually for five days. The course of therapy lasts 7 days.
- Recombinant interleukin-2 and LAK cells. Consistently carry out 5 intrapleural injections of recombinant interleukin-2 at a dosage of 1 million IU daily, then 5 injections of LAK at 50–100 million cells daily. On average, the course of treatment lasts 14 days.
During the course of treatment, the patient is constantly under the supervision of medical staff and receives supportive therapy. After completing the course, the patient is examined, then a break of 3–4 weeks is indicated, then a follow-up examination.
Efficiency of treatment in cancer patients with exudative pleurisy
Typically, an oncologist sends fluid obtained from the pleural cavity for cytological examination 3 times:
- Before starting treatment.
- During the course - usually in the middle.
- After completion of treatment.
In the laboratory, the exudate is studied under a microscope: the presence of tumor cells, their number and structural features are determined. In order to assess the effectiveness of treatment for cancer and exudative pleurisy, the doctor focuses on four main indicators:
- General condition of the patient, changes in complaints.
- Survey data.
- The rate of increase in fluid volume in the pleural cavity.
- Changes in the cellular composition of the fluid. Successful treatment is indicated by a decrease in the number of tumor cells and a predominance of lymphoid cells.
The diagnosis and treatment of exudative pleurisy in oncological diseases should be carried out by a doctor who specializes in this pathology, in a specialized hospital where there is the necessary equipment and drugs. Euroonco has everything you need.
Book a consultation 24 hours a day
+7+7+78