until September 30
Appointment with a doctor based on the results of instrumental diagnostics with a 50% discount More details All promotions
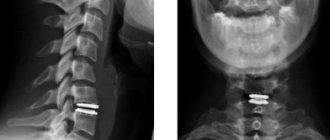
X-ray of the spine (x-ray of the spine)
is a simple and effective diagnostic method that allows you to identify pathologies, primarily associated with spinal deformity.
The human spine is adapted to upright posture: it connects various parts of the skeletal system, maintains the vertical position of the body and acts as a shock absorber when walking. That is why the spinal column has an S-shaped, curved shape and is not a rigid rod, but a complex structure consisting of elements attached to each other - vertebrae. Between the vertebrae there are intervertebral discs that absorb shocks and shocks.
The spine is divided into sections. Highlight:
- cervical spine, consisting of 7 vertebrae (designated C1-C7);
- thoracic spine: 12 vertebrae (designated D1-D12);
- lumbar: 5 vertebrae (designation L1-L5);
- sacrum or sacrum: 5 fixed vertebrae that form the sacrum;
- coccyx.
X-ray of the spine in the clinics of JSC "Family Doctor"
In most cases, an x-ray of a specific part of the spine is performed. At the Family Doctor clinics you can do:
- X-ray of the cervical spine
(including with functional tests); - X-ray of the thoracic spine
; - X-ray of the lumbosacral spine
(including functional tests); - X-ray of the coccyx
.
X-rays are performed in one or two projections (posterior and lateral). The essence of radiography of the spine with a functional test is that the picture is taken in the position of maximum possible flexion or extension. The position in which the photograph is taken is selected individually, depending on the mobility of which segment of the spine requires information.
Treatment tactics
After all the necessary examinations, treatment tactics are selected.
If conservative (non-surgical) treatment is possible, a corset is selected for the patient, and primary rehabilitation is carried out (the abdominal and back muscles need to be strengthened).
If a decision is made to undergo surgery, the doctor will determine the type of surgical treatment. You can read more about this in the section “For persons with medical education.”
Thanks to reliable and proven methods, the experience of surgeons, as well as modern technologies, patients recover quickly.
What does a spine x-ray show?

An X-ray of the spine can detect:
- pathological or physiological curvature of the spinal column;
- changes in the structure of vertebral bone tissue;
- tumor processes (for example, metastases to the spinal column);
- damage to articular surfaces;
- violation of the integrity or symmetry of the vertebrae;
- accumulation of fluid in joint cavities;
- changes in the vertebral discs;
- bone growths.
What diseases can be detected by a spinal x-ray?
An X-ray of the spine helps diagnose the following diseases and pathologies:
- spinal injuries (fractures, vertebral dislocation, subluxation);
- compression (compression) of the vertebrae;
- curvature of the spinal column (scoliosis, lordosis, kyphosis);
- osteochondrosis;
- osteoporosis;
- degenerative changes of the spine (for example, osteoarthritis);
- spinal tuberculosis;
- tumor changes;
- congenital anomalies of the spine;
- systemic diseases (rheumatoid arthritis, ankylosing spondylitis, etc.).
When is a spinal x-ray necessary?
An X-ray of the spine is prescribed if the above diseases are suspected. Indications for an X-ray of the spine may include:
- headache;
- dizziness that occurs when sharply tilting or turning the head (in these two cases, an x-ray of the cervical spine may be prescribed);
- pain in the chest or abdomen (x-ray of the thoracic spine);
- back pain;
- numbness of the limbs;
- weakness in the arms or legs.
Osteochondrosis?
Synonyms: radiculitis, salt deposits. Between the bodies of two adjacent vertebrae there is an intervertebral disc that performs 3 functions: shock absorption, holding adjacent vertebrae, ensuring mobility of the vertebral bodies. With osteochondrosis, the intervertebral disc loses its elasticity, becomes less durable, and therefore cannot perform its functions. Salts are deposited at the junctions of the vertebrae, bone growths appear, which, together with the discs, can shift and compress the nerve roots. This causes pain.
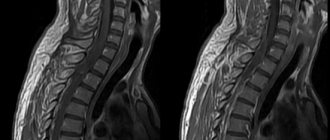
Manifestations of osteochondrosis are herniated intervertebral discs. A lumbar hernia causes pain in the back, buttocks, sacrum, and can spread to the legs. If you have any of these symptoms, it is necessary to undergo an examination, which includes not only x-rays, but also magnetic resonance imaging (MRI). When determining treatment tactics, we rely on MRI data. If an MRI reveals a disc herniation, the patient is most often frightened by this “terrible” diagnosis - not surgery! It must be said that for surgery for a herniated disc at the lumbar level, good reasons are needed. The patient makes the final decision after consultation with a neurosurgeon - vertebrologist.
A disc herniation causes severe pain, even with slight exertion, which interferes with life and work. If the patient wants to significantly improve the quality of his life, he will choose surgical treatment that will permanently rid him of this disease.
Another question arises: Where to have surgery? What to look for when choosing a medical institution?
To successfully perform an operation, in addition to the knowledge and skills of the surgeon, you need appropriate equipment in the operating room (Electro-optical converter (EOC) - a special X-ray unit, a powerful operating microscope, a special set of microsurgical instruments). The operating rooms in our clinic meet all these requirements and are fully equipped with everything necessary for spinal surgery.
A question that people leading an active lifestyle ask: How many days will the hospital stay take in case of surgery? Before surgery – from 2 to 5 days. After surgery – up to two weeks. The patient gets up on the second day and is discharged after the stitches are removed. He is offered a special rehabilitation program that will allow him to recover as soon as possible and return to an active lifestyle.
Preparing for a spine x-ray
No preparation is required for x-rays of the cervical and thoracic spine.
When preparing for an X-ray of the lumbosacral region, three days before the study, it is necessary to avoid consuming foods that cause increased formation of gases in the intestines (cabbage, brown bread, legumes, milk, carbonated drinks). On the day before the test you should not eat after 19-00. The study is carried out on an empty stomach. The evening before the test, you should cleanse your intestines (using an enema or laxative).
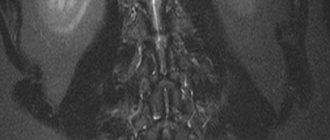
Examination of the lumbosacral plexus, nerves of the legs (sciatic nerve)
The lumbosacral nerve plexus conducts nerve impulses to the lower extremities and ensures their mobility and sensitivity. If the lumbosacral plexus is damaged, you can pay attention to some symptoms: pain along the nerves, changes in sensitivity, weakness and “wobbiness” of the legs.
The study of the lumbosacral plexus and nerves of the legs begins with an examination by a neurologist, after which diagnostic tactics will be determined. Most often, diagnosis of damage to the lumbosacral joint and nerves of the legs includes: ENMG, ultrasound of nerves, blood tests. In some cases, additional studies may be needed, in particular MRI scanning of the spine and pelvic organs.
We will offer you an examination of the lumbosacral plexus and nerves of the legs in order to find out the exact location of the damage to the plexus or nerve of the leg and the cause that led to the appearance of symptoms of nerve or nerve plexus pain.
After the examination, the neurologist will determine which nerve the disorder occurred in and will offer a set of examinations. Typically the examination includes:
- Electroneuromyography (ENMG) is used to pinpoint the location of nerve damage. Using electroneuromyography, we accurately determine at what level the nerve impulse stopped flowing from the brain to the legs or vice versa.
- Needle myography helps to study in more detail how a muscle responds to a nerve impulse.
- Ultrasound examination of the lumbosacral plexus and nerves of the legs (including the sciatic nerve).
- MRI of the lumbar spine, lumbosacral plexus. We recommend MRI of the pelvis because inflammation in the pelvis (endometritis, endometriosis, effusion due to cancer and inflammatory diseases of the pelvis, proctitis, paraproctitis, prostatitis, etc.) often leads to compression of the lumbosacral joint and causes symptoms of nerve damage. If pelvic diseases are detected, we will offer you the help of a urologist, gynecologist or gastroenterologist. MRI of the leg is useful for assessing the anatomical integrity of the nerves, but in many cases we can replace MRI of the leg with ultrasound.
Lower extremity stimulation electromyography (ENMG) will help determine the exact location of nerve damage.
Examination for inflammation of the lumbosacral nerve plexus and leg nerves. Nerve diseases can be caused by neuroinfections (borrelia, herpes simplex, cytomegalovirus, Epstein-Barr virus, herpes zoster, etc.) or aggression of the immune system towards the nerves. In this case, we will offer you studies for neuroinfections and autoimmune diseases of the nervous system (ALS, CIDP, multiple sclerosis, etc.)
Our frequent findings during the study of nerve plexuses, nerves and the search for the cause of nerve suffering: herniated disc, neoplasm, injury (sports, household, etc.), inflammation, nerve compression.