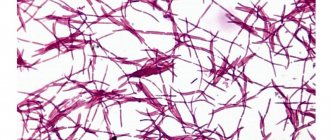
The detection of coccobacillary flora in a smear indicates disorders in the female body.
Cost of services in our clinic
| Appointment with a gynecologist with the highest category | 1000 rub. |
| Consultative appointment with a doctor based on test results and ultrasound results | 500 rub. |
| Extended colposcopy | 1500 rub. |
| Amino test for bacterial vaginosis | 300 rub. |
| Medical abortion (all inclusive) | 4500 |
| Make an appointment by phone: 8-800-707-15-60 (toll-free) |
| *The clinic is licensed to remove tumors |
Normally, the microflora of the female vagina is inhabited by bifidobacteria, peptostreptococci and lactobacilli, each of which has the function of protecting against harmful microorganisms that are causative agents of various diseases. The development of coccobacillary flora can begin as a result of disruptions in the body and exposure to external factors.
Normal vaginal microflora
The vaginal flora is represented by a combination of beneficial and transient microorganisms that are in strict balance: under normal conditions, the beneficial flora significantly exceeds the opportunistic flora.
Approximately 95-98% of all vaginal flora is represented by lactobacilli (Dederlein's rods).
It is lactobacilli (Lactobacillus), which destroy glycogen and produce lactic acid, which provides an acidic environment in the vagina and protects it from infection. The remaining 2-5% of the flora are represented by gram-positive rods, gram-negative cocci, gram-positive cocci, gram-negative obligate anaerobic rods and enterobacteria.

How to restore vaginal microflora after taking antibiotics
All these representatives of the vaginal flora are in symbiosis with the human body, not causing harm to health, but, on the contrary, protecting it from disease. With the normal functioning of the microflora, the infection entering the vagina is neutralized due to the acidic environment.
The microflora of the genital tract is not the same at different periods of a woman’s life and reflects the influence of a complex of factors from both the external and internal environment.
Even during one menstrual cycle, fluctuations in phases are detected. Thus, in the first days of the cycle, the pH of the vaginal environment rises to 5-6, which is associated with the breakdown of endometrial cells (Endometrium) and blood, while the number of lactobacilli decreases, but the balance is maintained by an increase in facultative and obligate anaerobes. At the end of menstruation, everything is quickly restored and by the middle of the cycle and the secretion phase it is 3.8-4.5, and is accompanied by the maximum number of lactoflora, glycogen and lactic acid content.
What does it mean
Normally, more than 95% of the vaginal microflora are lacto- and bifidobacteria, which maintain an acidic environment and prevent harmful microbes from multiplying. 5% is allocated to opportunistic flora: under the influence of certain factors, its representatives begin to quickly clone and displace beneficial bacteria.
Help: In the vagina of a healthy woman, beneficial and opportunistic bacilli are present in a ratio of 10:1.
Lactobacilli are the basis of the natural barrier between the external environment and the uterine cavity. Thanks to the acidic environment they create and the release of hydrogen peroxide, pathogens are neutralized, and the number of opportunistic pathogens remains low.
But if external or internal problems arise, the quantitative and qualitative composition of the flora begins to change. The level of lactobacilli decreases as the concentration of other microorganisms increases.
First of all, the rate of microbes that are constantly present in vaginal secretions increases. But the total number of bacteria also increases. All this can lead to the development of bacterial vaginosis.
A distinctive feature of the latter is the absence of a specific pathogen, since the infectious process is caused by not one, but several types of microbes.
Dysbacteriosis of vaginal microflora
When the vaginal microflora is disturbed, the number of lactobacilli decreases. Instead of the normal acidity level of 3.8-4.5, alkalization is observed, in which the pH is 4.5 or higher. This leads to a decrease in local vaginal immunity and the onset of favorable conditions for the development of infectious inflammatory and non-inflammatory diseases. Vaginal imbalance is commonly called bacterial vaginosis, dysbiosis and vaginal dysbiosis (Dysbacteriosis).

How to improve vaginal microflora
Mixed type
If a mixed flora is detected in the analysis, what does this mean? The issue is relevant for most women, and therefore special attention should be paid to it. The presence of a mixed type of flora in a smear indicates a balance between normal and pathogenic microorganisms. With this result, squamous epithelium, leukocytes, Doderlein's lactobacilli and other types of microorganisms are found in the biological material.

In the absence of an inflammatory process, the number of lactobacilli predominates (approximately 90-95%). The remaining 5% are opportunistic bacteria, which include rods and cocci. Potentially dangerous microorganisms do not harm the body, but as their numbers increase, the threat of developing pathology increases.
The risk of developing diseases with mixed abundant flora in a smear during pregnancy is very high. Carrying a child in general is a special condition of the female body, in which existing chronic diseases may worsen or new problems may appear. It may be necessary to undergo complex treatment to prevent the uncontrolled proliferation of pathogenic agents.
Disturbance of vaginal microflora: causes of imbalance
There are a number of factors that influence the likelihood of an imbalance in the vaginal flora. Among them the following can be noted:
- Hormonal surges observed during pregnancy, breastfeeding, abortion, perimenopause, menopause, transition, irregular sex life. For example, many women ask their gynecologists about how to restore the vaginal microflora after childbirth, since due to hormonal changes the mucous membrane becomes excessively dry and irritated.
Expert opinion
As soon as the level of estrogen drops for various reasons, a change in the vaginal biocenosis is observed: the number of Doderlein bacilli is reduced, which creates favorable conditions for the development of opportunistic microflora, as well as for the introduction of pathogenic agents. This is due to the influence of estrogens on the mechanism of glycogen formation and maintaining optimal conditions for the life of lactobacilli.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
- Antibacterial therapy. One of the features of antibiotics is that they destroy not only harmful, but also beneficial microorganisms. Therefore, after taking these medications, it is important to restore the disturbed vaginal microflora. And remember: under no circumstances should you take antibiotics uncontrolled for a long time without consulting a doctor, as this can lead to dire consequences.
- Regular hypothermia. They affect the level of general and local immunity, undermining the body's defenses.
- Insufficient hygiene of the intimate area. If you do not wash yourself regularly, do not change your underwear, used pads or tampons on time, there is a high probability of developing vaginal dysbiosis. Particular attention should be paid to the timely change of tampons during menstruation: this must be done every 2-3 hours, because otherwise ideal conditions are created for disruption of the vaginal microflora. You also need to wash yourself properly, directing the stream of water from the front and not from the back, since in the second case, intestinal bacteria may enter the vagina.
- Using inappropriate intimate hygiene products. For washing, it is necessary to use specialized gels and foams for intimate hygiene. They have a neutral pH level and do not cause symptoms of vaginal microflora disorders. You should also avoid using tampons and pads that contain dyes and fragrances.
- Using an intrauterine device for a long time, taking certain oral contraceptives.
- Staying in an unusual climate. Often, a change in climate zones from cool to warmer becomes one of the reasons for the imbalance of microflora.
- Stressful situations and unbalanced nutrition. Stress undermines the body's defenses, making it more susceptible to infectious processes. An unhealthy diet rich in yeast products, alcohol and simple carbohydrates also leads to a weakening of local vaginal immunity.
Why do they take a smear test for flora?
A gynecologist takes biological material from the vagina (smear for flora) from women to identify the presence of pathogenic microflora and determine the presence of pathology. In the absence of complaints, doctors previously recommended taking the test annually, but now the American Congress of Obstetricians and Gynecologists has introduced new rules. People between the ages of 21 and 65 need to have smear tests every three years.
More often, diagnostic manipulation is performed in the presence of complaints: burning or itching in the vagina, pain in the lower abdomen, changes in the consistency, color or smell of discharge. The analysis should be done during pregnancy, suspected development of gynecological pathologies, or menopause. Experts recommend doing a smear after finishing taking hormonal medications that can affect acidity levels, and regularly visiting a gynecologist.

Tests to determine the state of the vaginal microflora

Since the disease is often asymptomatic, many women learn about it only at an appointment with a gynecologist. If the doctor suspects that his patient is not healthy, he takes a urogenital smear to determine the vaginal microflora for laboratory tests. To obtain results, a smear examination with Gram staining can be used in accordance with European recommendations in accordance with the Hay-Ison scale or with the assessment of Nugent scores and the Russian recommendations of the national gynecology manual - analysis of femofloras (determination of DNA of microorganisms associated with bacterial vaginosis or assessment microscopic characteristics of the vaginal biocenosis (Kira classification).
A smear examination involves the analysis of squamous epithelium, gram-positive rods (including Dederlein's rods), leukocytes, etc.

Prevention of dysbacteriosis
As a result of the studies, the specialist can determine the composition and ratio of the vaginal microflora, the presence/absence/intensity of inflammation, and also determine the reason for the dysbiosis.
Taking an analysis to identify the ratio of beneficial and pathogenic microflora of the vagina requires certain preparation:
- It is necessary to abstain from sexual intercourse for 24 hours.
- Three days before the smear collection, you should avoid vaginal douching, the use of tampons, suppositories and other local remedies, and do not perform hygiene on the day of the test collection.
- After consulting with your doctor, it is advisable to refrain from taking antibacterial drugs for at least a few days.
Test results can usually be obtained after 1-3 days, after which it is necessary to begin appropriate treatment aimed at restoring, improving and maintaining the vaginal microflora in a normal, healthy state.
Signs of a hormonal “revolution”
Hormonal imbalance is perhaps the most key sign of the oncoming menopause . In addition to the above-mentioned manifestations of a vasomotor and emotional nature, there are also metabolic manifestations. Diseases of the cardiovascular system and musculoskeletal system may occur: atherosclerosis, hypertension, osteoporosis, osteochondrosis, vegetative-vascular dystonia syndrome and others. And all “thanks” to a decrease in the level of female sex hormones - estrogen.
The less these hormones become, the more often hot flashes, chills, sweating and other manifestations of thermoregulation disorders occur. Not to mention the fact that starting from about 35-40 years of age, calcium begins to be “washed out” from the bones in the female body, which leads to numerous ailments of the spine and joints. With the obvious progression of changes in bone tissue, the already mentioned osteoporosis occurs, which after a certain number of years is fraught with fractures, as they say, out of the blue. Everyone knows of cases where elderly people, having tripped and fallen, receive serious injuries to the hip joints, often chaining the victims to bed for the rest of their lives.
Various urogenital disorders are also frequent accompaniments of menopause. The cause is the same: a decrease in the level of sex hormones. Since many tissues and muscles in the bladder, urethra and vagina are sensitive to estrogens (or rather to their lack), atrophic and dystrophic processes are common in these organs with the onset of menopause. At best, a woman may experience that the vaginal mucosa will not be moisturized as well as before, which will cause a feeling of discomfort during sexual intercourse. At worst, she may experience impaired urinary function and prolapse (drooping) of the genital organs.
Preparations for restoring vaginal microflora

The selection of means and drugs for restoring and normalizing vaginal microflora should be done exclusively by a specialist, since self-medication can lead to an even more advanced form of dysbiosis.
Below we will look at the main categories of drugs that restore vaginal microflora.
Vaginal suppositories for restoration, normalization and improvement of vaginal microflora
Vaginal suppositories are small, oblong-shaped preparations that look like a ball, oval, cylinder or cone, with a diameter of about 1-1.5 cm and weighing from 1.5 to 6 g. They are inserted intravaginally (into the vagina) - with or without an applicator him. Vegetable and animal fats, glycerin or gelatin are used as the basis for the manufacture of vaginal suppositories. Under the influence of body temperature, suppositories lose their solid form, due to which the active substance is able to act on the vaginal mucosa.
To restore the vaginal microflora, suppositories are used based on active ingredients such as lactobacilli acidophilus, bifidobacterium bifidum, ascorbic acid, lactic acid, etc.
Is treatment required?
Mixed flora in a smear requires clarification of the diagnosis, because therapy is not required in all cases. If erosion is present, cauterization is prescribed, but some forms of the disease do not require medical intervention (only regular observation). Gonorrhea, mycoplasmosis, chlamydia, trichomoniasis and similar diseases are treated with special products containing components aimed at combating certain bacteria.
If there is a slight change in the microflora, a course of vaginal suppositories or ointments is sufficient. After finishing treatment, you need to take the test again. If the results again reveal pathological microorganisms in large quantities and mixed flora in the smear (in women, this may be a consequence of taking certain medications), you may need to undergo a course of therapy with stronger drugs.
The gynecologist may recommend additional examinations to the patient that will eliminate the possibility of an incorrect diagnosis (repeated analysis after certain preparation, for example, completion of a course of antibiotics or refusal of hormonal contraceptives, ultrasound of the pelvic organs, tests of biological fluids, etc.). It is better to immediately listen to the doctor’s advice in order to immediately clarify the diagnosis.

Gels, creams and sprays to restore vaginal microflora

Creams, gels and sprays belong to the category of local hydrophilic products. Unlike thicker, viscous and heavy ointments that have a fatty base, these products are much easier to apply, they are quickly absorbed, without leaving a greasy film feeling.
One of the effective products that has a beneficial effect on the vaginal microflora is the Ginocomfort® restoring gel. It not only helps restore normal microflora, but also protects against relapses of the disease in the future. The product contains natural ingredients such as tea tree oil, which has antimicrobial and anti-inflammatory effects, and chamomile extract, which has a regenerating effect. Bisabolol and panthenol help cope with irritation and inflammatory processes, and lactic acid helps restore normal vaginal microflora and maintain physiological acidity levels.
Features during pregnancy
Mixed microflora is often found in a smear of pregnant women. Pregnant women take this test at least three times: when issuing an exchange card and registering, up to thirty weeks and in the third trimester, shortly before giving birth, that is, at thirty-six to thirty-seven weeks. Sometimes there may be a need for additional examination: if there are complaints of itching, changes in the amount, smell or consistency of discharge, or burning.
A successful sign of conception before the onset of a delay in menstruation is a change in the nature of vaginal discharge. During implantation, immunity decreases slightly because the fertilized egg is often perceived by the body as a foreign object. Pregnant women often encounter thrush. It is important to get rid of the symptoms of this disease before delivery, because the child can become infected when passing through the mother’s genital tract.
If mixed flora is associated with serious illnesses, the doctor may recommend terminating the pregnancy. The fact is that many drugs are prohibited during pregnancy, and the lack of therapy can lead to intrauterine infection and death of the embryo. Therefore, experts recommend getting tested and undergoing treatment at the stage of pregnancy planning.

It is much easier to prevent any pathology than to eliminate it (especially if you have to be treated during pregnancy). Mixed flora in a smear in women is no exception. Do not forget about the prevention of diseases of the reproductive system and regularly visit a gynecologist. Following simple rules will not only prevent gynecological diseases, but also give birth to a healthy child.
How can you restore and improve the vaginal microflora using traditional medicine?
- Chamomile. To prepare an infusion of chamomile flowers, pour 1 tbsp into a thermos. l. dry raw materials, pour 1.5 cups of boiling water and leave to brew. Then strain the resulting infusion, strain it and do douching and insert cotton swabs soaked in chamomile infusion into the vagina.

Infusion of chamomile flowers to restore vaginal microflora
- Sea buckthorn oil. Soak a cotton swab in sea buckthorn oil and insert it into the vagina overnight.
If you decide to use any of the traditional medicines, be sure to inform your doctor. And remember: “grandmother’s” recipes can only act as additional therapy.
Vaginal microflora is normal with Gynocomfort products
If you are thinking about how to improve the vaginal microflora, be sure to check out the Ginocomfort product range.
Restoring gel "Ginocomfort" has a balanced composition developed by specialists from the pharmaceutical company VERTEX. The product has undergone clinical studies conducted at the Department of Dermatovenereology with the clinic of St. Petersburg State Medical University under the leadership of Ignatovsky A.V. and Sokolovsky E.V. As a result of research, the high effectiveness of the restorative gel as part of complex therapy for various dysbiotic disorders has been proven. Regular use of the gel will help you cope with itching, dryness and other unpleasant symptoms of dysbiosis and restore normal microflora.
You can also use Ginocomfort intimate washing gels for daily hygiene: they will ensure effective cleansing of the intimate area without drying it out and without disturbing the microflora.
All Ginocomfort products have the necessary documents and quality certificates.
What else can be found in a smear?
When performing bacterioscopy, it is possible to assess the biocenosis. This test is also called a staphylococcus smear.
But at the same time, it is possible to identify pseudomycelium, mixed microflora, fungal spores, enterobacteria, streptococci, Haemophilus influenzae, corynebacteria are determined. They are potential causative agents of vaginitis, vulvitis and vulvovaginitis.
Streptococcus agalactia and Streptococcus pyogenes are dangerous species. Regardless of the quantity of them found during culture, treatment must be prescribed.
The norm for opportunistic microorganisms in the vaginal environment is no more than 104 CFU (colony-forming units). If the content is elevated, inflammation cannot be ruled out; neutrophilic leukocytes may be present (more than 5 per field of view).
Rules for the treatment of vaginal microflora disorders, video
Video about vaginal microflora disorders.
Source - Makarova Mom Sources:
- SPECIES DIVERSITY OF VAGINAL LACTOBACILLUS IN NORMAL AND DURING DYSBIOTIC CONDITIONS. Budilovskaya O.V., Shipitsyna E.V., Gerasimova E.N., Safronova M.M., Savicheva A.M. // Journal of Obstetrics and Women's Diseases. – 2021. – No. 2. – P. 24-31.
- ENDOGENOUS MICROBIOTA OF THE VAGINA AND ITS REGULATION. Rishchuk S.V., Punchenko O.E., Malysheva A.A. // Bulletin of the Orenburg Scientific Center of the Ural Branch of the Russian Academy of Sciences. – 2013. – No. 4. – P. 1-30.
- Application of the real-time polymerase chain reaction method to assess the microbiocenosis of the urogenital tract in women. Sukhikh G.T., Prilepskaya V.N., Trofimov D.Yu., Donnikov A.E., Ailamazyan E.K., Savicheva A.M., Shipitsyna E.V. // (Femoflor test, instructions for medical technology. Moscow. - 2011. - P. 25.
- Immunology: atlas. Khaitov R.M., Yarilin A.A., Pinegin B.V. // M.: GEOTAR-Media. - 2011. - P. 624.
- Bacterial vaginosis - modern concepts, complex treatment: guidelines for obstetricians and gynecologists. Tikhomirov A.L., Oleinik Ch.G., Sarsania S.I. // Moscow. - 2005. - P. 26.
- https://bmcmicrobiol.biomedcentral.com/articles/10.1186/1471-2180-9-116
- https://www.researchgate.net/publication/272354426_LACTOBACILLUS_FOR_CORRECTION_VAGINAL_MICROFLORA/l…
- https://www.ncbi.nlm.nih.gov/pubmed/27437931
- https://www.pnas.org/content/108/Supplement_1/4680
Characteristics of scarcity and abundance
There are two main types of mixed flora - scanty and abundant . They differ in the ratio of pathogenic to harmless bacteria.
Sparse mixed flora can be easily treated without the use of potent agents. The abundant flora is corrected using the most effective drugs.
There is a third type of pathology - coccobacillary flora.
This phenomenon indicates that a woman has diseases transmitted through sexual contact or vaginal dysbiosis.
Popular questions
If a woman’s microflora is disturbed, then should her partner take pills and which ones?
If dysbacteriosis is detected in a woman, treatment and examination of her partner is mandatory. Therapy is determined by the results of the examination and prescribed by a urologist.
She took tests for microflora and cytology. After which, as usual, it was a little painful to go to the toilet, for about 1 day. Then it passed, on the trail. One day there was protected sexual intercourse, and a day later menstruation began, a burning sensation and itching appeared. It hurts to go to the toilet, there is no discharge or blood. And this has been going on for a week now. The test results are good. There were no complaints before these tests.
Have you noticed dryness during sexual intercourse or some trauma to the mucous membranes of the genital tract, which could worsen during menstruation? I recommend using Gynocomfort gel with tea tree oil, which will allow for mild anti-inflammatory therapy, heal microtraumas of the mucous membranes and balance the lactoflora in the genital tract. The gel is used in 1 dose 1 time per day for 7-10 days.
The gynecologist prescribed Tamistol suppositories for dysbacteriosis and an abundance of coccal flora. Severe pain in the lower abdomen and general malaise appeared. Could this be the cause of this condition?
Hello! The suppositories contain the antiseptic drug Miramistin, which has a wide spectrum of antimicrobial action. The occurrence of pain is not associated with their use. This is most likely a progression of the inflammatory process. You need to see a specialist again.
Hello, I have a question. My vaginal dysbiosis constantly recurs. The itching bothers me. STI-negative. I took hormone tests and the results were hyperprolactinemia and low progesterone. Could a change in the balance of these hormones cause a change in the microflora?
Hello!
An increase in prolactin levels leads to a decrease in estrogen, which can adversely affect the structure of the mucous membranes of the genital tract - leading to thinning, vulnerability, dryness, a decrease in the number of lactobacilli and a decrease in protective properties. If hormonal imbalances are detected, correction should be carried out, which will help cope with the manifestations of dysbiosis. In this case, you can additionally use Ginocomfort gel with tea tree oil, which will avoid the inflammatory process and stabilize the pH balance of the environment due to the lactic acid included in the composition. The gel is applied 1 dose 1 time per day for 7-10 days. For an accurate diagnosis, contact a specialist
Varieties
There are 2 large groups of bacteria that are found in the smear - rod and coccus. With rod flora, it is important which microorganisms are detected: small or large gram-positive.
Small rod flora indicates the presence of gram-negative pathogenic bacteria that negatively affect the immune system. The development of bacterial vaginosis, which is also called gardnerellosis or dysbiosis, is possible. To establish an accurate diagnosis, the doctor evaluates the ratio of the levels of lactobacilli, leukocytes and red blood cells.
The predominance of gram-positive, large and stable Dederlein rods, also known as lactobacilli, indicates the absence of pathology and means that the woman is healthy.
Coccal flora is a significant increase in the concentration of leukocytes against the background of the complete absence of Dederlein rods - lactobacilli. It is accompanied by characteristic symptoms of vaginosis, in which the thickness, color and smell of the discharge changes. They become thick, opaque and smelly. Antibacterial treatment is necessary here.
The second classification divides microflora depending on its quantity into scanty, moderate and abundant. In the first case, mainly lactobacilli are detected; there are few leukocytes - no more than 10; the presence of a small number of gram-positive cocci (conditional pathogens) is possible.

Leukocytes have the ability to penetrate the vascular wall and move independently. They absorb bacteria and process them, after which they are destroyed, releasing substances that cause inflammation. That is, the more leukocytes, the stronger the inflammatory process
A moderate number is said to exist if there are more than 10 leukocytes, but less than 30. In addition, there are both gram-positive and gram-negative rods and cocci. Lactobacillus levels are extremely low and key cells are present. The amount of mucus is increased.
Abundantly - this is when there are more than 30 leukocytes, there are no Dederlein bacilli, but there is a lot of mucus and various pathogenic and opportunistic microorganisms.