In medical terminology, metastases are secondary foci of growth (dropouts) of malignant tumors. Viable cancer cells, breaking away from the “maternal” tumor and penetrating the lumen of a blood or lymph vessel, move and settle in a new place. Then they begin to actively divide, forming a metastatic focus. The most extensive internal organ in terms of blood supply area is considered to be the lungs, which are one of the most common sites of tumor metastasis. In addition, various types of tumors have a tropism (craving) for the development of metastases in certain organs, most often such organs are, in addition to the lungs, the brain, liver, and bones.
Metastatic tumors
Modern oncology has information about a variety of primary malignant neoplasms that can spread, forming metastases in the lungs and other organs. This list includes:
- kidney cancer (16%);
- breast cancer (8.2%);
- colon cancer (rectum and colon) (14.3%);
- lung cancer (7.4%);
- bone sarcomas (24.1%).
In some cases, the primary tumor that triggered the screening of malignant cells remains unknown. Often, the process of metastasis does not make itself felt for a long time and is detected only during a diagnostic examination or at the very last stage of the disease.
How long do such patients live?
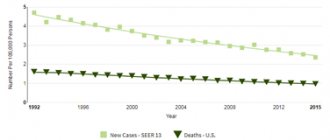
Metastatic cancer is very difficult to treat:
- The 5-year survival rate (percentage of patients still alive 5 years after diagnosis) is 1–2%.
- Median survival (time after which half of the patients died, the other half remained alive) is 6-12 months (without treatment - 2-4 months).
However, such negative statistics are not a reason to give up.
Some patients (even if only a few out of a hundred) still remain alive for a very long time, many years. No one knows in advance which of those newly diagnosed with stage IV lung cancer will be among these survivors.
In addition, science does not stand still. Now doctors and scientists have high hopes for immunotherapy and targeted drugs. Treatment methods are improving, which means the chances of defeating cancer are increasing.
Symptoms of metastatic lung disease
One of the most characteristic symptoms of metastases in the lungs is coughing. At first it can occur under the guise of prolonged bronchitis, then it becomes permanent, dry, hysterical and painful. Bloody streaks are often found in the sputum.
When a large part of the lung tissue is affected, compression or blockage of the bronchial lumen occurs, the accumulation of malignant pleural effusion (metastatic pleurisy) occurs. The patient experiences shortness of breath, the intensity of which depends on the volume of pathological fluid.
Sometimes the body temperature rises to subfebrile levels (37-38 °C) and remains there for a long time.
Pathomorphology of metastatic nodes
Metastatic nodes that form in the lungs, in their density, are an almost complete reflection of the primary malignant neoplasm. Cancer cells delivered to the lung tissue through the blood or lymphatic fluid form metastases of various shapes.
By localization, metastatic nodes are unilateral and bilateral, and by number - solitary (single peripheral neoplasms), single (2-3 nodes) and multiple (more than 3 foci).
Depending on the effectiveness of the therapeutic effect in the treatment of primary cancer, metastases in the lungs are divided into:
- for those sensitive to radiation and chemotherapy (screenings of choriocarcinoma, osteosarcoma, ovarian and testicular cancer);
- partially amenable to conservative therapy (secondary foci of non-small cell lung and breast cancer);
- resistant to radiation and chemotherapy (screenings of melanoma, cervical, endometrial, colon, kidney cancer).
Melanoma
It is diagnosed in 2.5-10% of patients and has a high probability of a malignant course and leads to death in 89% of cases. It is characterized by rapid progression and rapid transition from stages 1 to 4 of development.
This neoplasm develops from melanocytes - pigment cells of the skin. Women are more susceptible to the disease, especially after 50 years of age (at this age the risk increases sharply for all people). Most often, the tumor develops on the legs in women and on the back in men. In older patients (65 years and older), melanoma in the head and neck area is quite common.
Melanoma is the most aggressive type of cancer. The human immune system reacts poorly to this tumor, so it develops rapidly - weeks, and in some cases days, pass from the initial stage to life-threatening.
The disease quickly metastasizes, with metastases spreading both to adjacent areas of the skin and to distant organs and lymph nodes. The patient can be completely cured only at the first stage, after which the prognosis is unfavorable.
Photo of melanoma
Melanoma looks like an uneven spot several millimeters wide (in later stages - up to several centimeters), which protrudes slightly above the surface of the skin. At an early stage, it can be identified by pain and bleeding, and a change in color (usually black, dark blue, rarely red or white). Melanoma ulcerations are quite common.
It is noteworthy that this tumor can form from age spots and on clean skin as a result of injury, intense tanning, contact with carcinogens, burns or frostbite, self-medication and removal of nevi, and hormonal imbalances.
Also of great importance is genetic predisposition, endogenous constitutional characteristics and the nature of pigmentation (color of skin, hair and eyes, the presence of freckles on the face, hands, body, number, size and shape of moles on different parts of the body), skin reaction to ultraviolet rays.
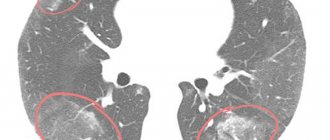
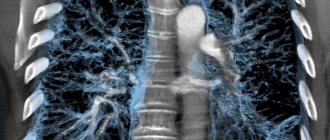
Diagnosis of pulmonary metastases
Due to the fact that metastatic nodes are most often localized in the peripheral parts of the lungs, their identification is a rather difficult task. Comprehensive diagnosis of pulmonary metastases includes the following techniques:
- Plain radiography of the lungs in frontal and lateral projections. It is carried out to clarify the location and extent of the tumor, its interaction with the root of the lung and organs located in the mediastinum.
- Computed tomography of the chest with intravenous contrast. The technique makes it possible to determine the condition of the pulmonary root, clarify the nature of the metastatic process, detect small foci with a diameter of up to 10 mm and affected intrathoracic lymph nodes.
- MRI. Magnetic resonance imaging allows you to obtain sections of the lung parenchyma to identify structural changes and the exact location of the tumor. But this method is not very informative for lung damage.
- PET-CT (positron emission tomography). Used to measure the metabolic activity of lung tissue. Allows detection of active metastatic tumors in the lungs and other organs. It is the most informative method for assessing metastatic spread.
- Fiberglass bronchoscopy. This endoscopic technique makes it possible to assess the condition of the inner surface of the bronchi and take a biopsy sample of the tumor to make the most accurate diagnosis.
- Fine needle aspiration biopsy. Prescribed for suspected tumor formation in the peripheral parts of the lung. It is performed under the control of x-ray equipment.
- Thoracentesis (pleural puncture). It is performed in the presence of pleural effusion (if the malignant tumor affects the pleura).
Treatment of metastases
Not so long ago, when a metastatic process was detected in the lungs, only symptomatic therapy was carried out, designed to alleviate the patient’s condition. However, with the introduction of innovative equipment and new, more effective treatment and diagnostic techniques, oncologists have more opportunities to radically destroy secondary tumors.
Treatment of metastases in the lungs is prescribed taking into account the histological type of the tumor, the age and general condition of the patient, as well as the presence of concomitant diseases. To increase the effectiveness of therapy and reduce the risk of complications, smoking patients are strongly recommended to quit smoking.
Currently, the following methods of combating metastases in the lungs are used in clinical practice.
Surgical removal
Classic surgical treatment of metastases in the lungs is carried out only after resection of the primary tumor (or if it is possible to completely remove it). The operation is performed with a limited number of localized nodes, their accessibility to the surgeon, the absence of screening out cancer cells in other organs, and absolute confidence that the patient will tolerate the planned treatment.
Laser resection
This type of treatment is more often used for recanalization (restoration of patency) of a bronchus with a lumen blocked by a tumor.
Chemotherapy
This is the main type of treatment for multiple metastases in the lungs. When developing a chemotherapy treatment regimen, the nature and extent of the primary tumor is taken into account.
Radiation therapy
It is prescribed both for single lesions and for multiple ones (in rare cases). The possibility of application is determined by the morphological appearance of the primary tumor, its sensitivity to radiation exposure, location and size of the lesion.
Hormone therapy
The use of hormonal drugs is advisable for metastatic spread of hormone-positive cancer. The purpose of this technique is to influence the level of hormones that can stimulate the growth of malignant tumors.
Radiosurgery
Today, one of the most progressive methods of non-invasive treatment of single metastases in the lungs is stereotactic radiosurgery. During treatment, the Cyber-Knife radiosurgical complex is used, which exposes the tumor to high-precision, high-intensity radiation.
Using sophisticated software, the system consists of a specialized linear accelerator mounted on a robotic arm. It is capable of moving in 6 directions, providing exceptional flexibility, maneuverability and precision. The targeted use of CyberKnife photon radiation beams can relieve the patient of a metastatic lesion without prolonged irradiation and the use of surgical interventions.
Risk factors and prevention of non-small cell lung cancer
A risk factor is anything that increases the likelihood of developing cancer. Although risk factors often influence the development of cancer, most do not directly cause cancer. Knowing your risk factors and discussing them with your doctor can help you make more informed lifestyle and health care choices. NSCLC most often occurs in former or current smokers. However, non-smokers may also be at risk.
The following factors may increase your risk of developing NSCLC:
- Tobacco and smoking. Tobacco smoke damages lung cells, causing them to grow abnormally. The risk that smoking will lead to cancer is higher among long-time, heavy smokers. Regular exposure to smoke from other people's cigarettes, cigars, or pipes can increase the risk of disease, even for a non-smoker. This is called exposure to environmental tobacco smoke, or secondhand smoke. Smoking marijuana and e-cigarettes also increases the risk of developing cancer.
- Asbestos . The hair-like crystals found in many types of rocks are often used as fire-retardant insulation in buildings. Inhalation of asbestos fibers causes lung irritation. Many studies show that the combination of smoking and asbestos exposure is especially dangerous. Smokers whose jobs involve asbestos in fields such as shipbuilding, asbestos mining, insulation, or automobile brake repair have a higher risk of developing NSCLC. Using respiratory protection reduces this risk.
- Radon. A colorless, odorless gas released from some types of soil and rocks. Exposure to radon is associated with an increased risk of developing cancer.
- Other substances. Other substances, such as gases or chemicals at work or in the environment, can increase the risk of developing cancer. Lung cancer is also caused by radiation, arsenic, nickel and chromium.
- Genetic factors . Some people have a genetic predisposition to lung cancer, especially those with a strong family history.
Prevention
The main way to prevent lung cancer is to quit smoking. Non-smokers have the lowest risk of developing a tumor. People who quit tobacco are less likely to get sick, but they will still be more likely to get sick than those who have never smoked.
Diagnostics and treatment at PET Technology
The federal network of nuclear medicine centers "PET Technology" has extensive experience in conducting PET-CT scanning and radiosurgery using the CyberKnife system. We offer early diagnosis of cancer and a specialized course of treatment for many primary tumors and metastases. Also, to confirm or refute a questionable diagnosis, PET Technology offers its patients to use and receive an expert opinion from our oncologists.
operate in several regions of Russia. To receive an online consultation and make an appointment, you can contact our operator at the contact number, use the form on the website or request a call back.