Chemotherapy is often accompanied by negative reactions of varying severity. Each drug causes certain complications, destroying both tumor cells and healthy, rapidly multiplying epithelial, reproductive, bone marrow, etc. cells. The body's response to the aggressor can occur instantly - immediately at the time of administration of the cytostatic, with a delay of a day or remotely, several years later.
Thrombocytopenia
Thrombocytopenia is one of the complications of chemotherapy, characterized by a decrease in the level of platelets (irregularly shaped cells produced by red bone marrow) in the blood. The function of these cells is to ensure blood clotting. Shaped plates close the lumen of the vessel at the site of its damage and prevent the passage of blood through it, thereby stopping bleeding. Platelets stop even significant bleeding and prevent large blood loss; without them, even a slightly cut person can die. Patients with thrombocytopenia should be especially attentive to their safety, because the slightest scratch can have unpleasant consequences for them.
Our clinic's capabilities
Is there really no way to mitigate the effect of anti-cancer drugs? - thinks every sane person. Of course it is possible, but the whole point is that this will reduce not only the toxicity, but also the therapeutic effect of chemotherapy.
Recently, photodynamic therapy has been increasingly used in the treatment of cancer. PDT is a technology proven by more than twenty years of successful practice. Selective chronophototherapy (SCPT), which is based on photodynamic therapy, is capable of activating a cascade of biochemical and cellular reactions to regulate the level of immune status indicators. A special substance is introduced into the body - chlorophyll (a natural photosensitizer of the latest generation), which accumulates in cancer cells. A laser beam is sent to the site of accumulation, capable of synchronizing with the patient’s rhythms, which makes it possible to reduce or increase the intensity of the effect. Penetrating to the required depth, it concentrates on pathological cells, destroying them, without touching healthy ones. Over the course of several months, the tumor disintegrates.
PDT is used not only to remove tumors, but also instead of chemotherapy, unlike which it does not have a destructive effect on the body. The manipulation can be performed on an outpatient basis.
Hemorrhagic purpura
After chemotherapy, the immune system may begin to produce antibodies that destroy platelets. This condition is characteristic of hemorrhagic purpura. Autoantibodies are antibodies that destroy platelets in the blood. They are reproduced by the spleen. With this disease, the body actually kills itself. The platelet content in a milliliter of blood of a healthy adult is 150-400 thousand; if the body becomes ill, the cell content can drop to almost zero. In proportion to the decrease in cell number, the likelihood of stroke increases.
How often should you have a blood test?
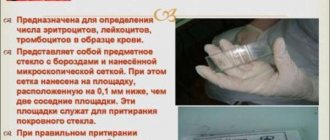
Blood tests - general with leukocyte count and platelets, as well as detailed biochemical tests - must be done before each cycle of chemotherapy. With a long cycle with weekly drug administration, the neutrophil level should be checked on the eve of administration, because the leukocyte level begins to decrease 7-10 days after the first injection of the cytostatic.
The time for performing a control blood test after chemotherapy is based on the initial state and the combination of cytostatics used, that is, always individually, but no later than 5-7 days after completion of chemotherapy. Further monitoring depends on the depth of neutropenia; daily monitoring of indicators is not excluded. If your white blood cell count is normal, the next test is scheduled before starting chemotherapy.
Acute thrombocytopenia
Thrombocytopenia is a disease characterized by the occurrence of small hematomas on the skin and internal organs. Most often it occurs after measles, rubella and other viral diseases. Often these patients experience nosebleeds and hemorrhages in internal organs. A cerebral hemorrhage can lead to a serious complication - a stroke, the recovery from which usually requires a lot of time and money.
Minor hemorrhages occur spontaneously; this is due to the fact that with thrombocytopenia, the integrity of the walls of blood vessels is disrupted and red blood cells are able to leak into the tissue. This can lead to impaired vision (due to hemorrhages in the eye) and heavy bleeding from small scratches (more often observed in the first days of the disease).
Treatment can be quite lengthy and expensive. A patient with thrombocytopenia should undergo treatment in a hospital. For treatment, glucocorticosteroids are used for a course of three to six weeks. Recently, immunoglobulins have been used. They are used in cases where it is necessary to greatly increase the number of platelets in the blood in a short time, for example before operations or childbirth. The effect of their use is short-lived.
For nosebleeds, a hemostatic sponge impregnated with thrombin is used. Sometimes anemia may require a transfusion of red blood cells or platelets. In most patients, treatment leads to complete recovery, but in 10-15% the disease can become chronic or have many relapses.
Basic questions for patients regarding chemotherapy
E.B. SHAKHNOVICH, oncologist, Federal State Health Institution Central Medical Unit No. 119, FMBA of Russia Medical Unit No. 4
Despite all the advances in medicine, the diagnosis of malignant oncological disease, in common non-medical vocabulary - cancer, remains the most psychologically unacceptable diagnosis, causing a feeling of fear and hopelessness in the patient.
Treatment of oncological pathology includes a number of techniques, such as surgical treatment, radiation therapy, antitumor treatment and many others. As a rule, antitumor treatment in non-medical vocabulary is called chemotherapy, although this concept includes a number of different drugs, such as chemotherapy itself (the use of cytostatic drugs), hormone therapy, immunotherapy, targeted therapy, etc. Drugs of these groups can be used both in combination with radiation therapy, surgical treatment, and in combination with each other, which is called combined or complex treatment.
In this article we will try to answer the main questions that arise in almost all patients who are prescribed chemotherapy treatment.
How chemotherapy drugs confuse cells
The main goal of antitumor therapy is to stop the growth of the tumor, reduce its size, reduce the clinical manifestations of the disease, and in the most favorable case, lead to its complete destruction. Each type of tumor has its own set and combination of drugs, and each patient has its own individual sensitivity and development of complications during chemotherapy, so you should never rely on other patients receiving antitumor treatment.
The mechanism of cytostatic drugs is based on the fact that these substances are released by rapidly dividing body cells (tumor cells), are integrated into the life processes of tumor cells, most often during the division process, and lead to the death of malignant cells. As a rule, several cytotoxic drugs are prescribed to have different effects on the functioning of the tumor cell, which is called a treatment regimen. Each drug has its own mechanism of action and, as a result, different types of toxicity.
In the process of creating and studying treatment regimens, drugs with different mechanisms of action and toxicity are selected, i.e. Cross (same) toxicity is eliminated whenever possible, which increases the tolerability of the treatment regimen and efficiency.
A feature of chemotherapy treatment is its duration and frequency, depending on the mechanism of action of the drugs. During the break between courses, the patient is exposed to the drug; repeated administration serves to create an optimal concentration of the drug in the blood in order to maximize the effect on the tumor. Doses of chemotherapy drugs are strictly individual for each patient and are calculated taking into account the patient’s height and weight (body surface area).
But in the human body, in addition to rapidly dividing tumor cells, there are also normal cells with rapid division according to their function. These include cells of hair follicles, bone marrow (hematopoietic precursor cells), intestinal epithelium, reproductive cells, etc. Chemotherapy drugs “confuse” these cells with the cells of a malignant tumor, which leads to complications: hair loss (alopecia), decreased levels of leukocytes (leukopenia, neutropenia), nausea and vomiting, loose stools (diarrhea), stomatitis, etc.
The most difficult psychological factor
Alopecia (hair loss) is not the most important phenomenon for the patient’s health, but it raises the first question about complications during chemotherapy, because is a psychologically difficult factor, especially for young women. Not all chemotherapy drugs cause hair loss. But if the patient undergoes preventive treatment after removal of the mammary gland for cancer with the use of Doxorubicin, Adriamycin, total hair loss is expected.
As a rule, maximum hair loss begins 10-14 days after chemotherapy is administered. In this case, in order to maintain personal hygiene, it is recommended to remove hair (shave your head) at the first signs of hair loss. Alopecia is reversible, hair restoration begins after the end of chemotherapy in approximately 2-3 weeks. Hair growth is very fast and according to our observations, the growth density increases, color changes and the appearance of curly hair growth are possible.
Not the most dangerous, but a common manifestation
Nausea and vomiting are not the most dangerous, but the most common and most painful manifestation of the toxic effect of chemotherapy drugs. There are acute nausea and vomiting, delayed and waiting vomiting.
Acute nausea and vomiting develops within 24 hours of chemotherapy administration. Delayed nausea and vomiting occurs more than 24 hours after treatment and may last several days. Anticipatory vomiting usually occurs before a second course of chemotherapy during long-term chemotherapy treatment and is psychogenic in nature. Vomiting of anticipation can be caused by the very thought of the upcoming chemotherapy the day before, the appearance of the hospital, the treatment room, specific smells, etc.
The main mechanism for the occurrence of acute vomiting is the activation of 5-HT3 receptors, which are located in the brain, neurons of the gastrointestinal tract (GIT), and the vagus nerve under the influence of serotonin produced in the cells of the upper intestine. In order to relieve this complication, pharmacology offers a sufficient range of drugs both in the form of solutions and tablet forms and suppositories. In the practice of Russian doctors, the most common drugs are Zofran (Latran, Emiset) in the form of tablets, injections or suppositories, Navobane in the form of capsules and solutions, Kytril in the form of tablets and solutions (drugs are ranked according to their effectiveness).
In order to increase the antiemetic effect of these drugs, glucocorticoid hormones are additionally used, most often dexamethasone, which, in addition to its antiemetic (antiemetic) effect, has antiallergic functions during chemotherapy. The choice of antiemetic therapy depends on the type of chemotherapy drugs, which are divided into highly emetogenic, moderately emetogenic and low emetogenic.
The mechanism of cytostatic drugs is based on the fact that these substances are released by rapidly dividing body cells (tumor cells), are integrated into the life processes of tumor cells, most often during the division process, and lead to the death of malignant cells. As a rule, several cytotoxic drugs are prescribed to have different effects on the functioning of the tumor cell, which is called a treatment regimen. Each drug has its own mechanism of action and, as a result, different types of toxicity.
Psychogenic nausea and vomiting
Initially, the prescription of anti-emetic therapy is carried out solely on the basis of the doctor’s experience; then, when an individual reaction is established, anti-emetic therapy can be changed towards intensification if the effect is insufficient. The time of administration and method of administration of the drug are determined by the instructions for use. The effect of antiemetic drugs lasts on average 8-12 hours, the effectiveness ceases 48 hours after the administration of chemotherapy and is meaningless, therefore, in order to prevent and relieve delayed vomiting, we recommend the use of cerucal, and in case of severe nausea or vomiting, the administration of dexamethasone.
All drugs in the 5-HT3 antagonist group act on intestinal activity and can cause constipation and, less commonly, diarrhea. In order to reduce toxic reactions of antiemetics, it is necessary to strictly observe the intervals between doses and the maximum permitted doses. Antiemetics do not prevent preliminary nausea and vomiting, because it is psychogenic in nature, the main drugs used for preliminary nausea or vomiting are sedatives (sedatives), selected strictly individually. The main complication of vomiting is dehydration, which can lead to heart failure due to electrolyte imbalance and venous thrombosis. If this complication occurs, it is recommended to drink plenty of mineral salts. If severe vomiting occurs more than 4-5 times a day for more than 2 days, you should consult a doctor to restore electrolyte balance by intravenous administration of electrolytes.
There is an opinion among patients
The nutrition of patients during chemotherapy treatment does not require adherence to any diet and remains typical for the patient’s daily routine nutrition. However, it is necessary to follow the diet recommended for concomitant diseases, such as diabetes, stomach ulcers, cholecystitis, etc.
There is an opinion among patients that consuming foods containing glucose promotes tumor growth or that consuming milk and fermented milk products contributes to the spread of breast cancer. But these statements are not true.
When administering chemotherapy, severe pain and a burning sensation may occur at the injection site or along the vein, which is due to the adverse effects of chemotherapy on the vascular endothelium. If these sensations occur, you should additionally “rinse” the vessel with saline solution after completing chemotherapy.
Repeated administration of chemotherapy can cause the development of phlebitis and phlebosclerosis of the veins of the limb. In order to prevent these complications, it is necessary to comply with the rules for diluting drugs and the duration of their administration according to the instructions. As an additional treatment, it is necessary to use alcohol or semi-alcohol compresses on the injection area, ointments containing anticoagulants.
In case of insufficient development of the superficial peripheral veins of the upper extremities, long-term infusions of 5-fluorouracil, and expected long-term repeated chemotherapy, it is possible to install an intravenous port, which allows treatment without the use of peripheral veins of the extremities.
Injection of chemotherapy into the arm from the surgical removal of the mammary gland should be avoided, because this can increase the symptoms of lymphostasis; taking blood from this arm is quite acceptable.
Is it possible to have children after chemotherapy?
When administering chemotherapy, an iatrogenic complication is possible: necrosis of the subcutaneous tissue when the drug gets under the skin. The occurrence of these complications depends on the practical skills of the medical worker administering the drug. The resulting necrosis is characterized by rapid spread through the subcutaneous tissue and a long process of tissue regeneration.
Allergic reactions during treatment can occur in 5-10% of patients when using various chemotherapy drugs; the most dangerous in this case are taxanes, which require specific pre- and post-medication with the inclusion of large doses of glucocorticoids. The occurrence of an allergic reaction is possible at any stage of treatment, regardless of the number of previously administered similar courses of chemotherapy.
Quite often, patients are concerned about the effect of chemotherapy on sexual function. Potency may decrease during chemotherapy, but after it is completed, erectile function is fully restored.
Chemotherapy has a significant impact on the growth and development of the egg, which can be accompanied by menstrual irregularities up to aminorrhea. Women over 40 years of age may experience menopause during chemotherapy, which in some cases requires consultation with a gynecologist.
The possibility of having children during chemotherapy is excluded for both men and women. Germ cells are highly sensitive to chemotherapy, which can lead to the development of genetic defects and the birth of an underdeveloped child. Abroad, before chemotherapy, women of reproductive age undergo a preliminary pregnancy test and sign a special document on the prevention of complications during pregnancy during chemotherapy.
It is more difficult to answer the patient’s question about the possibility of having children after treatment. There remains a risk of damage to the genetic apparatus of the egg and the development of genetic defects in the child. A patient who decides to have a child under these conditions must consult an oncologist and undergo an examination by a geneticist.
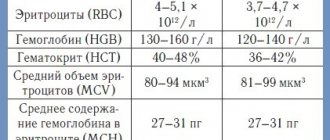
Anemia
The main damage chemotherapy drugs cause to the bone marrow, which is responsible for the formation of blood cells. As a result, hematopoietic processes are disrupted, which leads to a decrease in the number of red blood cells in the blood (anemia). The main function of red blood cells is the delivery of oxygen from the lungs to all organs and tissues, which is carried out thanks to the hemoglobin they contain. Under the influence of chemotherapy, the formation of blood cells is disrupted, which means the level of red blood cells decreases, which in turn can lead to a decrease in hemoglobin levels. These processes lead to a decrease in oxygen delivery to tissues and deterioration in the functioning of all organs. This is the main danger of anemia for the body.
Manifestations of anemia may include dizziness, palpitations, shortness of breath, and chills. Tell your doctor immediately if you notice any of these symptoms. Also, do not forget about the following recommendations:
• obligatory long night sleep and one to two hours of daytime sleep; • it is necessary to reduce activity as much as possible; • ask relatives for help with household chores (for example, cleaning the floor or looking after children); • consult a nutritionist for a balanced diet; • Avoid sudden movements to avoid dizziness.
Foods that stimulate increased white blood cell levels
As a rule, vitamin complexes are prescribed to raise the level of white blood cells, but as additional support it is necessary to review your diet and include in it foods that increase white blood cells after chemotherapy, namely: fruits and vegetables, berries, chicken and beef broths, buckwheat porridge, red caviar, seafood and fish, fermented milk products, settled beet juice. It is important to note that specific products are selected based on the type of cancer, as well as individual indicators of the body’s condition. Meals with low leukocytes should be fractional (5 times a day), balanced and complete. It is necessary to give up alcohol and tobacco. Also, foods such as animal fats, sugar, salt, sweets, strong tea, coffee, and high-fat cheeses will also not bring any benefit and, on the contrary, can even harm a weakened body.
Despite the fact that chemotherapy makes adjustments to the functioning of the body and, in particular, to the composition of the blood, modern approaches in medicine can reduce the destructive effect. You can raise the level of leukocytes both with medication and with the help of the right approach to nutrition. It is important to take into account all the features of treatment and the condition of the body and, of course, follow the doctor’s recommendations.
Share:
(0 ratings; article rating 0)
Effect of chemotherapy on blood clotting
Chemotherapy has very serious negative effects on the body, leading, for example, to a decrease in red blood cells or platelets. When undergoing a course of chemotherapy, bone marrow function may be impaired, as a result, the platelet count decreases and, consequently, the blood clotting function is impaired. Blood cells only live for a short period of time, so the bone marrow must constantly produce new ones, but if it is damaged by chemotherapy, this process is significantly disrupted.
Platelets ensure blood clotting and stop bleeding when any tissues and vessels are damaged, both large and very small, which can be damaged accidentally. If the integrity of the vessel wall is compromised, platelets disintegrate and active biological substances are released from them, which trigger a chain of sequential reactions in the formation of a blood clot. The clot closes the damaged area of the vessel and the bleeding stops.
During chemotherapy treatment, due to a sharp decrease in platelet levels, even minor scratches can cause severe bleeding, so patients should pay special attention to their safety. Also, symptoms of a decrease in platelet levels are the appearance of small bruises and hemorrhages on the body, bleeding gums, frequent nosebleeds, and occasionally blood appears in the urine (it takes on a reddish tint) and feces (it takes on a tarry appearance). Tell your doctor if at least one symptom occurs.
To ensure that complications do not affect you, the doctor must constantly monitor platelet levels and, if they drop critically, prescribe a blood transfusion.
Why is it so important to keep your white blood cell count normal?
Leukocytes have a common main function - ensuring the stable functioning of the body's immune defense. It’s worth talking separately about each faction, because each of them has its own task:
- neutrophils fight foreign bacteria and microscopic fungi;
- basophils help trigger the immune response to the penetration of foreign agents;
- eosinophils fight infections caused by parasites that have entered the human body;
- monocytes destroy and participate in the removal of pathogenic microorganisms, as well as dead cells of the body;
- lymphocytes provide an immune response when a virus enters the body. They are the basis of the immune system.
A decrease in the level of leukocytes entails unpleasant consequences, such as:
- exacerbation of chronic diseases, in particular respiratory tract infections;
- enlarged tonsils and spleen;
- bleeding gums and ulcers on the oral mucosa;
- fungal infections;
- skin infections;
- disruption of the gastrointestinal tract.
With a critical decrease in the level of leukocytes, the body ceases to resist any infections, and therefore even a simple cold can become fatal for the patient.
Neutropenia and neutrophils
The bone marrow constantly produces white blood cells called leukocytes. They are divided into three types: neutrophils, monocytes and lymphocytes. Neutropenia is a sharp decrease in the number of granulocytes in the blood. Agranulocytosis is the most dangerous type of neutropenia, in which the level of granulocytes decreases to almost zero.
The main function of neutrophils is to protect the body from infections. When they decrease, the patient is at risk of contracting dangerous infectious diseases, which may require hospitalization and the use of massive antibiotic therapy. The tissue that determines the composition of blood includes immature cells called hematopoietic stem cells, or progenitor cells. They can divide into absolutely any blood cells.
The most dangerous complication after undergoing chemotherapy is anemia. The dangers of chemotherapy are:
1. Reducing the number of red blood cells carrying oxygen; 2. Deterioration of blood clotting; 3. Decrease in the number of neutrophils.
Neutropenia is considered the most common complication of chemotherapy.
How to increase white blood cells after chemotherapy?
White blood cells, namely neutrophils, after chemotherapy can decrease to a critical level, which results in severe infections. A special form of a generalized inflammatory reaction after chemotherapy is febrile neutropenia, when nothing but a high temperature and a serious condition is found in the patient: there are no objective signs of sepsis, pneumonia and inflammation of other organs. The blood test does not find any pathological microflora - everything is sterile, only there are fewer neutrophils than normal, and the percentage may remain the same.
Neutropenia is divided into degrees as follows:
- the absolute number of cells is from one and a half thousand to a thousand, which does not exclude the development of febrile neutropenia after chemotherapy, that is, a single increase in temperature of more than 38.5℃ or twice in one day more than 38℃
- average degree from a thousand to 500 cells;
- severe neutropenia or agranulocytosis, that is, the absence of granulocytes - a drop in the neutrophil level below 500.
Stimulation of leukopoiesis is necessary only for febrile neutropenia; an asymptomatic decrease in the leukocyte fraction requires correction only in patients weakened by multiple chronic diseases.
The only effective drugs are colony-stimulating factors (CSF), there are several types of them, primarily aimed at stimulating the sprouts of white hematopoiesis. The drugs activate an increase in fertility and the rate of maturation of neutrophils in the bone marrow; with the initial use of CSF in a blood test, the result is visible within a few hours.
No other drugs, except CSF, affect the reproduction of leukocytes, but only promote the rapid removal of deposited leukocytes from the bone marrow, depleting hematopoietic resources. The number of white blood representatives is not affected by the patient’s diet or any procedures.
The use of hematopoietic stimulants is not only accompanied by unpleasant side reactions, but over time also depletes bone marrow reserves, so strict indications have been defined for CSF. CSF is never combined with chemotherapy; the drug is administered the next day after the cytostatic.