Let's imagine that you are a doctor or paramedic who has been called to provide emergency care. The patient has acute chest pain, shortness of breath, and nausea. Such events will resemble a heart attack, acute heart failure, cocaine abuse, indigestion, etc. [1] You will need to have an electrocardiogram done on site to see the approximate picture. You know that in the event of a heart attack, “time is saved heart muscle, and time spent is lost”! 2 Timely assistance can save the patient’s life and avoid possible consequences. [3] This is where a set of rapid troponin tests can come to the rescue. After pricking the patient's finger, apply a small amount of blood to the test strip. After a few minutes, a test line will appear that is highly likely to indicate a heart attack.
Figure 1 Cardiac troponin is a diagnostic marker for detecting heart attack. Such rapid tests help establish a quick diagnosis. The structural illustrations of the cardiac troponin complex in the figure are derived from the crystal structure of 1J1D deposited in the RCSB PDB. [4, 5]
Myocardial infarction
Myocardial infarction (heart attack or MI) is an acute condition that requires emergency medical attention.[1] Most heart attacks happen suddenly when one of the arteries leading to the heart becomes blocked, usually by a blood clot, cutting off blood flow. Lack of blood blocks the flow of oxygen and nutrients. Without them, heart cells begin to die. When it comes to treating a heart attack, every second counts. Extensive blockage, especially of a large blood vessel, can cause a severe heart attack. If heart disease is not treated early, it can lead to heart failure. Myocardial infarction is caused by a buildup of plaque made from fat and other substances that narrows or hardens the arteries.
Timely diagnosis is paramount for early treatment of MI
Irreversible cardiac damage resulting from coronary artery occlusion can be largely avoided with prompt reperfusion therapy. Reperfusion therapy includes the use of drugs and surgery. Medicines used to treat heart attacks dissolve the clot blocking the artery. Blood flow can be restored surgically by opening the artery at the site of the blockage (coronary angioplasty) or by grafting a new artery around the blockage (coronary artery bypass grafting).[6]
Early diagnosis of acute MI is critical in further treatment. Typical symptoms associated with MI—acute chest pain, often accompanied by upper body pain, shortness of breath, nausea, fatigue, and sweating—are not always observed in every case [7]. Thus, clinical assessment, even in combination with an electrocardiogram (ECG), is often insufficient to diagnose or exclude MI. A blood test to measure the concentration of cardiac troponin (cTn) is an important procedure for the early diagnosis of MI.
Cardiac troponins as diagnostic markers
Troponin is a regulatory protein complex responsible for the functioning of muscle cells. It consists of three subunits: troponin I, T and C (cTnI, cTnT and cTnC). [9] Cardiac muscle cells express cTnI and cTnT isoforms that are structurally different from their skeletal counterparts. In contrast, the cardiac and skeletal isoforms of troponin C are so similar that they are difficult to distinguish by standard diagnostic methods. Blood levels of cTnI and cTnT are usually very low. The death of cardiac muscle cells (myocardial necrosis) leads to the release of cTnI and cTnT into the bloodstream. After a heart attack, the concentration of cardiac troponin (cTnI) in peripheral blood increases 100-fold.
Immunoassays specific for cardiac troponin isoforms may show increased levels in peripheral blood independent of skeletal troponin levels. A number of immunoassays specific for cTnI or cTnT have been developed that meet the same characteristics and do not differ in terms of their diagnostic and prognostic value. cTn (I or T) is the preferred biomarker of myocardial necrosis due to its high-quality performance in the diagnosis and prognosis of cardiac conditions.[6]
Execution technique
Currently, pharmacies offer various rapid tests for detecting heart attacks. A diagnostic kit for the qualitative determination of troponin I or a combination kit that additionally determines myoglobin and creatine phosphokinase, markers of necrosis (death) of the heart myocardium.
This test kit contains:
- hermetically sealed test cassette and test strip;
- pipette for single use;
- scarifier for piercing a finger;
- buffer solution in a vial;
- instructions.
The analysis technique is quite simple; you need to:
- Use reagents and rapid test kit at room temperature.
- Remove the test card-cassette, scarifier and pipette from the packaging, read the instructions to understand the algorithm.
- Wash your hands with soap, dry and warm by rubbing your palms.
- A scarifier needle is used to pierce the lobe; one press on the inner surface of the middle or ring finger is enough.
- Massage your finger towards the edge to form the first drop of blood, then remove it with a cotton swab and alcohol.
- Place your finger over the cassette, but do not touch it, and squeeze the second drop of blood into the center of the rapid test window under the number indicated in the instructions.
- If possible, use a pipette to collect blood.
- Add the buffer solution from the bottle into the window on the cassette under the corresponding letter.
- After carefully putting the test cassette aside, apply a cotton swab with an antiseptic to your finger.
- Wait 15-20 minutes until reaction marks clearly appear in the window on the cassette.
The test must be scored according to the instructions. Standard troponin tests should consider:
- two red marks opposite the control zone with marks of the letters “C” and “T” mean a positive result;
- the appearance of a line opposite the “T” mark of any intensity, even weak, indicates a positive test and the presence of troponin in the blood;
- the only red risk opposite the “C” zone indicates a negative analysis;
- the complete absence of a line opposite o means the test is unsuitable, the deadline has expired, or an error has occurred.
Rapid tests help detect MI earlier than laboratory tests
This rapid test has many advantages for use in diagnosing MI: ease of use, reliability, instrument-free reading, and use of capillary blood taken from a finger prick. However, a key advantage is the ability of RDT to detect elevated cTnI earlier than laboratory testing in certain conditions. In the event of a myocardial infarction, early treatment is critical, which can help avoid extensive damage to the heart. Timely diagnosis is of paramount importance for early treatment of MI. RDT can be used whenever a result is needed before laboratory analysis.
In what cases is a rapid troponin test used?
Prehospital diagnostics
One of the advantages that makes it advisable to use a rapid test for the presence of troponin is that it gives a quicker result than a laboratory - this is the first contact of health workers with the patient. Peripheral blood cTnI levels begin to rise gradually several hours after myocardial infarction and typically peak at 24 to 48 hours, nearly 100 times the baseline level (Figure 2). Serious cases of myocardial infarction, or cases where several hours have passed between the onset of symptoms and contact with health care workers, can be identified at the scene or during transport to hospital. The patient can receive emergency medical treatment and upon arrival at the hospital, the correct treatment will be selected through cardiac imaging and coronary angioplasty.
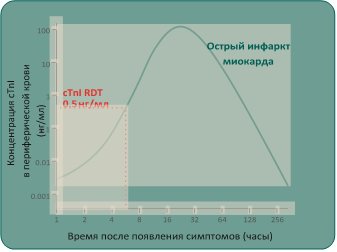
Figure 2 Concentrations of cardiac troponin (cTnI) in peripheral blood increase 100-fold after a heart attack. The cutoff value of this test for diagnosing elevated cTnI is about 0.5 ng/ml. Figure from Mahajan and Jarolin, Circulation, 2011.[11].
It can take several hours for a patient's blood sample to arrive at the central laboratory. In addition, the in vitro cTnI test is associated with a long turnaround time. In contrast, the cTnI test with RDT can be performed on site and the result is known almost instantly. If the result is positive, the patient can be treated immediately.
Crowded emergency room
Overcrowding in hospital emergency departments (ED) is a widely recognized problem that has been shown to lead to increased inpatient mortality.[12] Guidelines from leading heart associations indicate that cTn results should be available to clinicians within 60 minutes of arrival in the emergency department. [13,8] Contrary to these recommendations, even in developed countries, the time from blood collection in the emergency department to receiving the troponin test result is one to two hours. [14] Overcrowding in departments often results in sample processing failures and increases laboratory turnaround times.[15] The cTn test using RDT cTnI can be easily performed by a nurse independently of a central laboratory. By detecting elevated cTnI in a timely manner, RDT can quickly provide important information for medical triage of patients. This can reduce the delay in patient treatment and also reduce the overall workload on the department.
brief information
Rapid tests for the determination of cTnI are easy to use and read the result, reliable, compatible with capillary blood and, above all, give quick results. These features make them ideal for diagnosing myocardial infarction in the prehospital setting. These tests assist in triage in emergency departments. However, the diagnosis of acute myocardial infarction should not be based solely on the results of a rapid test, but should also include the patient's symptoms, ECG and/or angiographic findings. Tests can confirm acute MI, but not rule it out. A negative result on this test with serial blood draws ranging from several hours to several days after the onset of symptoms may indicate a mild form of myocardial infarction or other heart disease.

Figure 3.
Point-of-care versus central laboratory testing for cardiac troponin in patients with suspected heart attack. Point-of-care testing may rule out myocardial infarction earlier than laboratory testing. [16]
References 1. OJ Mechanic and S.A. Grossman, Myocardial Infarction, Acute, StatPearls Publishing, 2021. 2. E. Braunwald, Evolution of the management of acute myocardial infarction: A 20th century saga, vol. 352, Elsevier Limited, 1998, pp. 1771-1774. 3. „Heart attack - your quick guide | BHF,” [Online]. Available: https://www.bhf.org.uk/informationsupport/publications/heart-conditions/heart-attack—your-quick-guide. 4. S. Takeda, A. Yamashita, K. Maeda and Y. Maéda, “Structure of the core domain of human cardiac troponin in the Ca2+-saturated form,” Nature, vol. 424, no. 6944, pp. 35-41, 3 7 2003. 5. “RCSB PDB - 1J1D: Crystal structure of the 46kDa domain of human cardiac troponin in the Ca2+ saturated form,” [Online]. Available: https://www.rcsb.org/structure/1j1d. 6. K. Thygesen, J. S. Alpert, A. S. Jaffe, B. R. Chaitman, J. J. Bax, D. A. Morrow and H. D. White, “Fourth Universal Definition of Myocardial Infarction (2018), “ Journal of the American College of Cardiology, vol. 72, no. 18, pp. 2231-2264, 30 10 2021. 7. R. Twerenbold, J. Boeddinghaus, T. Nestelberger, K. Wildi, M. Rubini Gimenez, P. Badertscher and C. Mueller, Clinical Use of High-Sensitivity Cardiac Troponin in Patients With Suspected Myocardial Infarction, vol. 70, Elsevier USA, 2021, pp. 996-1012. 8. M. Roffi, C. Patrono, J.-P. Collet, C. Mueller, M. Valgimigli, F. Andreotti, J. J. Bax, M. A. Borger, C. Brotons, D. P. Chew, B. Gencer, G. Hasenfuss, K. Kjeldsen and P. Lancellotti, „2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation,” European Heart Journal, vol. 37, no. 3, p. 267–315, 2021. 9. “Troponin - StatPearls - NCBI Bookshelf,” [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK507805/. 10. F. S. Apple, Y. Sandoval, A. S. Jaffe and J. Ordonez-Llanos, “Cardiac Troponin Assays: A Guide to Understanding Analytical Characteristics and Their Impact on Clinical Care,” Clinical Chemistry, vol. 63, no. 1, pp. 73-81, 1 1 2021. 11. V. S. Mahajan and P. Jarolim, “How to interpret elevated cardiac troponin levels,” Circulation, vol. 124, no. 21, pp. 2350-2354, 22 11 2011. 12. B. C. Sun, R. Y. Hsia, R. E. Weiss, D. Zingmond, L. J. Liang, W. Han, H. McCreath and S. M. Asch, “Effect of emergency department crowding on outcomes of admitted patients,” Annals of Emergency Medicine, vol. 61, no. 6, p. 605, 2013. 13. A.H.B. Wu, R.H. Christenson, D.N. Greene, A.S. Jaffe, P.A. Kavsak, J. Ordonez-Llanos and F.S. Apple, “Clinical Laboratory Practice Recommendations for the Use of Cardiac Troponin in Acute Coronary Syndrome,” Clinical Chemistry, vol. 64, no. 4, pp. 645-655, 1 4 2021. 14. C. Ho, K. Cimon, L. Weeks, M. Mierzwinski-Urban, L. Dunfield, L. Soril, F. Clement and M. Jabr, “Point-of-Care Troponin Testing in Patients With Symptoms Suggestive of Acute Coronary Syndrome: A Health Technology Assessment Economic authors: “A Health Technology Assessment, vol. 5, no. 1b, 2021. 15. K. D. Rooney and M. M. Schilling, “Point-of-care testing in the overcrowded emergency department—Can it make a difference?,” Critical Care, vol. 18, no. 1, p. 692, 8 12 2014. 16. A. R. Chapman, S. Stewart and N. L. Mills, Contemporary point of care cardiac troponin testing in suspected acute coronary syndrome, vol. 105, BMJ Publishing Group, 2021, pp. 740-741.
When should you do a troponin test?
Myocardial infarction is an acute, life-threatening condition caused by a circulatory disorder in the myocardium as a result of complete or partial blockage of a coronary artery by a thrombus.
This leads to ischemia and necrosis of part of the heart muscle. Subsequently, the chances of a successful outcome depend on the timeliness of medical care. The myocardial infarction test is performed at the first symptoms of a heart attack:
- pain in the chest and heart area, aggravated at rest, of a compressive nature, with a feeling of squeezing or burning;
- pain in the arm, neck, jaw, on the back in the area of the shoulder blades or between them, discomfort in the abdomen;
- severe weakness and shortness of breath with a feeling of lack of air, fear of death;
- sticky cold sweat, chills, trembling in the arms and legs;
- nausea, vomiting, unstable blood pressure against the background of heart pain and a general progressive deterioration of the condition.
Also, the use of a rapid heart attack test is recommended for patients with angina pectoris, coronary artery disease with frequent attacks of chest pain.
Troponin analysis is used:
- at home, if it is impossible to see a doctor for heart pain;
- when severe pain occurs, in patients with chronic cardiac pathology;
- within 2-4 hours after the first symptoms of a heart attack appear;
- at the prehospital and hospital stage, to confirm the diagnosis.