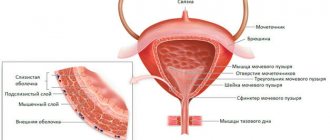
The pelvic floor is a dome-shaped layer of muscle that separates the pelvic cavity above from the perineal area below. The pelvic cavity contains internal organs such as the bladder, rectum and uterus (in women).
The pelvic floor muscles perform the following main functions:
- Supports the abdominal and pelvic organs.
- Control the retention of urine and feces.
- They enable defecation and urination, affect sexual function and play an important role in the process of childbirth.

Pelvic cavity (inside view)
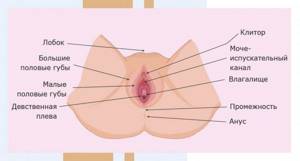
External female genitalia
The external genitalia of a woman are located outside, accessible for visual inspection, collectively called the vulva.
These include:
- The pubis is a mound-shaped projection covered with fatty tissue located in front of the vulva. The pubis becomes covered with hair at the onset of puberty. The degree of hair growth depends mainly on heredity.
- The labia are large - covered with pubic hair, contain glands (sweat and sebaceous), and therefore can be subject to skin lesions (cysts, boils). Large lips hide other organs completely or partially. The shade of the inner part of the lips is pinkish to brown. The main function is a barrier, they protect the vagina from microorganisms and retain moisturizing secretions. With the onset of sexual life, lips tend to part.
- The labia minora have the appearance of elastic, well-stretchable folds of skin located between the vagina and the labia majora. Size, color and even shape may vary. Elastic properties are necessary during childbirth. When excited, the lips swell.
- The clitoris is located “at the junction” of the labia minora, has a head covered with a “hood”.
- The external opening of the urethra (urethra) is located in front of the vagina below the clitoris. Urine leaves the bladder through the urethra.
- Vagina - occupies the space between the opening of the vagina and the cervix. The muscular organ is covered with a mucous membrane that contains glycogen. With the help of glycogen, lactic acid is formed, due to which the vaginal secretion acquires protective properties that prevent the penetration of pathogenic microflora into the genitourinary system. In women who have not had intimate contact with a man, the entrance to the vagina is covered by the hymen (hymen).
- Perineum - located between the anus and the vulva, can be torn during childbirth.
- Bartholin's (larger vestibular) glands are paired glands located at the base of the labia majora and in their thickness. Their size is 1.5-2 cm. During sex and arousal, the glands secrete a gray-transparent liquid.
Diagnostics
In order to identify pathologies of the pelvic organs, you must first consult a doctor.
In case of damage to the genital organs, a gynecologist can solve the problem:
- Diagnosis begins with a conversation, a detailed clarification of complaints, symptoms, as well as predisposing factors.
- The doctor examines the genital organs to determine the anatomical condition, identify pathological symptoms, etc.
- A mandatory part of the examination is the collection of material to study the microbiocenosis of the vagina , as well as a smear for oncocytology from the cervix or other most suspicious areas.
- Laboratory tests may include both the assessment of biological fluids, such as the determination of indirect signs of inflammation in the blood, and the assessment of the hormonal profile.
- Of the instrumental methods, the most popular currently is ultrasound examination (ultrasound). It allows you to assess the condition of the genital organs and the possible functioning of the hormonal system.
- Computed tomography may be used.
- In the presence of severe pathological conditions, methods such as hysteroscopy, laparoscopy and diagnostic laparotomy are used for diagnostic purposes . The latter serve not only as diagnostic methods, but also as possible treatment.
Internal female genital organs
The woman's genitals, located inside, can be examined using gynecological instruments or ultrasound.
These include:
- The uterus is a muscular hollow organ, the main function of which is to serve as a container for the development and preservation of the fetus during the gestational period. The inside of the uterus is lined with endometrium (mucous layer). The endometrium changes under the influence of hormonal substances. It consists of a body and a cervix, which is up to 4 cm long. The cervix consists of a vaginal part that has an internal os and a supravaginal (uterine) part that opens into the uterus. The mucous membrane of the cervix secretes a mucus barrier to microorganisms. Liquid mucus secreted before ovulation facilitates the passage of sperm into the uterus. During labor and delivery, mucus helps the fetus move.
- The fallopian tubes are a paired organ that extends from the uterus on the right and left sides. The tubes originate from the corners of the uterus, their size is 10 cm. The fallopian tubes have openings: one goes into the abdominal cavity, it is wide, the second goes into the uterine cavity, it is narrow. The main function of the tubes is transport; cilia on their surface “push” the embryo into the uterus.
- The ovaries are a pair of small organs located on both sides of the uterus. The main function of the ovaries is the production of hormones, the main of which is estrogen. The ovaries also contain follicles (vesicles) with oocytes. Every month, one follicle ruptures, releasing a mature egg for the fertilization process.

Pelvic structure:

Pelvic bones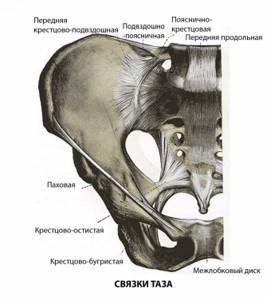
Pelvic ligaments
- The pelvis consists of two pelvic (or innominate) bones, the sacrum and the coccyx.
- The entrance to the small pelvis is located at the level of the sacral promontory and the upper edge of the pubic bones.
- The exit from the small pelvis is formed by the pubic arch, the ischial spines, the sacrotuberous ligament and the coccyx.
- The closed space between the inlet and outlet is called the true pelvis, with the inlet plane being at right angles to the outlet plane.
- The female true pelvis differs from the male one in that it is shorter, has smoother surfaces, a wider angle of convergence of the lower rami of the pubic bones and a wider plane of exit of the small pelvis.
- There are gynecoid, android, platypeloid and anthropoid forms of the female pelvis.

Pelvic shapes
Phases of the menstrual cycle
A woman's body functions cyclically. The average length of a cycle, called menstrual, is 28 days. They follow one after another. Menarche (first menstruation) begins at 11-15 years of age.
The cycle consists of three phases:
- Follicular.
- Ovulatory.
- Luteal.

Follicular phase
Starts on day 1 of menstruation and lasts 7–22 days, usually 14 days.
Processes in the ovaries
- Several follicles with eggs develop, of which by the 7th day one dominant one is determined. The rest are gradually deteriorating.
- The dominant follicle grows and secretes the hormone estradiol.
- The phase ends with the complete maturation of the follicle and the egg in it.
Signs
- At the beginning of the phase - bleeding from the uterine cavity, malaise, anemia, increased appetite.
- At the end of the phase, you feel better, work capacity increases, and you are in a good mood.
Ovulatory phase
Lasts about three days.
Processes in the ovaries
- The egg is released from the follicle and begins to move through the fallopian tube towards the uterus.
- This is ovulation - the time of conception.
- Its duration is about a day.
Signs
- Libido increases.
- Emotional uplift and desire to please.
- The lower abdomen may ache during ovulation.
- Vaginal discharge becomes more abundant and resembles egg white.
Fertile days are days close to ovulation, that is, they are located closer to the middle of the menstrual cycle. During this period, you are more likely to get pregnant if you have unprotected sex.
Luteal phase
Occurs after ovulation. If pregnancy does not occur, this phase lasts 13–14 days and ends with the beginning of the next menstruation.
Processes in the ovaries
- The corpus luteum, formed from the remains of a burst follicle, produces hormones for 10–12 days that are necessary for the successful implantation of a fertilized egg in the uterus.
- If fertilization of the egg does not occur before entering the uterus, it dissolves in its mucous membrane. And after this time, the corpus luteum stops secreting hormones and is destroyed.
Signs
- Metabolism slows down.
- A woman is gaining weight.
- Due to a decrease in smooth muscle tone, bloating and heaviness are felt.
- Malaise.
- Drowsiness.
- Decreased performance.
- Depressed mood.
- Depression.
Vaginal muscles
These are smooth muscle fibers that are necessary to maintain the tone of one of the pelvic organs - the vagina. They cannot be consciously controlled, so very often women complain about the problem of their tone, etc.
The only way to train these muscles is to change intra-abdominal pressure. This requires an alternating increase and decrease in intra-abdominal pressure in order for secondary recruitment of smooth muscle fibers to occur.
How to strengthen the pelvic floor and vaginal muscles?
Any muscle tissue of the human body requires regular maintenance of tone. In order to achieve this, regular exercises aimed at training muscle fibers are required.
The muscles of the pelvic floor and vagina also require regular training and maintenance of tone. This is especially true for those women who have recently given birth to a child naturally. It is after childbirth that the muscles of the pelvic floor and vagina tend to decrease in tone after relaxation and strong stretching.
At this time, several rules regarding special exercises must be observed. Such sets of exercises are also called Kegel exercises or vumbiling.

Vumbiling or intimate gymnastics
In order to maintain normal muscle tone and avoid prolapse and prolapse of the pelvic organs, you should use gymnastics and perform exercises according to the following scheme:
- Lie on your back and relax. Your arms should be at your sides and your legs should be bent so that your feet are shoulder-width apart.
- At the same speed, you should raise and lower your pelvis at least 40 times. The exercises should be performed with a short break.
- When performing the next exercise, the position must be left the same, but to perform it you will need to tense the sphincter and all intimate muscles. This exercise should be performed 10 times.
- In the next exercise, you should tense the muscles of your thighs and buttocks, while your feet should be placed side by side. The exercise requires 25 repetitions.
- You can perform such exercises with the help of specialized tools aimed at enhancing the development of muscle fibers.
Stages of the menstrual cycle
There is a small endocrine gland in the brain that produces hormones and controls the production of hormonal substances by other endocrine glands - the pituitary gland.
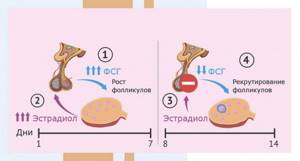
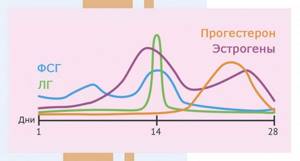
With the onset of the follicular phase, it produces follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Under their influence, up to 20 follicles mature in the ovaries, and estrogen production increases. After a certain time, the dominant follicle stands out, the rest undergo regression. The dominant follicle matures and produces estrogens. With a sufficient concentration of estrogens, they begin to suppress the synthesis of FSH. After the follicular phase, which lasts about two weeks, the ovulatory phase begins.
At the ovulatory stage, LH synthesis increases. Under its influence, the dominant follicle matures and bursts, releasing an egg that enters the abdominal cavity and from the cavity into the fallopian tube. This process is called ovulation. The cervix begins to increase the production of mucus, which helps sperm enter the uterus to meet the egg.
After menstruation, the luteal phase begins, lasting two weeks. The dominant follicle from which the egg is released is transformed into the corpus luteum. Its main function is the synthesis of progesterone (pregnancy hormone). Progesterone prepares the uterus for bearing a fetus: the mucous membrane of the organ swells and grows with blood vessels.
Then one of two scenarios is implemented:
- Pregnancy occurs if the “meeting” of sperm and egg occurs successfully and ends in conception. The embryo is implanted into the wall of the uterus and develops.
- Pregnancy does not occur, then the hormonal background changes, the endometrium is rejected, and menstruation begins.
Correctly, the monthly cycle is called menstrual-ovarian, since changes affect not only the endometrium, but also the gonads. The cycle length is calculated from the first day of menstruation in one cycle to the first day of subsequent menstruation. The ovarian cycle includes: follicle maturation, ovulation, transformation of the follicle into the corpus luteum.
Menstruation
Ovulation
Fertile day
Do you want to receive a personal ovulation calendar by e-mail?
Your ovulation calendar
How many eggs are there in the ovaries
Each woman receives a certain number of eggs from birth (ovarian reserve) and then this number is not replenished, but is only used up throughout life.
At birth, the ovarian reserve is 1-2 million eggs. By puberty, there are about 300 thousand of them.
Approximately 500 germ cells mature, leave the ovary and are ready for fertilization. All other germ cells remain unclaimed and die.