- What is bone radiography?
- In what areas is bone radiography used?
- How should you prepare for research?
- What does the diagnostic equipment look like?
- What is the basis for the research?
- How is the research conducted?
- What should you expect during and after the procedure?
- Who reviews the X-ray results and where can they be obtained?
- What are the benefits and risks of bone x-rays?
- Limitations of X-ray bone examination
Bone sarcomas treatment stages 1, 2, 3. Symptoms, signs, metastases, prognosis.
Content:
- General information about the origin of bone sarcomas
- What are the different forms of bone cancer? Osteosarcoma
- Ewing's sarcoma
- Chonrosarcoma
- Examination methods before prescribing treatment
- Surgery
General information about the origin of bone sarcomas
Bone cancer includes a group of neoplasms with different clinical characteristics (from extremely slowly developing to rapidly growing and early metastasizing tumors).
Bone sarcomas can be localized in any bones of the skeleton. However, the long bones most commonly affected are the femur, tibia, and humerus. Less commonly affected are the pelvic bones, scapula and ribs.
Secondary (metastatic) bone tumors occur in clinical practice much more often than primary ones. In this case, metastases mainly affect the vertebrae, ribs, pelvic bones, etc.
The most common cancers that metastasize to bone are breast, lung, prostate, kidney, and thyroid cancers.
How is an X-ray examination of bones performed?
The radiologist (a doctor who specializes in X-ray examinations) or nurse helps the patient onto the table and places the X-ray film or digital imager in a special compartment under the table at the level of the part of the body that needs to be imaged.
If necessary, sandbags, pillows, or other devices may be used to maintain the patient's position. To protect tissues from radiation, a lead apron is placed on the pelvic area or mammary glands.
You should remain as still as possible and hold your breath for a few seconds during the photo itself, which reduces the likelihood of blurring the image. When the X-ray machine is operating, the doctor moves towards the wall or leaves the treatment room into an adjacent room.
After the initial image, the doctor may ask the patient to change body position, after which the procedure is repeated. When examining joints (knee, elbow, wrist), 2-3 photographs are usually taken from different angles.
For comparison, a photograph of a healthy limb is also often taken, and when examining children, a photograph of the growth zone of bone formation on the opposite side is taken.
After the examination is completed, the radiologist asks the patient to wait until the images are analyzed, as additional series of images may be required.
An x-ray examination of bones generally takes about 10 minutes.
Up
What are the different forms of bone cancer?
Osteosarcoma
One of the most common forms of malignant bone tumors. The tumor usually occurs in children, adolescents, and young people, somewhat more often in men than in women. Osteosarcoma can develop in any bone of the skeleton, but its favorite location is long tubular bones and especially the lower extremities, mainly forming the knee joint.
Clinically, two forms of osteosarcoma are distinguished: rapidly developing tumors with an acute onset of the disease, severe pain, and more slowly developing tumors with less pronounced clinical manifestations. With rapidly growing forms of the tumor, detection of pulmonary metastases is possible during the initial examination.
Osteosarcoma differs from other bone sarcomas in its aggressiveness. This is evidenced by its tendency to rapid growth and early hematogenous metastasis. Metastases usually clinically manifest themselves 6 to 12 months after the appearance of the first signs of the disease. The lungs are most often affected by metastases.
Ewing's sarcoma (bone marrow tumor)
It ranks second in incidence among malignant bone tumors that occur in adolescence and childhood age groups.
The tumor most often develops in the second decade of life and is quite rare in children under 5 years of age. Boys get sick more often. In contrast to osteosarcoma, Ewing's sarcoma is more likely to affect the diaphysis of the bone, as well as flat bones, including the pelvis, scapula, ribs, and vertebral bodies.
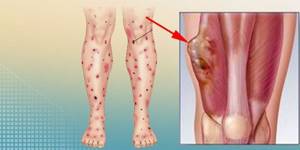
The most favorite localization of Ewing's sarcoma is the long tubular bones of the extremities and pelvic bones. The clinical picture of Ewing's sarcoma, along with the appearance of pain in the affected bone, is often characterized by the presence of fever, leukocytosis and accelerated ESR. Local hyperemia of the skin is noted.
Ewing's sarcoma leads to rapid bone destruction, spreads along the bone marrow canal, grows into surrounding tissues and early metastasizes to the bones, lungs, liver and other organs. Metastases to the lymph nodes are observed in up to 20% of cases.
Chonrosarcoma is a primary malignant bone tumor of cartilaginous nature.

In adults, chondrosarcoma is the second most common type of bone cancer after osteosarcoma. In the structure of primary bone tumors, chondrosarcomas occupy 10-20%. They can also arise as secondary tumors as a result of malignancy of benign osteochondromas or enchondromas. The tumor usually occurs in people over 40 years of age, and develops somewhat more often in men.
Chondrosarcomas can affect any bone of the skeleton, but the predominant tumor sites are the pelvis and femur. Often, chondrosarcoma develops in flat bones such as the shoulder blade, ribs, pelvis and skull. The clinical course of hondrosarcomas is relatively slow, but fast-growing variants of the disease are also found.
Metastases of chondrosarcoma develop at a relatively late stage. The clinical picture is characterized by pain in the affected area. When the pelvic bones are affected, the symptom complex includes a picture of involvement of the nerve roots, consisting of pain and dysfunction of the pelvic organs.
Side effects of osteoscintigraphy
A bone scan involves the use of a radiotracer, most commonly technetium −99m, which is injected into the blood. The radiation level of the radioactive tracer is very low, much lower than that of a CT scan. The radiopharmaceutical is quickly eliminated from the body: after 1-2 days it completely leaves the body. Therefore, there are no radiation-related side effects.
There is a small risk of an adverse reaction caused by technetium-99m. After administration of the drug, the patient may experience:
- soreness or redness at the injection site;
- feeling of a strange taste in the mouth;
- chest pain or discomfort;
- cardiopalmus;
- change in odor perception.
These side effects occur in only 1% of patients. In most cases, they soon go away on their own without treatment.
Statistics
Malignant bone tumors in the structure of cancer incidence account for approximately 1% of all malignant neoplasms. Primary malignant bone tumors occur at any age, but most often between 15 and 40 years of age.
According to some authors, children, adolescents, and young people most often fall ill, especially in adolescence and young adulthood (up to 20 years).
Among malignant bone tumors, osteosarcoma is the most common (50-60%), followed by Ewing's sarcoma, followed by chondrosarcoma, fibrosarcoma, etc.
In some patients, malignant tumors develop as a result of malignancy of benign and tumor-like formations.
Over the past ten years, from 90 to 140 cases of malignant bone tumors have been registered annually in Belarus.
Risk groups and factors predisposing to the development of bone sarcomas
The reasons for the development of bone tumors are not well understood. Often tumors develop after injury. However, nowadays they tend to believe that trauma simply draws attention to an already existing tumor and does not play a significant role in the etiology of the disease, but contributes to its rapid growth.
Sarcomas can develop in bone that has previously been exposed to ionizing radiation for the treatment of other malignancies. Radiation-induced bone sarcomas usually develop at least 3 years after irradiation.
Prevention and early detection of bone sarcomas

There is no specific prevention of bone tumors. Processes prone to transformation into malignant bone tumors include fibrous degeneration, chondromas, osteochondral exostoses and Paget's disease (deforming osteosis). According to various authors, the frequency of their malignancy can reach 15%.
Treatment of precancerous bone diseases is surgical. In case of multiple bone lesions, it is necessary to undergo annual follow-up examinations with an orthopedic traumatologist for early detection of malignancy.
Diagnosis of bone cancer
The leading method for diagnosing bone cancer is x-ray examination.
The most significant radiological signs of a malignant tumor are:
- the presence of a focus of bone destruction (destruction);
- the presence of a periosteal reaction in the form of a characteristic visor, long thread-like spicules located perpendicular to the bone, appearance next to the affected bone, as well as a soft tissue component with areas of calcification.
Examination methods before prescribing treatment
The diagnosis of bone sarcomas is established on the basis of morphological examination of a tumor fragment obtained by biopsy and x-ray examination.
Tumor biopsy can be performed by trephine biopsy (removal of tumor material using a thick needle, including under X-ray guidance) or open biopsy.
It is mandatory to perform an X-ray of the entire affected bone, as well as a CT or MRI. These studies may be repeated during chemotherapy to evaluate its effectiveness.
To clarify the extent of the tumor and develop optimal treatment tactics, an instrumental examination is carried out:
- CT scan of the chest;
- ultrasound examination of the abdominal organs;
- osteoscintigraphy;
- bone marrow biopsy (for Ewing's sarcoma).
How should you prepare for research?
In most cases, bone x-rays do not require any preparation. During the examination, you will need to remove some or all of your clothing and wear a special hospital gown. In addition, you should remove all jewelry, glasses, dentures, and any metal or clothing that could interfere with the x-ray image.
Women should inform their doctor and radiologist of any possibility of pregnancy. As a rule, X-ray examinations are not performed during pregnancy to avoid exposure of the fetus to radiation. If x-rays are necessary, special precautions should be taken to protect the developing child.
Up
Stages of bone sarcomas
The classification is used for the most common bone tumors (osteosarcoma, Ewing's sarcoma, chondrosarcoma, etc.). The stage is established on the basis of histological examination and instrumental examination data (radiography, osteoscintigraphy, etc.).
- Stage I All low-grade tumors without metastases;
- Stage II All high-grade tumors without metastases;
- Stage III All tumors without metastases with the presence of several foci in one bone;
- Stage IV All tumors with the presence of metastases in distant organs and/or regional lymph nodes.
Who reviews the X-ray results and where can they be obtained?
The images are analyzed by a radiologist: a doctor who specializes in performing x-ray examinations and interpreting their results.
After examining the images, the radiologist draws up and signs a report, which is sent to the attending physician. In some cases, the report can be collected from the radiology department itself. The results of the study should be discussed with your doctor.
A follow-up examination is often required, the exact reason for which will be explained to the patient by the attending physician. In some cases, additional examination is carried out when doubtful results are obtained that require clarification during repeated images or the use of special imaging techniques. Dynamic observation allows timely identification of any pathological abnormalities that arise over time. In some situations, repeated examination allows us to talk about the effectiveness of treatment or stabilization of tissue condition over time.
Up
Treatment methods for bone cancer
Currently, the principles of treatment of some types of malignant bone tumors have undergone significant changes. Radical surgical interventions can be independent methods of treatment exclusively for highly differentiated (low-grade) tumors (chondrosarcoma, fibrosarcoma, parosteal sarcoma).
Treatment of low-grade (high-grade) tumors (osteosarcoma, Ewing's sarcoma, etc.), given their high tendency to hematogenous metastasis, involves long courses of chemotherapy after surgery to prevent the development of metastases or treat them. In the treatment of radiosensitive bone tumors (Ewing's sarcoma, bone lymphosarcoma), radiation is used, which in combination with chemotherapy can cure the tumor without surgery.
Surgery
Surgical intervention is the main component of almost any complex of therapeutic measures for bone tumors. Radical operations for bone sarcomas include amputation, disarticulation and organ-preserving operations.
Amputations and disarticulations are performed in cases of advanced tumor process (tumor decay with severe intoxication, bleeding from eroded great vessels, pathological fractures with severe pain).
Extended radical operations include interiliac-abdominal dissection and interscapular-thoracic amputation, which can be used for low-grade tumors with a more favorable prognosis in cases where organ-preserving treatment is not possible.
For tumors affecting the bones of the extremities, preference is given to organ-preserving operations using individual endoprosthetics, as well as bone grafting, including microsurgical autologous bone transplantation.
Contraindications to organ-preserving surgical interventions are: involvement of the main neurovascular bundle in the tumor process over a large extent; pathological fractures with infection and seeding of tissues with tumor cells; extensive tumor damage to muscles.
Radiation treatment
Radiation therapy for malignant bone tumors is rarely used, with the exception of treating Ewing's sarcoma and bone lymphoma. Sometimes radiation treatment is used when it is impossible to remove the tumor or its metastases.
Chemotherapy
Chemotherapy is widely used in the treatment of high-grade bone tumors.
The goal of chemotherapy before surgery (neoadjuvant chemotherapy) is to target micrometastases and reduce tumor size.
Another advantage of neoadjuvant chemotherapy is the ability, based on the response of the tumor to preoperative courses of treatment, to determine its sensitivity to the drugs used and, if necessary, to change the treatment regimen after surgery.
The goal of postoperative chemotherapy is to suppress the growth and destroy microscopic metastases (adjuvant chemotherapy) or treat distant metastases that have already developed (curative chemotherapy).
Typically, four to 10 courses of postoperative chemotherapy are given, depending on the type of tumor.
In the treatment of osteosarcoma, the highest effectiveness has been established for combinations including doxorubicin, cisplatin, ifosfamide, and methotrexate. In the treatment of Ewing's sarcoma, combinations of doxorubicin, vincristine, ifosfamide, dactinomycin, etoposide and cyclophosphamide have proven themselves well and are widely used.
If chemotherapy is effective and there are single metastases in the lung, surgical removal is possible.
Observation and examination after treatment
For high-grade sarcomas, follow-up examinations with an oncologist are carried out:
- during the first two years after completion of treatment - every 3 months;
- during the third year - every four months;
- during the fourth and fifth years every 6 months. and further – annually.
For low-grade sarcomas, observation is carried out every 6 months. for 2 years and then annually.
Follow-up examination after completion of treatment includes:
- MRI/CT of the bone affected by the tumor;
- CT scan or chest x-ray;
- osteoscincigraphy;
- Ultrasound of the abdominal organs.
What does the diagnostic equipment look like?
Bone x-ray equipment includes an x-ray tube suspended above the patient's table. The drawer, which is located under the table, contains X-ray film or a special photographic plate for obtaining images. In some cases, radiography is performed with the patient in an upright position, for example when examining knee joints.
A portable (portable) X-ray machine is a compact device that allows you to examine a patient directly in the intensive care unit or in a hospital bed. In this case, the X-ray tube is attached to a flexible arm, which is placed above the patient's body, while the photographic plate or X-ray film holder is placed behind the patient's body.
Up
Prices for treatment of bone sarcoma in Belarus
| Type of medical research | Amount, BYN |
| X-ray computed tomography of the spine with contrast enhancement | 501,00 |
| X-ray computed tomography of bones and joints without contrast enhancement | 298,00 |
| Ultrasound of the abdominal cavity and retroperitoneal space using the SMI method | 103,00 |
| Skeletal scintigraphy (profile scan) with Tc99m-MDP | 242,93 |
| SPECT/CT of the skeleton with Tc99m-MDP | 571,02 |
| Consultations with medical specialists (depending on qualifications) | 75,00-186,00 |
*Prices are indicative, because Payment for services is made in Bel. rub.
*You can view all types of services and exact prices on the page
Preparing for bone scintigraphy
Osteoscintigraphy does not require special preparation. Before the test, you can eat as usual and take all prescribed medications. If a scan of the hip or pelvis is required, you will need to empty your bladder and bowels before the scan. This is necessary to obtain clearer images.
You must come to the examination in loose clothing that does not restrict movement. It is also worth bringing your medical record with you, as well as pictures or disks with the results of previous diagnostic imaging tests (X-ray, CT, MRI). This information may be helpful in interpreting the results.