13.11.2017
Diabetes mellitus is a group of diseases of the endocrine system that develop due to the lack or absence of insulin (hormone) in the body, resulting in a significant increase in the level of glucose (sugar) in the blood (hyperglycemia).
Diabetes mellitus is mainly a chronic disease. It is characterized by metabolic disorders - fat, carbohydrate, protein, water-salt and mineral. In diabetes mellitus, the functions of the pancreas, which actually produces insulin, are impaired.
Insulin is a protein hormone produced by the pancreas, the main function of which is to participate in metabolic processes - the processing and conversion of sugar into glucose, and the further transport of glucose into cells. In addition, insulin regulates blood sugar levels.
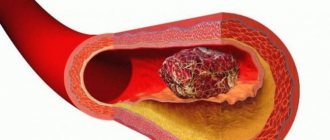
In diabetes, cells do not receive the necessary nutrition. It is difficult for the body to retain water in the cells, and it is excreted through the kidneys. Disruptions occur in the protective functions of tissues, the skin, teeth, kidneys, and nervous system are affected, the level of vision decreases, atherosclerosis and hypertension develop.
In addition to humans, the disease can also affect some animals, such as dogs and cats.
Diabetes mellitus is inherited, but it can also be acquired in other ways.
How does diabetes develop?
The hormone insulin converts sugar into glucose, which is an energy substance necessary for the normal functioning of body cells. When there is a failure in the production of insulin by the pancreas, disturbances in metabolic processes begin. Glucose is not delivered to the cells and settles in the blood. The cells, in turn, starving, begin to malfunction, which externally manifests itself in the form of secondary diseases (diseases of the skin, circulatory system, nervous and other systems). At the same time, there is a significant increase in blood glucose (hyperglycemia). The quality and effect of blood deteriorate. This whole process is called diabetes.
Why is high blood sugar harmful?
High blood sugar levels can cause dysfunction of almost all organs, including death. The higher the blood sugar level, the more obvious the result of its action, which is expressed in:
- obesity;
- glycosylation (sugarification) of cells;
- intoxication of the body with damage to the nervous system;
- damage to blood vessels;
- the development of secondary diseases affecting the brain, heart, liver, lungs, gastrointestinal tract, muscles, skin, eyes;
- manifestations of fainting states, coma;
- lethal outcome.
Symptoms of diabetes
Diabetes mellitus in most cases develops gradually, and only occasionally does the disease develop rapidly, accompanied by an increase in glucose levels to a critical level with various diabetic comas.
The first signs of diabetes
- constant feeling of thirst;
- constant dry mouth;
- increased urine output (increased diuresis);
- increased dryness and severe itching of the skin;
- increased susceptibility to skin diseases, pustules;
- prolonged wound healing;
- a sharp decrease or increase in body weight;
- increased sweating;
- muscle weakness.
Signs of diabetes
- frequent headaches, fainting, loss of consciousness;
- blurred vision;
- heart pain;
- numbness in the legs, pain in the legs;
- decreased skin sensitivity, especially on the feet;
- swelling of the face and legs;
- liver enlargement;
- prolonged wound healing;
- high blood pressure;
- the patient begins to smell of acetone.
Complications of diabetes
Diabetic neuropathy - manifested by pain, burning, numbness of the extremities. It is associated with disruption of metabolic processes in nervous tissue.
Edema. Swelling in diabetes can spread locally - on the face, legs, or throughout the body. Swelling indicates a disturbance in the functioning of the kidneys, and depends on the degree of heart failure. Asymmetrical swelling indicates diabetic microangiopathy.
Leg pain. Pain in the legs with diabetes, especially when walking and other physical activity on the legs, may indicate diabetic microangiopathy. Leg pain during rest, especially at night, indicates diabetic neuropathy. Often, leg pain in diabetes is accompanied by burning and numbness in the feet or some parts of the legs.
Trophic ulcers. Trophic ulcers in diabetes mellitus, after pain in the legs, are the next stage in the development of diabetic angio- and neuropathy. The types of wounds differ greatly from each other, so treatment of trophic ulcers in diabetes is prescribed after an accurate diagnosis, noting the smallest symptomatic details. The negative impact of ulcers is a decrease in the sensitivity of the affected feet, which occurs due to damage to the nerves when the foot is deformed. In some places, this results in corns, under which hematomas are formed with further suppuration. All these processes often occur unnoticeably, so people, as a rule, go to the doctor whose leg is already very swollen, red, and has a trophic ulcer.
Gangrene. Gangrene in diabetes mellitus in most cases is the result of diabetic angiopathy. The onset of gangrene occurs due to damage to small and large blood vessels in the area of the lower limb, most often the big toe. In this case, the patient feels severe pain in the foot. Redness of the damaged area occurs, which over time gives way to bluish skin, and after some time, this area becomes covered with black spots and blisters with cloudy contents. The process is irreversible - amputation of the limb is necessary. The optimal level of limb amputation is the lower leg.
High and low pressure. High and low pressure in diabetes mellitus is observed simultaneously in two points of the body. In the upper part of the body (in the brachial artery) there is increased pressure, which indicates kidney damage (diabetic nephropathy). In the lower part of the body (in the vessels of the legs) there is low pressure, which indicates the degree of diabetic angiopathy of the lower extremities.
Coma. Coma with diabetes occurs extremely quickly. A sign of coma in diabetes is the patient's lethargy and fainting. Before this, a person may smell of acetone coming from the mouth when breathing, which is due to extreme intoxication of the body. In addition, the patient may break into a cold sweat. If the patient exhibits at least one of these signs, he must be taken to a medical facility immediately.
Causes of diabetes
There can be quite a few causes of diabetes, so let’s highlight the most significant:
- heredity;
- age (the older the person, the greater the likelihood of getting sick);
- obesity;
- nervous tension;
- diseases that destroy beta cells of the pancreas that produce insulin: pancreatic cancer, pancreatitis, etc.;
- viral infections: hepatitis, chickenpox, rubella, influenza, etc.
In addition, diabetes mellitus can develop against the background of:
- hyperfunction of the adrenal glands (hypercortisolism);
- tumors of the gastrointestinal tract;
- increased levels of hormones that block insulin;
- liver cirrhosis;
- hyperthyroidism;
- poor digestibility of carbohydrates;
- short-term increase in blood sugar levels.
According to the severity of the disease:
Diabetes mellitus 1 degree (mild form). Characterized by a low level of glycemia (blood sugar) - no more than 8 mmol/l (on an empty stomach). The level of daily glucosuria is no more than 20 g/l. May be accompanied by angioneuropathy. Treatment at the level of diet and taking certain medications.
Diabetes mellitus 2 degrees (moderate form). Characteristic is a relatively small, but already with a more obvious effect, increase in glycemic levels at the level of 7-10 mmol/l. The level of daily glucosuria is no more than 40 g/l. Manifestations of ketosis and ketoacidosis are periodically possible. Severe disturbances in the functioning of organs do not occur, but at the same time, some disturbances and signs in the functioning of the eyes, heart, blood vessels, lower extremities, kidneys and nervous system are possible. Possible signs of diabetic angioneuropathy. Treatment is carried out at the level of diet therapy and oral administration of sugar-lowering drugs. In some cases, your doctor may prescribe insulin injections.
Diabetes mellitus stage 3 (severe form). A typical average glycemic level is 10-14 mmol/l. The level of daily glucosuria is about 40 g/l. There is a high level of proteinuria (protein in the urine). The picture of clinical manifestations of target organs—eyes, heart, blood vessels, legs, kidneys, nervous system—is enhanced. Vision decreases, numbness and pain appear in the legs, and blood pressure increases.
Diabetes mellitus stage 4 (super severe form). A typical high level of glycemia is 15-25 mmol/l or more. The level of daily glucosuria is over 40-50 g/l. Proteinuria increases, the body loses protein. Almost all organs are affected. The patient is prone to frequent diabetic comas. Life is maintained purely on insulin injections - at a dose of 60 OD or more.
Steps on the path to health. Sugar slightly increased. Is it so harmless?
Yes, this “triad” - excess weight, high blood sugar, cardiovascular diseases - always appears together. And most importantly, everything grows very gradually, unnoticed over a long time and often without symptoms. And at some point in your life, as always at the wrong time, you are given a diagnosis, which is followed by multiple changes in the body. After all, type 2 diabetes mellitus is a chronic disease associated with metabolic disorders, accompanied by a malfunction of the endocrine system and at least one cardiovascular disease, for which, in fact, you see a doctor. But the most unpleasant thing can happen later, when complications of type 2 diabetes mellitus - the result of just an unhealthy lifestyle - lead to irreversible consequences and disability. People tend to be afraid of type 1 diabetes (insulin-dependent), but in fact, type 2 diabetes is more insidious, dangerous and more common among all types of diabetes.
According to the International Diabetes Federation, by 2040, 642 million people will suffer from diabetes. The rapid increase in the incidence of diabetes mellitus was the reason for the adoption of the UN Resolution (61\225 of December 20, 2006 “On diabetes mellitus”), and in 2011 the UN Political Declaration addressed to national health care systems.
The results of a large-scale Russian epidemiological study (NATION) confirm that only 50% of cases of type 2 diabetes are diagnosed, and that the real number of patients in the Russian Federation is at least 8–9 million people (about 6% of the population).
In response to the rapid increase in the number of diabetes cases worldwide, the International Diabetes Federation and the World Health Organization declared November 14 as World Diabetes Day in 1991.
The most dangerous consequences of diabetes mellitus (DM) are systemic vascular lesions and complications: nephropathy (vascular lesions in the glomeruli of the kidneys), damage to the mitral vessels of the heart (vessels that supply the heart itself), brain, peripheral vessels of the lower extremities (often leading to amputation). It is these complications that cause disability and mortality in patients with diabetes.
According to the International Diabetes Federation, every 12 minutes a patient with diabetes suffers a stroke, every 19 minutes a heart attack, every 90 minutes a loss of vision, every 30 minutes a loss of a leg, and every 10 minutes doctors record a death caused by complications of this terrible disease. .
In order to prevent the development of irreversible processes in the body, it is necessary that an accurate diagnosis be made as early as possible. As early as possible, you should start taking measures to prevent the development of diabetes: losing weight and establishing a healthy lifestyle, reducing all elevated indicators (it is always better to focus on the average or lower level of the norm) - sugar, cholesterol, uric acid and others. After all, a diagnosis is already a disease, and action must be taken during the pre-illness period.
I have already mentioned in my articles that diabetes is a consequence of impaired insulin secretion, insulin action, or both of these factors and is accompanied by hyperglycemia.
Chronic hyperglycemia (consistently elevated blood sugar) always leads to damage and dysfunction of various organs: especially the eyes, kidneys, nerves, heart and blood vessels.
This type of diabetes mellitus is caused by a decrease in the sensitivity of cells to the action of insulin (insulin resistance), which in the initial stages of the disease is synthesized by the pancreas in normal and even increased quantities. It does not require lifelong insulin administration. Correction of blood sugar levels is possible only through physical activity, diet or a balanced diet.
In addition to diabetes mellitus of the first (insulin-dependent) and second (non-insulin-dependent) types, diabetes mellitus of the third type is now distinguished, which occurs with chronic or acute damage to the pancreas itself: pancreatitis/inflammation, trauma, neoplasms, cystic fibrosis, fibrocalculous pancreapathy, surgical operations. It is not associated with obesity or heredity, but only with the pathology of the pancreas itself.
It should be noted that the so-called gestational diabetes mellitus .
The risk group includes young women (usually without excess body weight) who experience periodic increases in blood sugar associated with diet (the so-called impaired glucose tolerance). Which, in the presence of a hereditary predisposition (which they may not even know about), can lead to severe complications and the development of type 1 diabetes during pregnancy.
Why does gestational diabetes develop? The reason is the so-called “counter-insulin” effect - blocking the action of insulin by hormones that are produced in a woman’s body during pregnancy and are involved in maintaining the required blood sugar level. Typically, gestational diabetes mellitus begins to appear between 20 and 24 weeks of pregnancy. This is facilitated by overwork, unbalanced nutrition, half-starvation, stress, and various diseases.
If a pregnant woman’s fasting blood sugar level is more than 5.3 mmol/l, and 2 hours after eating it reaches 6.8 mmol/l or more, then it is necessary to consult a specialist to clarify the diagnosis and correct the condition.
Why don't all pregnant women develop GDM? Because this is facilitated by a hereditary predisposition, which is realized under the influence of certain risk factors:
- overweight and obesity;
- the presence of diabetes mellitus in relatives (a genetic analysis can be done to determine a hereditary predisposition to diabetes);
- first pregnancy complicated by GDM; the birth of a child weighing more than 4000 g, with a large abdominal circumference;
- age over 25 years;
- chronic miscarriage (more than three times) in the 1st or 2nd trimester;
- fetal stillbirth; developmental defects in previous children.
When planning a pregnancy, it is important to pay attention to your blood sugar levels by reviewing your previous tests. Normally it is 3.5–4.5 mmol/l.
It is very important to control blood pressure in type 2 diabetes mellitus, since type 2 diabetes mellitus and hypertension almost always go hand in hand. And a blood pressure level of 130/80 in combination with diabetes mellitus and prolonged hyperglycemia is accompanied by a high risk of microvascular complications.
71% of people with diabetes suffer from hypertension, and very few undergo adequate drug therapy to lower blood pressure levels, and many do not think about the consequences and complications at all, ignoring the recommendations of doctors. Patients with type 2 diabetes mellitus have an increased tendency to thrombosis, which contributes to the progression of atherosclerosis and its complications.
A companion to type 2 diabetes is also coronary heart disease (CHD) - myocardial damage due to tissue ischemia (impaired nutrition and oxygen supply to the heart).
What are the features of cardiac ischemia in type 2 diabetes mellitus?
- The disease is asymptomatic, the so-called “silent” painless forms of coronary artery disease and myocardial infarction.
- The risk of development is the same in men and women over the age of 45 years.
- High risk of sudden death.
- High incidence of post-infarction complications: congestive heart failure, heart rhythm disturbances.
Guarantees of a severe course of IHD will be: the presence of high cholesterol levels, constantly elevated blood pressure (160–180 mmHg); duration of diabetes mellitus more than 15 years; the presence of vascular complications: nephropathy and retinopathy.
That is, if blood sugar is elevated for a long time, it means that by the age of 40–45, a person already has at least one of the cardiovascular diseases. Often this is hypertension or asymptomatic ischemic heart disease detected during examination.
According to statistics, the presence of diabetes mellitus increases the risk of coronary artery disease by 2–4 times, and with the initial detection of diabetes, diffuse damage to the coronary arteries supplying the heart is often already observed. In diabetes, there is a high probability of stenosis at the site of stent implantation. Mortality due to the development of acute coronary syndrome in patients with diabetes mellitus is 2–3 times higher.
Obesity is a classic factor that provokes the development of diabetes mellitus and aggravates its course. With a decrease in body weight, insulin resistance decreases, and the cells begin to better perceive insulin and receive glucose. Blood pressure and cholesterol levels improve.
The statistics are that 90% of patients with diabetes are obese. Long-term weight loss in patients with type 2 diabetes mellitus is possible through an integrated approach: lifestyle changes, a balanced diet, and a developed individual plan for physical exercise and exercise.
No less dangerous complications of a long-term increase in blood sugar are: diabetic nephropathy, rhinopathy, the appearance of glycated hemoglobin and neuropathy. What it is? Diabetic nephropathy is kidney damage in the area where urine is filtered, which disrupts the water and electrolyte balance and leads to even more negative consequences.
Diabetic rhinopathy is vascular changes in the retina that threaten vision loss.
Damage to the renal glomeruli occurs in parallel with damage to the vessels of the fundus (80%). Advanced diabetes mellitus “hits” the eyes and kidneys.
We know that hemoglobin in red blood cells carries oxygen to tissues and to the brain. In diabetes mellitus, glycated hemoglobin is determined in the blood. What does this mean? This is a specific combination of red blood cell hemoglobin with glucose. Its concentration reflects the average blood glucose level over the past three months. Hemoglobin must carry oxygen, but when there is a lot of sugar, it combines with glucose, and the space for binding oxygen in it decreases. Glycated hemoglobin is a very stable compound (breaks down slowly), which is not very good for the body, its tissues and brain.
Diabetic neuropathy is damage to nerve tissue. Occurs due to a malnutrition of the nervous tissue, again with the participation of capillaries.
Diagnosis of diabetes mellitus
The following methods and tests have been established for diagnosing diabetes mellitus:
- measuring blood glucose levels (determination of glycemia);
- measurement of daily fluctuations in glycemic levels (glycemic profile);
- measuring insulin levels in the blood;
- glucose tolerance test;
- blood test for the concentration of glycosylated hemoglobin;
- blood chemistry;
- urine test to determine white blood cell, glucose and protein levels;
- Ultrasound of the abdominal organs;
- Rehberg's test.
In addition, if necessary, carry out:
- study of blood electrolyte composition;
- urine test to determine the presence of acetone;
- fundus examination;
- electrocardiography (ECG).
Treatment of diabetes
Before starting treatment, it is necessary to conduct an accurate diagnosis of the body, because a positive prognosis for recovery depends on this.
Treatment of diabetes is aimed at:
- decreased blood sugar levels;
- normalization of metabolism;
- preventing the development of diabetes complications.
Further, treatment varies depending on the type of diabetes. Let's look at them separately.
Treatment of type 1 diabetes (insulin dependent)
As we already mentioned in the middle of the article, in the “Classification of Diabetes Mellitus” section, patients with type 1 diabetes constantly need insulin injections, since the body cannot produce this hormone itself in sufficient quantities. There are currently no other methods of delivering insulin to the body other than injections. Insulin-based tablets will not help with type 1 diabetes.
In addition to insulin injections, treatment for type 1 diabetes includes:
- diet;
- performing dosed individual physical activity (DIPE).
Treatment of type 2 diabetes (non-insulin dependent)
Type 2 diabetes is treated by following a diet and, if necessary, taking antihyperglycemic drugs, which are available in tablet form.
Diet for type 2 diabetes mellitus is the main method of treatment due to the fact that this type of diabetes develops due to improper nutrition of a person. With improper nutrition, all types of metabolism are disrupted, therefore, by changing their diet, a diabetic in many cases gets better.
In some cases, with persistent types of type 2 diabetes, the doctor may prescribe insulin injections.
Diet for diabetes
When treating any type of diabetes, diet therapy is a must.
A nutritionist for diabetes mellitus, after receiving tests, taking into account age, body weight, gender, lifestyle, outlines an individual nutrition program. When dieting, the patient must calculate the amount of calories, proteins, fats, carbohydrates, vitamins and microelements consumed. The menu must be followed strictly as prescribed, which minimizes the risk of developing complications of this disease. Moreover, by following a diet for diabetes, it is possible to defeat this disease without additional medications.
The general emphasis of diet therapy for diabetes is on eating food with minimal or no content of easily digestible carbohydrates, as well as fats, which are easily converted into carbohydrate compounds.
Diabetes symptoms
Common initial symptoms of diabetes (Fig. 1) include:
- dry mouth, constant thirst. A person consumes a lot of fluid, so he experiences frequent urge to go to the toilet;
- strong feeling of hunger;
- causeless weight loss or, conversely, sudden weight gain, development of obesity;
- poor wound healing. As a result, pustules and ulcers appear;
- More rare cases include memory loss and headaches.
Figure 3. Some common symptoms of diabetes.
Source: medindia.net But since the disease has several types (sugar, gestational, non-sugar), it proceeds in different ways. In some cases, the patient is not even aware of the presence of diabetes and the diagnosis is made by chance: during a clinical examination or hospitalization for a completely different disease.
Symptoms of type I diabetes
Type I diabetes mellitus occurs at a young age, but can also be congenital. In this case, the pancreas either does not produce insulin at all or produces insufficient amounts. The only treatment is insulin injections. It’s not for nothing that this type of disease is called insulin-dependent diabetes.
Important! If a person with diabetes does not eat on time, injects himself with too much insulin, or overdoes physical training, his blood glucose concentration may sharply decrease - hypoglycemia will occur. This is a life-threatening condition whose symptoms can be frightening. Hypoglycemia can result in loss of consciousness, seizures and coma. All patients with diabetes, their friends and relatives should know and recognize the first signs of hypoglycemia, including:
- weakness,
- loss of orientation,
- blurred vision,
- increased sweating,
- headache,
- strong feeling of hunger.
If there is a sharp decrease in the patient's blood glucose concentration, hypoglycemia may occur. Photo: GrinPhoto/Depositphotos
Symptoms of type II diabetes mellitus
This type is called insulin-independent. After all, the pancreas produces insulin, but the body develops resistance to it (insulin resistance). In the early stages of the disease, glucose-lowering drugs are usually sufficient to treat type II diabetes.
According to doctors, this type of diabetes has become “younger.” The disease usually occurred in people over 40 years of age, but now teenagers also suffer from type II diabetes.
This type may have no symptoms. Among the most common:
- change in body weight: a person suddenly loses weight or, conversely, gains it. Obesity is not a symptom of diabetes, but can lead to it;
- scratches that take a long time to heal and fester. As a result, ulcers occur (mainly on the feet);
- memory loss due to constant fluctuations in blood sugar.
Symptoms such as thirst, dry mouth, and frequent urination are much less characteristic of the disease and only with very high blood sugar levels.
One of the symptoms of diabetes is a sudden change in body weight. Photo: dexteris/Depositphotos
Symptoms of Gestational Diabetes
Gestational diabetes (or pregnancy diabetes) is diabetes that occurs during pregnancy and goes away immediately after it.
Every pregnant woman develops insulin resistance, which can lead to pathology. Diabetes may go away after childbirth or remain, especially in women who are obese or have a genetic predisposition to the disease. In a number of cases, women had type II diabetes before pregnancy, but the disease did not manifest itself in any way.
Every pregnant woman, after registering at the antenatal clinic, is screened for gestational diabetes. For control, the doctor takes a blood test for sugar and the level of glycated hemoglobin, and then, at 24-28 weeks of pregnancy, a glucose tolerance test. Three days after birth, women diagnosed with gestational diabetes undergo a control test. If the blood sugar level has returned to normal, the diagnosis is removed; if it is not normal, further observation is necessary.
Symptoms of diabetes insipidus
The main cause of diabetes insipidus is the lack of production of a certain pituitary hormone (antidiuretic hormone). This is the hormone that affects water-salt metabolism.
The main symptom is the consumption of large amounts of fluid and frequent urge to go to the toilet. The patient can drink 15–20 liters of fluid per day and excrete the same amount. The patient's health is normal and there are no other complaints. The patient's sugar level is normal, but the specific gravity of the urine is low. In other words, a person pees with water.