- Magnetic resonance imaging (MRI)
- Computed tomography (CT, MSCT)
- X-ray studies
- Mammography
- Department of Radionuclide Diagnostics
The examination is performed on a single-photon emission computed tomograph: E. cam Signature (with two detectors), manufactured by SIEMENS (Germany) 2007, with a new software package for the analysis of radioisotope studies (2007). Conducting research and registering for examination: Monday-Friday 9.00 – 15.00 Tel: (495)-942-43-53 (city) Head of department Smirnov Alexander Mikhailovich Radiologist Bugriy Mikhail Evgenievich Senior nurse Markina Irina Petrovna Nurse Dubova Natalia Viktorovna
A distinctive feature of radioisotope research methods is their functionality: the ability to reflect physiological and pathophysiological processes in the organs and tissues of the body in dynamics. High sensitivity – the introduction into practice of modern radiopharmaceuticals, which make it possible to determine the manifestations of pathological processes in the early stages of the disease. Non-invasiveness – the use of indirect diagnostic methods. Low radiation exposure to the patient due to the use of short-lived isotopes. The radiopharmaceuticals used do not cause allergic reactions. Contraindications to performing radioisotope studies: pregnancy, women breastfeeding. The department currently carries out the following studies:
This technique has a number of advantages:
- Versatility when studying a range of diseases.
- Simplicity and speed of execution.
- Minimal possibility of allergic reactions.
- Obtaining maximum information with a single minimum exposure.
- Very low trauma, which is important for weakened patients.
- The uniqueness of the information received.
Thus, it is possible to diagnose both primary tumors and metastases, as well as determine the extent of the tumor process.
It should be noted that the use of the radionculide diagnostic method at the Moscow Center of the Central Clinical Hospital of the Russian Academy of Sciences is one of the safest. All premises are subject to daily radiation and dosimetric monitoring. Patients in adjacent rooms are protected from radiation due to thickened walls, lead-shielded doors and the use of specially equipped containers for storing radiopharmaceuticals. The doses of radiopharmaceuticals used when introduced into the circulatory system are minimal, and the radiopharmaceutical itself is short-lived.
Is treatment with radioisotopes safe?
Strictly speaking, both receptors for prostate-specific membrane antigen and receptors for somatostatin are also present on healthy cells. But on the membranes of malignantly degenerated cells their number is many times greater. This means that the vast majority of molecular complexes with radioactive elements will join these cells. Consequently, the radiation dose received by the tumor will be much higher. This property of radionuclide therapy is called targeting (from the word target, or “goal”), it means high accuracy of the effect on the malignant neoplasm, and not on healthy tissue.
In addition, the types of radiation used during treatment play an important role in the safety of treatment. Lutetium-177 produces beta radiation, while actinium-225 and radium produce alpha radiation. The penetrating ability of beta particles is quite small - they are stopped by only 2–2.5 centimeters of living tissue. That is, this radiation will affect exclusively at the local level. The penetrating ability of alpha particles is even less - it can pass through only 5-10 neighboring cells. This means that the targeting of tumor cells will be as high as possible.
Find out the price
Find out the price
Error! Please fill in all required fields
Thank you! We will contact you shortly
✕
All patients can be divided into three separate categories:
- Category AD. This includes patients who are prescribed studies using radiopharmaceuticals to determine the presence of tumors, their nature or location. In this case, diagnosis is carried out according to vital indications.
- Database category. Studies to clarify the diagnosis in patients who do not have cancer.
- Category VD. Prescribed for patients who need regular examination, including for cancer.
What are the goals of radionuclide therapy?
First of all, the goal of such treatment is to destroy the maximum number of tumor cells in the patient’s body. Reducing the size of malignant foci, as well as destroying individual metastases, then allows one to resort to radical surgery to remove the tumor. In addition, reducing the number of tumor elements has a beneficial effect on the patient’s well-being and alleviates the symptoms of advanced cancer. Reducing the severity of pain and other manifestations is especially important, since radionuclide therapy is usually prescribed in the later stages of the tumor process or when the side effects of chemotherapy are too severe.
Radionuclide diagnostic methods:
There are two options for carrying out such diagnostics: in vivo (with the introduction of radiopharmaceuticals into the body) and in vitro (without administration).
- The first option has restrictions for women with a possible or confirmed pregnancy of the category BD and VD, nursing mothers, and children.
- The second method is safe with respect to radiation and can be used in all patients. In this case, blood or other biological medium and diagnostic test kits are used for analysis.
Depending on the circumstances, radionuclide diagnostics is used, which can be divided into two separate groups:
- Diagnosis without a visual image of the organ affected by the tumor (radiography or radiometry). In the first case, after the administration of radiopharmaceuticals, a special device continuously records changes in organs in the form of curves (radiograms). There are RKG - checking the parameters of the heart; RCH – study of cerebral circulatory disorders; radiopulmonography - testing the function of the lungs and their segments; radiorenography - study of kidney function and radiohepatography - assessment of liver parenchyma and hepatocyte function. In the second case, the amount of accumulated radioactive drug in the organ is recorded in a certain period of time. In this case, radiopharmaceuticals can be introduced into the circulatory system, or a biological medium in vitro can be used.
- Diagnostics with obtaining a visual image of the organ. This technique, in turn, is divided into scanning (scintigraphy) and dynamic scintigraphy. Using a scanner, it is possible to obtain data on the morphological features of organs and systems and their consistent image at all points. When using scintigraphy, a g-camera allows you to quickly (in 30-40 minutes) conduct a study and process the data using a computer. Dynamic scintigraphy expands the study by obtaining not only morphological, but functional data. Information. Obtained from organs during the study is displayed as a series of topograms. Overlapping each other, they give an idea of the dynamic changes in the organ during the passage of radiopharmaceuticals through it. Visual analysis allows you to assess the position of the organ, its size, and areas of change in it. Dynamic scintigraphy also studies the functional characteristics of the organ being studied. This type of research includes radionuclide angiography, hepatobilis scintigraphy, dynamic scintigraphy of individual organs.
DYNAMIC NEPHROSCINTIGRAPHY with indirect angiography
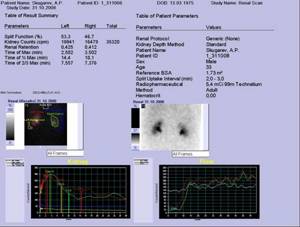
- assessment of renal function (general and separate)
- assessment of renal blood flow velocity and volumetric blood flow visualization of renal duplication, non-functioning kidney, dystopia and nephroptosis, ectopic renal tissue, congenital anomalies, condition of the renal cavity system and ureters
- assessment of patency of the renal arteries (renal artery stenosis)
- diagnosis of vasorenal hypertension
- assessment of acute and chronic renal failure
- severity of renal dysfunction (secretory, filtration and excretory) in pyelonephritis and glomerulonephritis
- determination of the volume of functioning renal parenchyma
- assessment of renal urodynamics (urinary tract obstruction)
- detection of vesicoureteral reflux
Additionally, during the study it is possible to determine the volume of residual urine (men over 40 years old - screening method, prostatitis, prostate adenoma)
No preparation for the study is required. The examination is performed immediately after intravenous administration of radiopharmaceuticals (duration – 30 minutes)
Types of radionuclide diagnostics
Scintigraphy is a modern radiation diagnostic method that is used to assess the functioning of various organs and tissues.
An advantageous difference between scintigraphy and other diagnostic methods is the recognition of the pathological process in the early stages of the disease, i.e. before the disease has time to manifest itself. The advantage of scintigraphy is not only information about the function of the organ, but also obtaining quantitative characteristics of the degree of its damage at the earliest stages. In most cases, scintigraphy does not require special preparation. The use of an innovative gamma camera and radioisotope diagnostics has very high accuracy and efficiency.
The apparatus for radionuclide diagnostics includes a scintillation or gamma camera, which, when absorbing radiation, converts it into electrical signals displayed on a computer screen.
Download brochure Scintigraphy
After the introduction of a radiopharmaceutical into the patient’s circulatory system, the drug selectively accumulates in the organs and is displayed as “hot” zones when it comes to tumors.
There is also a technique where pharmaceuticals that are specific to a specific organ are administered. In this case, the presence of cancer displays them on the screen as a void - a “cold” zone. The presence of metastases gives the same result.
The slice-by-slice images obtained are provided by an innovative SPECT device, which helps to obtain a three-dimensional, three-dimensional model of the organ. In this case, two independent devices (PET and CT) are replaced by a single device with a rotating gamma camera. One or more tomograph detectors move along the patient's body, which makes it possible to study such difficult-to-diagnose areas of the body as the abdominal cavity and chest organs. The scan takes significantly less time compared to a standard study and provides a more complete picture of the disease.
Thanks to radionuclide diagnostics, it becomes possible to study malignant formations of such organs as the thyroid gland, kidneys, liver, lungs, and circulatory system. If bone cancer or metastases are present, skeletal scintigraphy is used. The method is practically safe and can be performed monthly without harming the patient’s health. Such research is very informative. Since, unlike X-ray, it indicates changes in the bones even before signs of their destruction appear.
For tumors of the lymph nodes or diseases of the lymphatic system - lymphography. There are two common methods of procedure: direct and indirect. In the first case, the drug is injected into the lymphatic vessel using an automatic syringe. When lymphogramming hard-to-reach areas (for example, cervical lymph nodes), an indirect lymphogram (administration of the drug intramuscularly) is used. In this case, radiopharmaceuticals do not penetrate into the lymph nodes affected by malignant cells and are not displayed on the computer screen. This allows you to detect metastases and take timely measures by prescribing the correct treatment regimen.
SCINTIGRAPHY OF THE THYROID GLAND
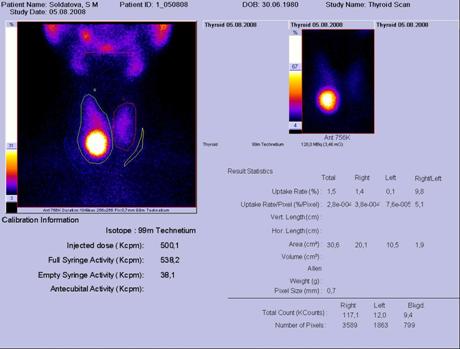
- differential diagnosis of nodular diseases of the thyroid gland
- severity of diffuse changes in the thyroid gland
- dystopia of the thyroid gland
- dynamic assessment of the results of conservative and surgical treatment
No preparation for the study is required. The examination is performed 30 minutes after intravenous administration of radiopharmaceuticals (study duration 20 minutes).
Radioimmunological tests (RIA) for malignant tumors
Radionuclide diagnostics can be indispensable in cases of controversial diagnosis of cancer. Traditional radiographs are often uninformative and indicate the presence of a tumor indirectly. CT scans do not always display the boundaries of the tumor process in detail, and ultrasound diagnostics do not always show rare tumors. The use of MRI, Central Clinical Hospital of the Russian Academy of Sciences, SPECT for some patients is an expensive procedure. This makes it advisable to use radioimmunoassays that provide unique information.
The use of in vitro techniques has its undeniable advantages. It is indispensable for determining the concentration of hormones, immunoglobulins, and tumor antigens in organs. This allows this radioimmunoassay to be used to study diseases such as AIDS, diabetes mellitus, and various forms of severe allergies. Determining the concentration of carcinoembryonic antigen makes it possible to detect oncological pathologies in the early stages.
The principle of radiological analysis (RIA) is to study artificially radiolabeled systems (transport proteins, antibodies, receptor proteins, etc.) obtained from a biological environment. Blood, urine, lymph, etc. can be studied.
Drugs used in radionuclide diagnostics
To successfully conduct a study using radionuclide diagnostics, a combination of three important factors is necessary: high-tech innovative equipment, qualified personnel and high-quality radiopharmaceuticals. The oncology center in Moscow is equipped with the most modern equipment from leading manufacturers. All doctors of the clinic received the highest or first medical category.
All radiopharmaceuticals used in research meet the necessary requirements regarding chemical, radionuclide and radiochemical purity. Ultra-short-lived AFs are used for diagnosis at the Moscow Oncology Center. This eliminates the risk of adverse reactions and complications.
In addition to drugs administered into the circulatory system or lymphatic vessels, radiopharmaceuticals manufactured in the form of tablets are used.
This method has a number of advantages, namely:
- Does not require special storage facilities due to very low radiation levels.
- The risk of radiation exposure for medical personnel and patients is reduced tenfold compared to the use of traditional drugs.
- Radiopharmaceuticals disintegrate and are eliminated from the body in a short time, without causing damage to health.
- The method is atraumatic.
- The use of a new type of radiopharmaceutical does not affect the accuracy and quality of diagnosis.
Carrying out a full range of diagnostic studies along with laboratory tests provide an accurate picture of the development of cancer and help evaluate the methods adopted to combat it.
Non-immunochemical method. Plasma proteins or hormone receptors act as reagents. This method is very accurate, but may be biased if the patient is using stimulants or if there are factors that influence the initial concentration of the hormone or enzyme in the blood.
The Department of Radionuclide Diagnostic Methods of the Central Clinical Hospital of the Russian Academy of Sciences is equipped with a single-photon emission computed tomograph combined with an X-ray computed tomograph, which makes it possible to conduct studies of all human organs and systems.
What types of such therapy exist?
Therapy "Lutetium-177-PSMA"
This treatment is based on the use of a radioactive isotope of the element lutetium. It is used to fight advanced prostate cancer. The therapy is based on the fact that cancer cells of the gland have on their surface a large number of receptors for a special protein - prostate-specific membrane antigen (PSMA). Complexes consisting of the lutetium-177 isotope and PSMA attach with high selectivity to these receptors, which means that the main part of the radiation will affect tumor cells.
Therapy "Lutetium-DOTATAT"
The principle of action of this treatment method is similar to Lutetium-177-PSMA therapy, only here the target is cellular receptors for the hormone somatostatin. They are present in large quantities on the cell membranes of neuroendocrine tumors of the gastrointestinal tract and pancreas.
Actinium-225-PSMA therapy
This method is based on the same principles as the Lutetium-177-PSMA therapy, and is also designed to destroy cancer cells in the prostate gland with radioactive radiation. The difference here is the use of another radioisotope - actinium-225. If lutetium-177 during decay emits beta particles, that is, high-energy electrons, then actinium-225 during decay emits alpha particles - helium nuclei. Actinium-225-PSMA therapy is used in cases where the patient does not demonstrate a good response to radionuclide treatment with lutetium-177.
Radium therapy
It is based on the natural radioactivity of this element, which produces alpha radiation, and in the human body behaves like calcium. This means that more than 80% of the radium that enters our body accumulates in the bones. And therefore, it is convenient to use it for local radiation effects on metastases of malignant tumors in bone tissue.