TORCH-complex
- these are intrauterine infections that are especially dangerous for the child and can cause his death (first trimester), severe malformations (first trimester), multiple organ damage (second, third trimesters).
The name of the complex is an abbreviation of the first letters of the names of these infections. It was adopted in 1971 by the World Health Organization:
- T - Toxoplasma - toxoplasmosis,
- O - Other - others: originally - syphilis, now, when pronouncing other, they talk about mycoplasma, syphilis, hepatitis, streptococci, candida and other viral / bacterial infections;
- R - Rubella - rubella;
- C - Cytomegalovirus - cytomegalovirus, cytomegaly;
- H - Herpes simplex virus - simple herpes of the first, second type.
Infections from the TORCH complex are dangerous if a woman is initially infected during pregnancy or immediately before it and her body does not have immunity to the disease.
During an infection in the acute stage, there is a high probability of termination of pregnancy in any trimester and the development of severe pathologies in the child. Chronic infection is much less dangerous. A blood test for TORCH complex infections must be done:
- when planning pregnancy, for the first time - 9 months before it, then immediately before it;
- during pregnancy as directed by a doctor;
- after birth, if the child has developmental defects and clinical signs of intrauterine infection.
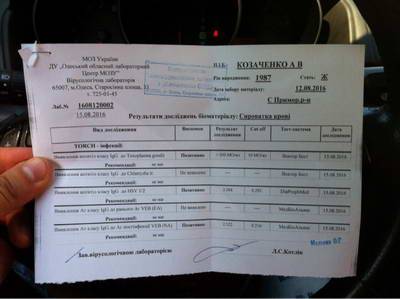
Analysis for torch infections
Diseases of the TORCH complex
Toxoplasmosis
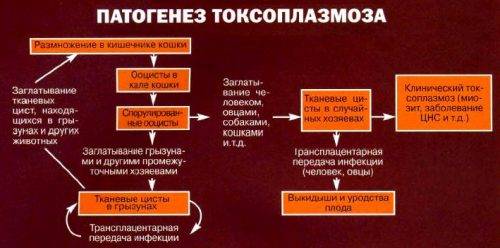
According to the most conservative estimates, more than half of the people around the world are infected with toxoplasmosis. This disease is caused by the Toxoplasma gondii parasite, which can pass to humans from any domestic warm-blooded animals, but primarily from cats, in whose bodies Toxoplasma multiplies. Infection of a pregnant woman can occur not only through direct contact with an animal, but also at the moment when the woman cleans the tray. Other sources of invasion:
- insufficiently cooked, fried meat, especially pork, sheep, poultry;
- contact with raw meat, for example when cooking it;
- intrauterine infection.
When infected with Toxoplasma, an adult may not regard his condition as a disease. The temperature may rise slightly to subfebrile (37.1-38.0 °C), sometimes headache, soreness of the lymph nodes, and fatigue occur. Often toxoplasmosis occurs in a completely latent form.
If a woman becomes infected with Toxoplasma during pregnancy, in approximately 30% of cases, Toxoplasma tachyzoites infect the placenta and infect the fetus. A negative prognosis for the fetus also exists if the expectant mother is infected 3-9 months before pregnancy.
Important!
Since infection even a few months before pregnancy is fraught with fetal death or severe pathologies, it is necessary to undergo testing for TORCH complex infections before you plan a pregnancy. Infection with Toxoplasma during pregnancy is fraught with:
- for 9 months and in the first trimester - developmental deviations incompatible with life (loss of a child);
- second trimester - pathologies of the nervous system, brain, visual organs;
- third trimester - organ damage, but a favorable outcome is also likely.
Basic methods for detecting TORCH infections
The main, most accurate method for simultaneously determining all of the above infections, as well as the presence of antibodies to them, is the TORCH test. This is a serological test that examines blood plasma. This test is based on innovative ELISA technology (enzyme-linked immunosorbent assay).
It allows:
- determine with a high degree of certainty the presence or absence of a disease;
- draw a conclusion whether the patient was previously ill or not;
- monitor the results of drug therapy.
To perform the procedure, a unique Immunocomb complex is used. It is a set of 3 so-called “combs”, on 12 teeth of which marker substances are applied pointwise, having:
- increased sensitivity to antibodies and antigens of a certain type;
- capable of changing color upon contact with them.
Packed in aluminum foil in developing baths with cells that already contain reagents, designed to perform up to 36 different analyzes simultaneously, for about 40 minutes.

The kit is supplemented with a puncher for opening the foil and a diluent (used if it is necessary to pre-process the blood sample). The possibility of visual and automated recording of results is provided. No additional testing equipment is required.
At the request of the patient and the doctor’s recommendation, it is possible to perform:
- a simple analysis consisting of 8 tests and capable of detecting IgG and IgM antibodies to TORCH infections;
- extended analysis, which also evaluates immunity to these diseases (12 tests).
If necessary, it is possible to perform tests for the presence of infections from group “O”.
Among the advantages of the ELISA method:
- high information content and reliability;
- the ability to perform tests for several diseases at once;
- no need for complex, expensive equipment;
- speed of execution.
TORCH infections are a disease that can be detected and identified in several ways:
| Diagnostic method | Description |
| RIF – immunofluorescence reaction | The method is based on the ability of antibodies to glow when treated with one or another immunofluorescent drug. Based on the characteristic glow and its intensity, conclusions are drawn about the presence or absence of antibodies. The advantage is the ability to quickly obtain results, the disadvantage is the need to use expensive equipment and high requirements for the professionalism of personnel. |
| NIIF – indirect immunofluorescence method | It is rarely used because it produces a large error and often causes an erroneous diagnosis. |
| PCR – polymer chain reaction | One of the most accurate direct diagnostic methods, based on DNA analysis of the pathogen. The disadvantage is the high cost and the need to use specific equipment, which is not available in every clinic. |
Other infections
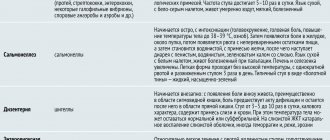
Syphilis
Syphilis is a bacterial disease from the group of STDs that can be transmitted from mother to child during pregnancy or during childbirth. Infection in the first trimester sometimes leads to miscarriage. If the fetus is preserved, the child may be born with pathologies of the visual organs, teeth, nervous system, deafness, and others. Congenital syphilis is very dangerous because even complete destruction of the pathogen in the child’s body will not stop pathological changes, which only worsen with age.
HIV
Congenital HIV is the result of the spread of the virus to children born or breastfed by mothers infected with the virus.
However, not every child born to an HIV-infected mother will become infected with the virus. To increase the chances of having a healthy baby, you need to strictly follow your doctor's recommendations, undergo antiretroviral therapy and consciously choose a cesarean section. With treatment, the risk of transmission of the virus from mother to child in developed countries today is about 1%. Important!
In Russia, cases have become more frequent when prosperous, apparently healthy women do not even suspect that they are infected with HIV. Therefore, even if you lead a very strict, healthy lifestyle and have one sexual partner, you must be tested for TORCH complex diseases before planning a pregnancy.
Varicella (chickenpox)
The causative agent of chickenpox is Varicella zoster, a virus from the herpetic family. It is especially dangerous for a woman to become infected a few days before giving birth and in the first 20 weeks of pregnancy. If Varicella zoster infection occurs before birth, in 1 case out of about 8 a child develops congenital chickenpox, which is accompanied by extensive bronchopneumonia, diarrhea, perforation of the small intestine, and damage to other organs. As a result of infection, up to a third of newborns die. Infection in the first 20 weeks of pregnancy is fraught with spontaneous abortion, intrauterine fetal death, and congenital chickenpox syndrome, which leads to pathologies of the organs of vision, brain, and limbs.
Chlamydia
Chlamydia is a disease from the STD category. For a child infected from the mother in utero or during the birth canal, it is dangerous due to eye infection and pneumonia with complications. To avoid infection, you need to undergo treatment before planning a pregnancy or during it.
Hepatitis B, C
If the mother is infected with viral hepatitis, the likelihood of “vertical” infection (in utero, during childbirth) is quite high. The infection is dangerous because during pregnancy it is often activated in the body and more often affects women who have not yet been infected.
The result of viral hepatitis is spontaneous abortion, non-developing pregnancy (frozen fetus), polyhydramnios, developmental anomalies, antenatal death, the birth of a child with diseases and pathologies, primarily of the liver. With congenital hepatitis, liver failure, cirrhosis, and cancer can develop.
Rubella
Rubella infection is especially dangerous at the beginning of pregnancy. In the first trimester, approximately a quarter of the embryos suffer from infection, and after 4 months the child is already relatively safe. Infection of the mother with Rubella virus can provoke in the child the development of multiple defects syndrome (congenital rubella syndrome, or Greg's triad) with congenital cataracts, deafness, and heart defects.
Cytomegalovirus
Cytomegalovirus is one of the herpes viruses type 5, and therefore infection with it is very dangerous for a pregnant woman and her child. The result of invasion can be:
- miscarriage;
- death of a child in utero or after childbirth;
- physical and mental diseases associated with damage to the brain and nervous system.
Herpes
Infection with the herpes simplex virus (labial, commonly known as a cold sore) in early pregnancy can lead to the development of autism in a child, especially a boy. Invasion in the first trimester increases the risk of miscarriage, development of pathologies of the central nervous system, brain, organs of vision, hearing, and deviations in physical development.
Important!
The danger of TORCH complex infections is that they may not manifest themselves in any way in an adult woman, but “work” during pregnancy. Since the consequences of each disease are extremely serious, you need to undergo testing for the entire complex when planning a pregnancy, and then undergo testing at the frequency recommended by the doctor.
Preventive measures

All diseases in this group are very common. You can encounter them not only on the street, but also at home, in your own kitchen or when caring for your pets. Therefore, preventing infection during pregnancy is very important. For this reason, it is important to plan for pregnancy before it occurs. In the absence of positive results for the presence of antibodies in the body of the expectant mother, it is necessary to protect yourself as much as possible from the penetration of pathogens.
Only against rubella there is the most reliable method of prevention - vaccination. In the countries of the post-Soviet space it is mandatory.
If the pregnancy is planned, then it is best to get vaccinated against the rubella virus prematurely. However, surveys show that antibodies are present in 86% of women who have once had this disease and are not at risk of re-infection.
The differences between rubella and toxoplasmosis are that persistent antibodies are produced to the first virus, while antibodies to the second are produced in only 40% of patients. Toxoplasma infection most often occurs due to poor heat treatment of meat.
For reference! Very often, furry pets - dogs and cats - become the source of infection. For this reason, many give their pets to other owners while they are pregnant, believing that they pose a danger. But it is not always the case. Most often, owners of felines have long had antibodies to toxoplasmosis. But having a tailed friend is not advisable for those who have not had one before during pregnancy. However, if tests for the presence of antibodies are positive, there is no need to worry.
The situation is completely different with regard to herpes and cytomegalovirus. Herpetic infections, as a rule, affect the body at an early age. These pathogens are transmitted primarily by airborne droplets. Almost everyone (about 98% of the world's population) is carriers of these pathogens. With good immune defense of the body, they are suppressed and do not pose a threat. But when the body’s defenses are suppressed, these infections can manifest themselves. Therefore, the only way to prevent these diseases is to strengthen the body’s defenses using well-known methods, namely:
- healthy lifestyle;
- getting enough sleep;
- compliance with the regime;
- proper and balanced nutrition;
- avoiding stressful situations.
Important! During pregnancy, you need to avoid colds and limit your stay in places where there are a large number of people.
Strengthening the immune system while carrying a baby will help avoid periods of exacerbation of herpetic infections and protect against negative consequences.
How is basic testing for TORCH complex infections performed?
For the test, you need to donate blood from a vein on an empty stomach.
Preparing for testing:
- stop taking antiviral and antibacterial drugs approximately 3 weeks beforehand;
- 12 hours before the test, avoid eating, smoking, alcoholic drinks, and high physical activity;
- Stop taking any medications 12 hours before the test. If this is not possible, consult your doctor and/or inform the laboratory technician of the situation.
The test results are known after a few minutes: the deadline can be found directly in the laboratory where the research is carried out.
When to get tested
Since TORCH infections are most dangerous in the first trimester, it is recommended to do the test in the earliest stages of pregnancy.

Cases that deserve special attention are:
- there are symptoms that may indicate the presence of one of the diseases;
- the infection was diagnosed based on laboratory test results;
- the pregnant woman has had miscarriages or stillbirths in the past;
- there is a factor that increases the risk of infection for a pregnant woman: for example, the presence of a cat in the apartment, a disease diagnosed in someone in the household;
- recently suffered a serious illness, which could lead to a general weakening of the body;
- pregnant women are susceptible to inflammatory diseases of the genital organs;
- to women who have already given birth, when signs of congenital pathologies are detected in the child, the cause of which may be TORCH infections suffered during intrauterine development. In this case, examination of the newborn is also necessary. In such circumstances, a woman should get tested as soon as possible, even if she feels completely healthy.
In the absence of antibodies to any of the TORCH infections, the threat of infection remains, so the pregnant woman is recommended to repeat the procedure every 2-3 months of pregnancy, limiting herself to performing tests for these diseases.
In addition, regardless of the results of the first test, it is advisable to repeat the rubella test at 16-18 weeks. Comparing old and new tests allows you to obtain more accurate data on the presence/absence of infection and take timely measures necessary to protect the fetus.
Research results
The blood is examined for the presence of antibodies to the TORCH complex - immunoglobulins M and G. The analysis consists of 8 tests that check the presence/absence of immunity to the infections that we described above.
Interpretation of the result is solely a matter for a specialist. In general terms, the test results can be described as follows:
- the presence of only G antibodies (to a specific disease) is evidence of a long-standing infection and the formation of immunity to it; there is no danger for the child and mother;
- Class M antibodies are most often evidence of the acute phase of infection. The level of danger is determined in each case individually, as is the therapy program;
- if antibodies M and G are not detected (for a specific infection), there is no immunity and precautions need to be taken to avoid being infected during pregnancy.
If you do not have immunity to rubella, it is recommended to get vaccinated 3 months before your planned pregnancy. Prevention of toxoplasmosis, one of the especially dangerous infections for pregnant women, will be hygiene. Before pregnancy and during it, you need to avoid contact with cats, including your own and other animals. Any meat must be especially carefully cooked, well boiled and fried; raw meat and surfaces with which it has been in contact must not be touched with bare hands. Just wash your hands as often as possible, do not touch food or your face with unwashed hands.
To protect yourself from herpes, chickenpox, you need to reduce the number of contacts with people if possible, not visit public places (theaters, cinemas, etc.), if necessary - in public transport, clinics, shops - use personal protective equipment (masks, household supplies). hand washing soap and others). Before and during pregnancy, it is not recommended to visit beauty salons, plastic surgery and hardware cosmetology clinics, to have manicures and pedicures done by specialists if you are not sure whether the instruments are disinfected, and to exclude any procedures associated with the risk of hepatitis infection. All of the above causes a lot of inconvenience, but the cost of infection from the TORCH complex is too high to risk the life and health of your child.
What the analysis shows
TORCH tests are classified as indirect diagnostic methods that detect the presence of IgG and IgM antibodies in the blood serum. These are protein formations produced by the immune system to protect against pathogenic microorganisms.
All known antibodies resemble the letter “Y” in appearance, and the “leg” and the adjacent V-shaped part have the same structure, and the shape of the ends of the “fork” is variable. It differs among antibodies designed to protect against different antigens.
IgM antibodies begin to be produced immediately after the onset of the disease. Afterwards, over the course of 1-4 weeks, their number increases, and by the end of the 4th week it reaches a maximum, after which it gradually decreases: this means that the body has already coped with the infection.
IgG antibodies behave differently: at the beginning of the disease they are completely absent. They begin to be produced after 2 weeks from the moment of infection. Their concentration increases more slowly than the concentration of IgM, but they persist longer (sometimes throughout life).
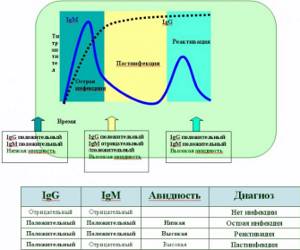
Based on the quantitative ratio of IgG and IgM antibodies, as well as their structure, one can judge:
- whether the woman is currently sick;
- what pathogen caused the disease;
- at what stage the disease is;
- whether she had been ill before or was not infected at all.
There are also direct diagnostic methods that directly determine the presence of the pathogen. This is, in particular, a blood test that will indicate the presence of an infection, but will not be able to identify it and provide all the information necessary to make a final diagnosis.
Where to get tested for TORCH complex infections
The study can be completed in all departments (medical centers and laboratory terminals) of the North-West Center for Evidence-Based Medicine. They are located in St. Petersburg, Leningrad region, and other cities and towns of the Northwestern Federal District.
Find a medical facility near you
You can use the table, the drop-down menu on the left (search by city, metro station), or interactive map. Using the map, you can create a route and find out about traffic jams.
Next to the name of each medical institution of JSC "SZTSDM" a detailed address and telephone number are given. We recommend that you call before visiting the terminal or center to find out when and what tests can be taken.
go to analyzes
Do I need to get tested when planning pregnancy?
TORCH infections are a disease that must be identified if a woman is planning to become pregnant.
Performed approximately 2-3 months before the expected date of conception, the examination makes it possible to:
- obtain complete information about which infections a woman should be wary of;
- get vaccinated in advance, or get recommendations, following which you can minimize the risk of infecting your unborn child;
- in the event of a primary infection, make adjustments to plans regarding future pregnancy.
When planning a pregnancy, it is advisable for the future father of the child to undergo the TORCH test.
Conclusions from the analysis results
Today there are different methods for identifying these infections. Thus, a positive or negative result for syphilis, hepatitis and HIV infection is obtained together with a general blood test, and other pathogens are determined by ELISA or PCR.
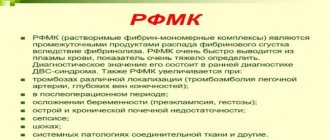
PCR (polymerase chain reaction) allows you to detect even the smallest concentration of the virus in the blood and other secretions (urine and cervical vaginal mucus), but it is impossible to distinguish the acute phase of the disease from the carriage of infection based on the results of this method.
ELISA (Enzyme-linked immunosorbent assay) is more suitable for this. The method is based on identifying immunoglobulins (IgG and IgM) in the blood, which are proteins and are produced as protection after foreign agents (in this case, viruses) enter the body. At the beginning of the disease, IgM appears, and only after 2-3 weeks - IgG, the presence of IgM indicates a recent infection, and IgG indicates the presence of immunity to this pathogen. After the infection leaves the body, IgM also disappears, but IgG is present for life.
There are no specific digital values and norms for TORCH infections; the conventional answer looks like this:
- IgG -IgM — — the infection has never entered the body;
- IgG + IgM — — there was infection, but strong immunity has already formed, so there is no danger;
- IgG-IgM + - the infection entered the body for the first time recently and poses a great threat;
- IgG + IgM + - an infection has been activated in the body, which had already entered it before.
In doubtful cases, an IgG visibility test and immunoblotting can be performed. The methods allow us to more accurately understand when the infection occurred and how strong the immune response was developed. However, studies are expensive and are prescribed as a last resort. Only a doctor can correctly decipher the analysis of TORCH infections. He will identify the risks, prescribe treatment if necessary and tell you how to protect yourself from infection.
Preparation for the event
Preparation for the analysis is quite simple and consists of following a simple diet and temporarily avoiding foods and actions that can distort the test results.
In particular, the patient is offered:
- Stop taking any medications 2 weeks before donating blood. If this is not possible, notify the doctor in advance and obtain all the necessary recommendations from him.
- Stop drinking alcoholic beverages for 3 days.
- Eliminate fried and fatty foods from your diet for 2 days.
- Do not consume any food or drinks other than clean water for 8-12 hours.
- No smoking for 1 hour.
- Take half an hour to rest, relax, calm down.
If you feel unwell, have a high temperature, or feel unwell, the TORCH test will have to be rescheduled to another time.
It is also undesirable to carry it out immediately after execution:
- physiotherapy;
- x-ray;
- any hardware examinations.
Approximate cost in Russia
The TORCH test is a paid service, and the prices charged by medical centers are high. If desired, you can order testing for the presence of antibodies not for all TORCH infections, but for the disease that is most likely. Typically, the price list indicates the prices for each component of the test.
Average cost of a test that detects the presence of antibodies to the virus:
- toxoplasmosis – 490 rub. (IgG) and 660 rub. (IgM);
- rubella – 480 rub. (IgG) and 610 rub. (IgM);
- cytomegalovirus – 510 rub. (IgG) and 610 rub. (IgM);
- herpes – 310 rub. (IgG) and 540 rub. (IgM).
Performing an advanced analysis to determine antibody avidity will be even more expensive.
On average, you will have to pay for a test for resistance to a viral or parasitic infection:
- toxoplasmosis – 1500 rub.;
- rubella – 760 rubles;
- cytomegalovirus – 2400 rubles;
- herpes – 550 rub.
An advanced analysis may be required in the event of a sharp increase in the concentration of IgM antibodies in the blood, detected during simple testing, and the need to clarify whether it is caused by an acute primary infection, re-infection, or activation of viruses that were previously in the latent phase.
Symptoms and signs of TORCH infections
Each of the nosological infectious forms belonging to the TORCH infection group has its own characteristics of infection, course of the clinical picture, impact on health and prognosis for recovery.
Thus, toxoplasmosis is a fairly common pathology with a worldwide population infection rate of 30%. The only possible causative agent of the disease is toxoplasma, which chooses the domestic cat as the primary host for its reproduction, which epidemiologists consider as a source of human infection. Epidemiologists also do not exclude the possibility of transmission of Toxoplasma by contact, which is observed mainly among children. In the case when a person’s immune system functions actively, Toxoplasma infection is not accompanied by the development of clinical symptoms, and after a period of convalescence, persistent protective type-specific immune mechanisms are formed in the human body, preventing the possibility of re-infection.
Rubella, as an infectious viral pathology, also belongs to the group of TORCH infections and differs from the previous nosology mainly by the airborne method of transmission of the pathogen. Rubella is common mainly in pediatric practice and has a favorable course in most situations. The main pathognomonic clinical markers of rubella are small pink exanthema of a common type and febrile fever without a pronounced intoxication syndrome. The danger of rubella lies in the long period of incubation of the pathogen, during which a person is infectious to others. After the end of the convalescent period in the human body, as with toxoplasmosis, persistent immune mechanisms are formed that prevent the possibility of reinfection.
Cytomegalovirus infection is a relatively “young infectious pathology”, since its identification was made only at the end of the twentieth century. The predominant mode of transmission of cytomegalovirus, as the main provocateur of the disease, is sexual and hematogenous, and children are infected through breastfeeding. In individuals who do not suffer from any form of immunodeficiency, cytomegalovirus infection does not provoke the development of clinical symptoms. When the function of the human immune system decreases, cytomegalovirus affects various organs of the human body with the development of polymorphic clinical symptoms. Antibodies produced in the body of a person infected with cytomegalovirus are lifelong.
Herpetic infection is a polyetiological nosological unit, which is due to the presence of several varieties of its causative agent. Herpes of the first type is the causative agent of the so-called oral herpes, that is, all specific clinical manifestations are localized in the perioral area. When infected with herpes type 2, a person exhibits clinical symptoms localized in the urogenital area. In this regard, there are several possible methods of transmission of the pathogen (airborne, contact-sexual, fetoplacental). In severe cases of herpetic infection, a person experiences damage to internal organs, especially the structures of the central nervous system, which is an unfavorable prognostic sign.
Possible consequences of infection
This is a whole complex of ailments that are determined by special tests.
All diseases that are included in the TORCH list are very dangerous and can cause various abnormalities in a newborn. We are talking about problems with internal organs and some physical abnormalities. Experts note that the greatest danger of the disease is in the first 3 months of pregnancy. At this stage, the development of the most important vital organs and systems occurs.
If any factor has a negative impact on them, the consequences will be irreparable
Therefore, it is very important to identify the problem early. It is advisable that existing TORCH infections be identified before conception
If a woman has not undergone an early examination, then a laboratory blood test is mandatory when registering the expectant mother.
The peculiarity of these diseases is not only their relative safety for adults and a great threat to children, but also their modes of transmission.
Infections can pass not only from one partner to another, or from mother to child, but there is a risk of infection through household means or through blood.
If a representative of the fair sex, being at an early stage of pregnancy, takes a test, the results of which turn out to be positive, it is quite possible that a specialist will advise having an abortion.
In such a situation, this will be the best solution, since often the fetus has no chance of survival if there is a TORCH infection. Even in cases where a child is born, he most often turns out to be non-viable. If the presence of infections was determined at a later date, special treatment can be carried out.
However, this does not guarantee that everything will go without complications.
Even the best treatment for TORCH infections in the 2nd half of pregnancy often does not eliminate complications. These include:
- blindness;
- deafness;
- heart diseases;
- mental retardation.