Using ultrasound, you can see most of the pathologies of the kidneys and bladder in children, such as:
- Inflammation
- Stones, sand
- Pyelonephritis
- Prolapse of the kidneys (nephroptosis)
- Cysts
- Tumor
- Organ anomaly
- Kidney expansion, etc.
Ultrasound of the kidneys and bladder in children is carried out after special preparation; the norms depend on the child’s age and gender, height and weight. Three days before the ultrasound, you should not eat spicy, fatty, fried, salty foods, or cabbage and beans. Another important condition for a high-quality procedure is to refrain from eating 7–8 hours before the examination. You can take one tablet of activated charcoal per 10 kilograms of body weight after a meal, 1 hour later (to reduce gas formation).
The examination begins with the abdomen and lower back; the doctor applies a special gel to the sensor for better conductivity of ultrasonic waves. Ultrasound of the kidneys is examined from three sides:
- From the stomach
- From the back
- On the side
After the examination, the doctor will give the result; during ultrasound, the following parameters are deciphered: width, thickness, length.
Ultrasound of the bladder in children.
It is incredibly informative for identifying pathology or an inflammatory process. How much fluid a child needs to drink before the procedure depends on age:
- Up to 2 years – 100.0.
- Up to 7 years -200.0 – 300.0.
- Up to 11 years – 500 ml.
- Up to 15 years – 700.0 – 800.0.
This examination is carried out in two stages. First they look at him with a full bladder, then they ask him to go to the toilet and look at him again. Ultrasound of the bladder is prescribed in the following cases: suspicion of urolithiasis, assessment of the shape of the bladder, inflammatory diseases, assessment of the amount of residual urine.
How does ultrasound of the bladder occur in children?
The child lies on his back, the abdominal area is freed from clothing, the doctor applies the gel to the lower abdomen, the bladder area, and begins the examination by moving the sensor over the abdomen. What can a doctor find during an examination? Attention is drawn to the shape of the bladder; its asymmetrical shape may indicate neoplasms. A small size indicates chronic cystitis in the acute stages, fibrosis (overgrowth of connective tissue due to inflammation). The bladder may contain pus, blood clots, sand, or suspension. The child is then asked to urinate and the examination continues to determine the volume of residual urine.
Normal bladder volume in children:
- Up to a year 35 – 50.0
- Up to 3 years 50 – 70.0
- Up to 8 years 100 – 200.0
- 8 – 10 years 200 – 300.0
- 10 – 14 years 300 – 450.0
Residual urine after urination is unacceptable and indicates a dysfunction of the bladder. This may be due to a small force of contraction of the bladder walls or, most often, due to the sphincter - the muscle that closes the urinary canal. The presence of residual urine indicates a violation of the emptying of the organ, this is manifested in a frequent urge to urinate, poor urine stream, urinary retention, urinary incontinence and recurrent urinary tract infection. The presence of residual urine is the only sign of vesicoureteral reflux (reverse reflux). In general, for an ultrasound, the bladder must be completely empty, but up to 10% urinary retention is acceptable:
- Newborn 2 -3.0
- Up to year 3 – 5.0
- 1 – 4 years 5 – 7.0
- 4 – 10 years 7 – 10.0
- 10 – 14 years 20.0
- Over 14 years old up to 40.0
If an ultrasound of the bladder in children reveals an excess of residual urine, it means that the child has a problem with urology.
Reasons for increased residual urine volume during ultrasound of the bladder in children.
Problems with nervous regulation, spinal injuries, hypothermia in the pelvic area, weakened tone of the bladder muscles, impaired conductivity of the urinary canal, urolithiasis of the bladder, cystitis, tumors.
To decipher an ultrasound of the kidneys and bladder in children, you need to contact a pediatrician; if there is any pathology in the examination, in this case you will need to consult a specialist doctor - a nephrologist, urologist.
Hydronephrosis in children: why you shouldn’t delay seeing a doctor
When children are sick, it is doubly difficult. Fortunately, today many congenital pathologies are 100% correctable. These include such a serious disease of the genitourinary system as hydronephrosis. Artur Vladimirovich Kulaev, a pediatric surgeon, urologist-andrologist at the Department of Pediatric Urology and Andrology at the Morozov Children's Hospital, told the Moscow - Capital of Health project about what hydronephrosis is like, how it is diagnosed and what modern methods are successfully used to treat the disease.
What is hydronephrosis?
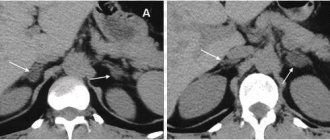
Hydronephrosis is a kidney disease that is characterized by expansion of the collector system and thinning of its parenchyma (the main tissue of the kidney). The high pressure that is created in the pelvis and calyces negatively affects the working part of the kidney. Thinning of the parenchyma and deterioration of blood flow inside it cause dysfunction of the kidney, and, ultimately, can lead to its death.
What types of diseases exist?
There are two types of hydronephrosis: congenital or acquired. When it comes to pediatric urology, congenital hydronephrosis is more common. Typically, the disease is caused by stenosis (narrowing) of the ureter where it leaves the pelvis, but other causes are possible.
As for acquired hydronephrosis, it appears at an older age, when children develop, for example, urolithiasis. In this case, obstruction is caused by concretions (i.e. stones) in the area of the upper third of the ureter. Also, acquired hydronephrosis may be based on various oncological diseases, for example, when a tumor outside the kidney compresses the area where the ureter departs from the pelvis.
What are the symptoms of hydronephrosis?
Unfortunately, there are no specific symptoms of hydronephrosis. The only sign that may indicate that the child’s pelvis is critically dilated is the so-called kidney block. This is a complex of symptoms manifested by pain in the lumbar region, nausea and vomiting. If they are present, you should immediately seek help from a doctor who will conduct a differential diagnosis.
How is renal hydronephrosis treated in children?
We treat hydronephrosis surgically. Surgical interventions for hydronephrosis are divided into two groups: laparoscopic and open. They are aimed at restoring the patency of the urinary tract, that is, removing the obstacle that prevents urine from flowing from the pelvis into the ureter without problems. In the Morozov Hospital, since 2010, preference has been given to laparoscopic operations, in which the trauma for the child is minimal, and therefore the pain syndrome is less pronounced and the period of hospitalization is shorter.
Tell us in more detail how laparoscopic surgery is performed?
The correct name of the operation is “laparoscopic ureteroplasty” (or laparoscopic pyeloplasty). Laparoscopic pyeloplasty is highly effective and is currently considered the gold standard in the treatment of hydronephrosis. How is it different from open surgery? Open surgery for hydronephrosis is performed using conventional surgical instruments: an incision is made in the lumbar region or abdomen, and then reconstruction is performed from this incision.
With laparoscopic pyeloplasty, the operation takes place practically without blood: we use optics, which we insert into the child’s abdomen through 3 small punctures, and manipulators - special laparoscopic instruments. Next, we look at the monitor and work with our hands inside the child’s abdominal cavity. The operation is performed under general anesthesia and can take from 1.5 to 3 hours, depending on how the kidney is positioned in relation to our camera (whether it is rotated or not, etc.).
What is the key to success in surgical treatment of hydronephrosis at the Morozov Children's Clinical Hospital?
In short, I would highlight three components of success: modern equipment, professionalism of surgeons and a multidisciplinary approach to treatment. We have accumulated the most experience of all Russian clinics in the treatment of hydronephrosis using laparoscopic technologies. We are actively working with 3D laparoscopy. This is a unique equipment that allows the surgeon to see a three-dimensional picture and more accurately perform movements, apply sutures and perform other manipulations. We can see better and understand more clearly what we are doing, and the three-dimensional picture is more familiar to the human eye. As a result, the risk of bleeding, as well as other postoperative complications, is reduced to almost zero.
How accessible is surgery for hydronephrosis in a child at Morozov Hospital to non-residents?
All types of laparoscopic pyeloplasty at the Morozov Hospital are performed free of charge for patients, regardless of their place of residence. The only condition is the presence of a compulsory medical insurance policy.
How long will it take for a child to recover after laparoscopic pyeloplasty?
On average, 5 - 7 days. During the first 24 hours after surgery, the child is prescribed bed rest. In addition, the patient is under 24-hour supervision. Then, for 2 - 3 days, the child receives the necessary antibacterial and infusion therapy (in the form of droppers), after which he is discharged home.
What is the current prevention of hydronephrosis in children?
Unfortunately, the disease cannot be prevented by taking medications. Taking this opportunity, I want to appeal to all parents who are faced with the problem of hydronephrosis in a child: there is no need to be afraid. Just seek professional help as soon as possible.
Source: Moscow - the capital of health
What kidney pathologies in the fetus can be detected at the 2nd screening
The 2nd screening is carried out at 20-24 weeks of pregnancy. It reveals various kidney defects in the fetus:
- Agenesis (absence of one or both kidneys) . With unilateral agenesis, on ultrasound, on one side the kidney is not visualized at all, but on the other side it is enlarged compared to the norm. With bilateral agenesis, there is no organ at all, so the fetus usually dies at a certain stage of pregnancy. Unilateral agenesis is not an indication for abortion, because a person can live with one kidney.
- Dystopia (atypical position of the organ). The location of the kidney is the renal fossa. Sometimes the kidney does not rise into the fossa, but is located in any area of the pelvis. In this case, the dystopic kidney will not be visible on ultrasound, so an inexperienced doctor may mistake dystopia for agenesis.
- Enlarged or reduced organ size;
- Dilatation of the renal pelvis over 2 mm from normal;
- Pyeelectasia is an enlargement of the renal pelvis without concomitant pathologies of the organ;
- Pyeloureterectasia - dilation of the renal pelvis with dilation of the ureter;
- Pyelocalicectasia is the simultaneous expansion of both the renal pelvis and the calyx.
- Hydronephrosis is the accumulation of urine in the pelvis, leading to an increase in the size of the cups and pelvis. Urine accumulates at the base of the ureter, causing it to expand. Pathology is not a disease, but indicates pathology of the pelvis and renal cup. Diagnosed in 80% of pregnancies. If by the time of birth the renal pelvis is enlarged by more than 10 mm, the baby will need urgent surgery.
- Kidney cysts. Multicystic dysplasia is one of the most dangerous kidney diseases. It is expressed in the degeneration of nephrons into cysts, which clog the ducts and impede the outflow of urine. They contain fluid inside and reach a size of 3-4 cm. In case of bilateral multicystic kidney disease, doctors recommend terminating the pregnancy, and in case of unilateral pathology, removing the affected kidney immediately after the birth of the baby.
- Polycystic kidney disease has several cysts of 1-2 mm in size on the organ. They are not visible on an ultrasound machine, but their presence is indicated by oligohydramnios in the pregnant woman and bilateral enlargement of the kidneys in size. The echogenicity of the kidneys will be increased, and the outline will be white. In this case, the woman is sent for an abortion because the fetus dies in the womb.
- Obstruction of the ureteropelvic anastomosis . Ultrasound visualizes the expansion of the renal pelvis while maintaining the normal width of the ureter and renal cup. The amount of amniotic fluid remains normal, and kidney underdevelopment is also not observed. Against the background of obstruction of the ureteropelvic anastomosis, hydronephrosis occurs (stagnation of urine in the kidney).
The pathology is dangerous because renal dysplasia develops against its background - damage to the kidney tissue by cysts that impairs the functionality of the organ. On ultrasound, the kidney becomes hyperechoic and cysts appear in it.
Causes of abnormal kidney development in the fetus
Hypoplasia or underdevelopment of the kidney is an intrauterine anomaly in which the kidney is small and does not function properly. The deviation occurs in less than 0.2% of all pregnancies.
The following factors contribute to the development of renal hypoplasia:
- early trips to warm countries, exposure to the sun, overheating;
- blows to the stomach, falls;
- the influence of alcohol and tobacco smoking;
- inflammation of the uterus;
- exacerbation of pyelonephritis, infection of the fetus;
- negative impact of medications;
- food poisoning causing intoxication of the body;
- oligohydramnios;
- TORCH infections in the mother;
- renal vein thrombosis in the fetus;
- exposure to ionizing radiation.
On ultrasound, hypoplasia is easily noticeable; the kidneys are visualized from the 14th week of pregnancy. A high-precision 3D device will help with this. The kidney is displayed on the monitor screen as an oval or bean-shaped formation in longitudinal scanning and round in transverse scanning.
The kidney is a paired organ located on either side of the spine. The basis of the organ is the renal pelvis, consisting of renal calyces merging with each other. The pelvis gradually narrows and passes into the ureter, which leads to the bladder. The ureter itself in a healthy fetus is not visualized on ultrasound.
In a healthy organ, the diameter of the renal pelvis is 4-5 mm in the 2nd trimester and 7 mm in the 3rd trimester. The structural and functional unit of the kidney is the nephron, which carries out filtration. At 1 screening, you can verify the presence or absence of kidneys, unilateral or bilateral underdevelopment (hypoplasia), kidney duplication, as well as normal or abnormal location. But the functionality of the organ will become clear at the 2nd screening.
Kidney ultrasound with Doppler ultrasound
In our center, ultrasound of the kidneys in children can be performed with Doppler ultrasound - an additional study of the blood flow of the renal vessels. The assessment is based on 15 different indicators: the direction and speed of blood movement, the width of the lumen of the vessels and the pressure inside them, and so on. Doppler testing of renal vessels helps to determine the causes of some renal diseases, for example, arterial hypertension, a disease that occurs even in childhood. Arterial hypertension is caused by stenosis (narrowing of the lumen) of the renal arteries, which can only be detected using Doppler ultrasound.
Useful!
|