Ultrasound examination of organs and tissues is carried out using ultrasonic vibrations. In the process of passing between the boundaries of tissues of different thicknesses, sound reflection does not occur in the same way. The sensor, which performs the function of receiving the reflected echo signal, converts them into graphic symbols, which are subsequently recorded on the device’s monitor and, if desired, printed on special photographic paper.
The huge advantage of this method is that it has absolutely no contraindications; it can be performed as many times as necessary to monitor the course of the disease or diagnose. Even if necessary, it is allowed to do an ultrasound a couple of times a day.
Difficulties in conducting the study or it may not be informative due to the presence of dense scars in the patient after surgery, excess body weight, and flatulence.
History of ultrasound
Ultrasonic vibrations were discovered by Italian scientist Lazzaro Spallanzani back in 1794. While watching the bat, he wondered how it was possible to navigate in space at night while flying. It turned out that this is carried out using high-frequency sound vibrations, inaudible to humans. But animals, particularly bats, perceive them very well. The principles of echolocation are also used by marine animals - killer whales, dolphins, whales, etc. Over time, they became known as ultrasonic waves.
In 1942, for the first time, the German doctor Theodor Dussick and his brother, scientist and physicist Friedrich Dussick, tried to use ultrasound to diagnose a tumor in a patient’s brain. The first medical ultrasound device was created in 1949 by the American scientist Douglas Haury.
Doppler Christian Anders made a great contribution to the development of ultrasound diagnostics. While working on his scientific work “On the collometric characteristics of the study of double stars and some other stars in the sky,” he noticed that the frequency of the signal reflected from an object depends on its speed and direction of movement. This property is called the Doppler effect, which is widely used in Dopplerography to examine blood flow parameters.
Forecast
The prognosis depends on the time of initiation of therapy; the earlier it is started, the more favorable the prognosis. As for the psychomotor development of children with congenital hypothyroidism , this depends on the age at which treatment was started and the correct dose of drugs. If treatment is carried out from the first month of life, children develop normally, but they need to take the drug for life. Myxedematous coma hypothyroidism is untreated , is an extremely severe and often fatal condition. Mortality reaches 75%.
What is the thyroid gland?
The thyroid gland, or “thyroid” for short, is a gland that is part of the endocrine system (a system for regulating the functioning of internal organs with the help of hormones that secrete endocrine cells into the blood) that stores iodine and secretes hormones containing iodine.
Regulates metabolism, cell growth and the growth of the entire organism in general. The thyroid gland is located in the neck in front of the trachea under the larynx. It looks like a butterfly located on the surface of the cartilage. If there are changes in the functioning of the thyroid gland, the patient will feel unwell (this may indicate an incipient disease), and later various complications may arise. The method of ultrasound examination of the thyroid gland will help to effectively identify incipient diseases.
If the thyroid gland does not function properly, the following pathologies may appear:
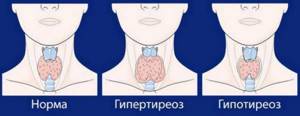
- hyperthyroidism – excessive activity of the gland;
- hypothyroidism – low activity of the gland, characterized by a reduced level of hormones produced;
- cancer;
- cyst;
- benign formations;
- thyroiditis is an inflammatory disease of the gland;
Pathogenesis
In developmental disorders (dysgenesis) of the thyroid gland, genetic factors (mutations of genes encoding transcription and thyroid hormones) and environmental factors play a role. It has been established that three transcription factors are involved in the formation of this organ: PAX-8, TTF-1 and TTF-2. The role of TTF-1 in agenesis/hypoplasia has been shown; TTF-2 is involved in gland morphogenesis. TTF-2 and PAX-8 regulate thyroglobulin and thyroid peroxidase .
Gland hormones affect the development of the body. T3 is more metabolically active. Hormones regulate growth, development and differentiation of tissues. They stimulate the secretion of growth hormone and have an anabolic effect on protein metabolism. They take part in the development of bones and muscles, enhance the release of fat from the depot, stimulate hematopoiesis and myelination of nerve fibers, increase the excitability of the central nervous system, regulate reproductive function and activate mental processes.
Lack of hormones disrupts the growth and development of a child’s body. The biosynthesis and breakdown of proteins slows down. The basal metabolism decreases. Mucopolysaccharides accumulate in tissues and fluid is retained in tissues and cavities (mucoedema - myxedema ). The absorption of glucose decreases, its use by cells slows down, and a tendency to hypoglycemia appears. With a deficiency of T3 and T4, the synthesis of somatotropic hormone .
Ultrasound of the thyroid gland
, an ultrasound diagnosis of the thyroid gland should be performed . This procedure is invasive, fairly cheap, fast and provides accurate results.
Ultrasound is a study of the body using ultrasonic waves. The echo signals reflected from the internal organs, after certain transformations, create on the monitor screen an image of a section of the gland in different shades of gray.
A specialist can determine the condition of the organ: geometric dimensions, state of borders, lymph nodes, blood vessels. Ultrasound determines the acoustic density of an organ, called echogenicity.

May be:
- normal;
- reduced;
- increased;
- echonegativity.
The condition of the organ being studied is determined by the types of echogenicity.
Reduced (hypoechogenicity) is characteristic of liquid formations (dark gray areas on the screen). Perhaps it is a cyst, liquid formations, vascular formations and cancer in 5% of cases. A doctor cannot always reliably determine the nature of these formations, so other diagnostics, such as a biopsy, will be required.
Increased (hyperechogenicity) indicates a lack of iodine (endemic goiter), damage to the organ by poison (toxic goiter), autoimmune thyroiditis, subacute thyroiditis, oncology, areas of sclerosis. Visualized on the monitor as white spots. Hyperechogenicity may occur in a healthy gland, or it may indicate serious pathologies, therefore, to obtain a reliable diagnosis, it is advisable to conduct additional research.
Echonegativity (anechoicity) is displayed as black areas. Perhaps it is a cyst, pseudocyst, colloid cyst, adenoma. It is also recommended to undergo other examinations to make a more accurate diagnosis.
With normal echogenicity, the silhouette of the gland is smooth and clear. A benign tumor has smooth edges, while a malignant tumor has curved edges.
Since the frequency of ultrasound is not high, there is no harmful effect on the body.
Diet
Diet for hypothyroidism of the thyroid gland
- Efficacy: therapeutic effect after 3 weeks
- Timing: constantly
- Cost of food: 1480-1660 rubles per week
Diet 8 table
- Efficiency: weight loss to the required level
- Time frame: long-term, until the expected effect is achieved
- Cost of products: 1120 - 1230 rubles per week
Proper nutrition helps to improve gland function to some extent. In iodine-deficient areas, the menu must include foods rich in iodine: seaweed, sea fish (sea bass, cod, tuna, salmon, horse mackerel), squid, shrimp, vegetables and fruits (radish, lettuce, beets, cabbage, apricot, pumpkin), beans, durum wheat, powdered eggs, powdered milk, and also use iodized salt.
Nutritional therapy for hypothyroidism is aimed at weight loss. To do this, it is necessary to reduce the energy value of the diet and speed up metabolic processes through active sports. Even with normal weight, taking into account the decrease in the rate of metabolic processes, the energy value of the diet is reduced to 2200 Kcal due to carbohydrates and fats. Protein products in the diet should be present in sufficient quantities (100 g/day from lean meat, cottage cheese, eggs, fish and seafood), as they speed up metabolism. The meals are fractional, which also helps speed up metabolic processes. Frying is excluded from culinary processing, since the calorie content of a fried dish increases significantly.
When losing weight, Table No. 8 , the energy value of which is reduced to 1700-1800 Kcal, and salt consumption is also reduced. In this case, you need to drink enough liquid. To feel full, it is recommended to introduce foods with a large amount of dietary fiber (bran, raw vegetables, unsweetened fruits, grain breads). Considering that patients have a tendency to constipation, the diet should include plums, prunes, apricots, raw beets and bran.
How to prepare for an ultrasound
The method is accessible and simple, does not require special preparatory operations. You can eat absolutely any food product. But there are a number of restrictions:
1. Regardless of the feeling of nausea, older people are not recommended to eat before the procedure. Age-related changes may have an effect.
2. Women are recommended to undergo examination on days 7-9 of the menstrual cycle to avoid inaccurate results.
3. Immediately before the procedure, you need to free your neck from elements that interfere: jewelry, collars, etc.
4. Preparation for an ultrasound examination of the thyroid gland in children is no different from the procedure for adults. The child must be psychologically prepared for the procedure so that he is not afraid of either the doctor or what he will do.
Doctors recommend that women undergo testing both during pregnancy and at the planning stage. If it is impossible to get pregnant, gland pathology may be one of the possible causes.
After the child has suffered stress, it is also worth going to the clinic so that an endocrinologist can perform an ultrasound of the thyroid gland.
Prevention
The health of a pregnant woman and compensation for hypothyroidism , if a woman suffers from it, is the prevention of thyroid hypotrophy and congenital hypothyroidism in a child:
- taking prenatal vitamins and iodine supplements;
- healthy eating;
- physical activity;
- regular observation in the antenatal clinic;
- adequate treatment in case of hypothyroidism.
A healthy and active lifestyle in old age, treatment of chronic foci of infection, proper nutrition, yoga, maintaining a normal weight, taking vitamin-mineral complexes and antioxidants - these are the components that will help prevent rapid aging of the body and atrophy of the thyroid gland. If this happens, it is important to compensate for the developed hypothyroidism to improve the quality of your life.
How is the procedure carried out?

The patient lies down on a special couch with his head thrown back, a soft pillow or cushion is placed at the level of the shoulder girdle. A gel that conducts ultrasound well is applied to the neck in the area of the thyroid gland. An ultrasound transducer is applied to the neck and ultrasonic waves are emitted. The sensor is a transceiver that emits and receives a reflected echo signal. This information is processed by a computer and the result is displayed on the monitor. During the procedure, the patient does not experience any discomfort; sometimes there may be slight discomfort due to incorrect body position.
Consequences and complications
Atrophy of the gland in adults leads to sexual dysfunction; if conception occurs, there is a risk of having a child with gland pathology.
Hypoplasia of this organ is most dangerous for children - even congenital cretinism . Its cause is not only hypoplasia , but also an enzyme defect, which disrupts the biosynthesis of hormones at different stages - from iodine absorption to the synthesis of T3 and T4. Hypothyroid cretinism is characterized by mental retardation up to idiocy. At the same time, physical development is also disrupted and there is a disproportionate development of the body - a short neck, arms and legs, a large head, a large protruding belly. Such children have poorly developed sexual characteristics.
In children, but more often in adults and adolescents who do not take treatment, it is possible to develop severe hypothyroidism - myxedema . Myxedema is characterized by mucous swelling involving the skin and subcutaneous tissue, decreased intelligence, slowed thinking, lethargy, sluggishness, constant drowsiness , memory impairment, aseptic polyserositis (accumulation of fluid in body cavities) and depressive states . The appearance of patients is characteristic - coarsening of features and puffiness of the face, its mask-like appearance, swelling around the eyes, low and rough voice.
, hypothyroid coma may develop . A feature of this coma is a significant decrease in body temperature to 23-240C. Hypothermia is a consequence of low basal metabolic rate. Patients develop severe bradycardia and arterial hypotension (even collapse ), respiratory failure and increasing hypoxia and acidosis .
Interpretation of ultrasound results
The diagnostician describes the results obtained in the study protocol. Typically, the time to prepare a written report does not exceed 15 minutes.
Determination of exact geometric dimensions
The location of the gland will normally be typical or low, the shape will be classic, the contour will have a clear outline. It consists of two lobes with an isthmus that connects them. Sometimes a pyramidal lobe may be present.
Minor (less than one centimeter) tissue growths may be visible. If during the period of intrauterine growth the gland develops with pathology, the tissue may not be divided into two sides, but may move to one side. This is called aplasia of one lobe.
In the case of a completely undeveloped gland, they speak of complete aplasia. The length of the lobe should be from 4 to 6 cm, width from 1.3 to 1.8 cm, thickness from 1.5 to 1.8 cm; the shares are normally the same; the lintel has a thickness of 4 to 8 cm.
The volume of a healthy gland depends on the patient’s weight and is:
- weight 50 kg, gland volume 15.5 cm³
- weight 50-60 kg, volume 18.7 cm³
- weight 60-70 kg, volume 22 cm³
- weight 70-80 kg, volume 25 cm³
- weight 80-90 kg, volume 28.4 cm³
- 100 kg or more, volume 32 cm³
Non-compliance with standard sizes will indicate possible pathologies.
Definition of structure
The echogenicity of a healthy thyroid gland, without any peculiarities, the structure of the jelly tissue is fine-mesh, homogeneous, echogenic granularity is 1 mm or less. Fibrous and connective tissues are not detected. In inflammatory processes, the structure is heterogeneous.
Focal education. There should be no new growths. If the formation is present, it must be classified. If the size is up to 10 mm, then it is a focal formation, more than 10 mm, then it is a node.
Blood flow analysis. The parameters of blood flow, its nature and density, and parameters of the lymph nodes are determined. Normal nodes have clear boundaries, the width is approximately 2 times less than the length.
Contours. Clear contours are the norm. Fuzzy outlines indicate an inflammatory process or tumor.
Focal formations. Assessed for the presence of nodes, cysts, and calcinitis.
Echogenicity is the grayscale image of the tissue being examined and its tone on a monitor.
Parameters of visible lymph nodes (if present), their structure, size, structure. By their presence, the onset of tumor formation can be diagnosed.
The structure of the salivary gland and the level of response to ultrasound.
The size and structure of the soft tissues of the neck and larynx. Those areas that are located near the thyroid gland are examined.
Women over 35 years of age are recommended to have their thyroid gland examined at least once a year. This category of people is at risk for thyroid diseases.
The human neck is quite complex; it contains many nerve trunks and large vessels, the esophagus, trachea, many lymph nodes, and other glands. Therefore, the specialist performing the ultrasound procedure must be highly qualified.
The doctor conducting the research records the data obtained in a special protocol, which describes the geometric parameters of the lobes and isthmus, calculates the volume of the gland, and writes a conclusion.
The document evaluates the position and contours, tissue structures, analyzes the parathyroid glands and lymph nodes, and the images taken are also attached to the protocol. In case of normal indicators, a corresponding entry is made in the document. This takes no more than 10 minutes.
Hypoplasia in children
Differentiation of the fetal thyroid gland begins at week 7 of embryogenesis and takes four weeks. Structural changes consist in the formation of follicular cells and the functional unit of the gland - follicles. Rapid follicular growth begins and thyrocytes are able to synthesize hormones from the 12th week. By this time, the fetal thyroid gland can already accumulate iodide and synthesize hormones. The activity of the fetal gland is affected by iodine, which enters the pregnant woman’s body and is the main component of hormones. In this regard, it is important to promptly identify iodine deficiency during pregnancy and prescribe iodine supplements. This ensures the normal course of pregnancy and the birth of a healthy child.
The developing fetus requires a high iodine intake, so during pregnancy there is a risk of developing physiological iodine deficiency. Compensation for hypothyroidism in a pregnant woman is important, since it and iodine deficiency are the main causes of glandular hypotrophy in a child and congenital hypothyroidism. Pregnant women with hypothyroidism in 56% of cases give birth to children with hypoplasia of the thyroid gland.
Congenital hypothyroidism is the main cause of growth retardation and mental development. If treatment for hypothyroidism begins in the first month after birth, normal psychomotor development of the child can be expected. Without timely treatment, children become mentally retarded and have short stature. This is due to the fact that low levels of thyroid hormones in the first months of the child lead to a delay in the myelination of nerve fibers, the accumulation of lipids in the nervous tissue decreases, and structural disorders occur in neurons. In the case of congenital hypothyroidism, the growth of children is inhibited (thyroidism).
Signs of congenital hypothyroidism:
- high birth weight;
- late loss of the umbilical cord;
- weakened sucking;
- swelling of the tissues (the tongue does not fit in the mouth);
- bloating;
- tendency to constipation ;
- prolonged jaundice;
- rough voice;
- drowsiness;
- low mental activity;
- slow reactions;
- muscle hypertonicity;
- cold hands and feet.
If the disease is not compensated by taking hormones in the second or third month, a detailed picture of hypothyroidism develops: trophic changes in the skin, lethargy, adynamia , bradycardia , pale skin, persistent constipation, impaired psychomotor skills and attention . In the future, hypothyroidism in delayed physical and mental development: the child begins to walk late, the fontanelle closes late, and the timing of teething is delayed. Thyroid dwarfism is characterized by the fact that the body proportions are close to chondrodystrophic. Due to a pronounced disturbance in the metabolism of glycoproteins, swelling of the subcutaneous tissue develops and weight increases. The face becomes puffy, the tongue becomes large and thick, and the palpebral fissures narrow.
Disturbances occur in all systems: the heart enlarges, the pulse slows down, blood pressure decreases significantly, constipation and bloating , liver and kidney function decreases. If treatment is not started in the first weeks of life, irreversible changes in the central nervous system occur (mental retardation and decreased intelligence).
Screening for congenital hypothyroidism allows you to diagnose it in the first days of life, begin treatment and avoid serious consequences. For early detection of congenital hypothyroidism in newborns, the TSH level is checked on days 4-5, and it should not be higher than 20 µU/ml (normal). A TSH above 20.0 mU/L is considered a threshold level and the analysis is repeated. At a level of 50.0 mU/L and above, hypothyroidism is suspected, and above 100.0 mU/L indicates hypothyroidism. Congenital hypothyroidism is characterized by the following changes during ultrasound: a significant decrease in the size of the gland, heterogeneity of its structure and increased echogenicity.
If the TSH level is 50-100 µU/ml, treatment with levothyroxine is immediately prescribed. It is believed that the earlier treatment is started, the fewer complications of the disease there will be in the future. In Germany, treatment is carried out from 8-9 days of life. Newborns who have not been prescribed treatment have their TSH level re-determined; if it increases, treatment is prescribed. The drug used to treat congenital hypothyroidism in children, as in adults, is levothyroxine. It is prescribed at a dose of 10-15 mcg/kg body weight immediately after receiving the results of neonatal screening. For severe forms, the dose is higher. An indicator of the adequacy of therapy is a normal TSH level, and in children under one year of age - the thyroxine . Normalization of thyroxine and TSH is achieved after 2-4 weeks. These indicators are assessed every 1-2 months in the first year of life. The initial dose of levothyroxine is 10–15 mcg/kg body weight per day. In addition, the child's need for thyroid hormones correlates with body surface area. For small children, it is prescribed in crushed form during morning feeding.
Replacement therapy is carried out for life and as the child grows and weight increases, the dose of the drug increases, since the calculation is per kg of weight. With long-term treatment, if it was correctly prescribed, the child will have positive dynamics of growth and differentiation of the skeleton, as well as general development.
Simultaneously with replacement therapy, the child should take vitamins, Cerebrolysin , Glutamic acid , Encephabol , Nootropil , Pantogam , which improve nerve cell metabolism, as well as massage and general developmental gymnastics. There are cases when congenital hypothyroidism is discovered at 10-15 years of age, and before that there were different diagnoses ( chondrodystrophy , pituitary dwarfism , Down's disease , amenorrhea , cystic fibrosis ) and improper treatment.
List of sources
- Petunina N. A. Hypothyroidism: primary, central, peripheral. Approaches to diagnosis and treatment // Diseases of the thyroid gland. 2006, vol. 8, no. 9.
- Fadeev V.V. Modern concepts of diagnosis and treatment of hypothyroidism // Problems of endocrinology. 2004, vol. 50, no. 2.
- Endocrinology. National leadership. Ed. I. I. Dedova, G. A. Melnichenko. M.: GEOTAR-Media, 2009.
- Dedov I. I., Melnichenko G. A., Sviridenko N. Yu. et al. Diagnosis, prevention and treatment of iatrogenic iodine-induced diseases of the thyroid gland // Bulletin of the Russian Academy of Medical Sciences. No. 2. 2006. pp. 15–22.
- Evdokimova Yu. A. Gestational hypothyroxinemia: outcomes, prevention and treatment // Abstract of the dissertation for the degree of candidate of science. honey. Sci. M., 2005. 24 p.