Full text of the article:
Examinations that provide information about the state of the gastrointestinal tract cannot be called pleasant procedures. Colonoscopy and gastroscopy are very often a reason for patients not to contact specialists. But modern medicine suggests performing a colonoscopy and FGDS under anesthesia at the same time, thereby relieving the patient of such unpleasant sensations and even minimal pain.
When is it necessary to do a gastroscopy?
It is a mistake to underestimate the effectiveness of these two methods in determining a number of diseases. For doctors, they are the main ones in the study of the gastrointestinal tract.
Gastroscopy helps to identify diseases such as:
- peptic ulcer;
- malignant diseases of the esophagus, stomach;
- presence of erosion;
- polyps;
- types of gastritis;
- the presence of foreign bodies and much more.
Most often, a doctor will refer you for a gastroscopy if you complain of stomach pain, frequent heartburn, vomiting, loss of appetite, weight loss, difficulty swallowing and pain associated with eating.
A modern endoscope is able to show the most accurate information about the state of the gastrointestinal tract to the doctor, while the examination is carried out more thoroughly under drug sedation.
The main requirements for the patient during gastroscopy are to limit food intake 10 hours before the examination, as well as abstain from drinking water for three hours.
If the patient needs to take medications on a special schedule, it is worth agreeing with the doctor.
Gastro- and colonoscopy
- Home /
- Branches /
- Endoscopy /
- Gastro- and colonoscopy
- Price
- Colonoscopy with anesthesia RUB 14,000.
- Colonoscopy RUB 8,600
- Gastro + colonoscopy under anesthesia RUB 19,400.
- Gastroscopy under anesthesia RUB 10,800.
Specialists from the endoscopy department of the Yauza Clinical Hospital perform gastroscopy and colonoscopy under anesthesia in the iScan expert mode. Studies are performed using narrow-spectrum lighting, which helps to clearly visualize the vascular pattern of the mucous membrane and diagnose pathology with the highest accuracy at an early stage of development.
We identify various diseases of the stomach, esophagus, and duodenum, including ulcers, gastritis, duodenitis, esophagitis, acute or postoperative colonic obstruction, irritable bowel syndrome, and neoplasms. During the process, it is possible to remove foreign objects, remove tumors, stop bleeding, and perform a tissue biopsy.
You should contact a specialist if you are concerned about symptoms such as constipation, flatulence, a feeling of incomplete emptying of the intestines, blood in the stool, heartburn, nausea, vomiting, belching, dysphagia, pain in the stomach, weight loss, lack of appetite. Early diagnosis of diseases allows you to prescribe effective treatment in a timely manner and prevent the occurrence of complications.
In order to make the procedures as comfortable as possible and eliminate the risk of side effects, we perform gastroscopy and colonoscopy under sedation . You will be able to leave the clinic shortly after the procedures are completed. Sedation allows for the most accurate diagnosis and various therapeutic procedures.
Preparation and execution
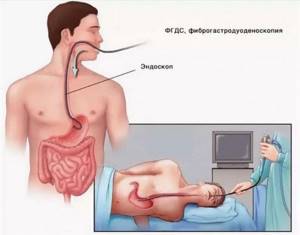
The procedures are performed using an endoscope, a device that is a flexible tube equipped with an optical system and a light source.
The patient needs to follow a diet for several days: exclude foods rich in fiber, dyes, carbonated drinks, black coffee, milk from the diet, and also take medications to cleanse the intestines. Before the procedures, you need to abstain from eating for 8–10 hours.
Learn more about preparing for a colonoscopy
You should have your ECG results with you. You can undergo an electrocardiogram at our medical center immediately before the examination.
Contraindications include severe heart failure, peritonitis, acute myocardial infarction, stroke. Driving is not recommended after the procedure.
You can see prices for services
Indications and contraindications for the procedure
Gastroscopy can be prescribed for the purpose of preventive examination of the gastrointestinal tract, to monitor the effectiveness of treatment, as well as to take tissue samples (biopsy).
The study makes it possible to determine the causes of the following symptoms:
- pain in the epigastric region associated with eating;
- heartburn;
- nausea and vomiting;
- a feeling of heaviness and bloating that is constant.
Contraindications to gastroscopy are serious forms of mental disorders, as well as acute heart diseases. Diagnostics is not recommended for patients suffering from severe respiratory failure, hypertensive crisis and during the rehabilitation period after a heart attack and stroke. Gastroscopy in a dream is mandatory for people with a low pain threshold, a labile psyche, and children under 12 years of age.
Carrying out FDGS
Preparation for examinations under anesthesia with MOVIPREP
Share information with your Facebook friends
VK
Preparation for examinations under anesthesia with MOVIPREP
The examination under sedation or anesthesia must be done strictly on an empty stomach. You cannot even drink water later than 3 hours before the test. Features of preparation for the research themselves are given below.
Tests for anesthesia (the need is determined by the anesthesiologist and the corporate requirements of the clinic; the Ministry of Health does not regulate):
- HIV.
- Hepatitis B and C.
- Syphilis.
- General blood analysis.
- General urine analysis.
- Fluorography of the chest organs (X-ray, CT) no more than 1 year ago.
Preparation for gastroscopy
Does not require special preparation. The evening before the study, the last dinner at 18:00 without meat products and cottage cheese. The water regime is maintained until bedtime.
In the morning on the day of the examination, do not drink, do not eat, do not take pills, do not smoke, brush your teeth without toothpaste, do not chew gum.
Regarding the morning intake of tablet medications, additionally consult with your doctor or endoscopist.
On the day of the test, you can rinse your mouth with water.
Preparing for a colonoscopy
Preparation for colonoscopy (intestinal endoscopy) includes 3 stages: following a diet, choosing a nutrition plan depending on the time of intestinal endoscopy, and the process of bowel cleansing itself. Each liter of drug solution takes an average of 2 hours to act. While taking the drug, it is recommended to perform light physical exercises: circular rotations of the pelvis, bending to the sides, forward, backward, squats. You can do some light house cleaning: dusting, vacuuming, vacuuming, tidying up your closet.
The criteria for a patient's readiness for intestinal endoscopy are the appearance of liquid that is clear or slightly yellow in color.
The appropriate time frame for traveling to the clinic for a colonoscopy must be considered. If it is possible to undergo training at a clinic, find out about it in advance. Some patients find it easier to undergo it under the supervision of medical staff.
Stage 1. Diet.
Forbidden
1-2 days before colonoscopy.
All plant foods: vegetables and fruits, berries, herbs, cereals and cereals, nuts, bread. Colored juices, alcohol, carbonated drinks and everything that is not included in the “allowed” section.
Allowed
1-2 days before colonoscopy.
All protein foods: boiled meat and poultry with the exception of sausages, low-fat fish, low-fat fermented milk products, cottage cheese, eggs. Low-fat clear broth, weak black tea without milk, compote without berries, clarified juice without pulp, non-alcoholic, uncolored clear drinks, water.
Stage 2. Colonoscopy time.
Colonoscopy in the morning (before lunch)
If intestinal endoscopy is scheduled between 8:00-10:00. Recommendations: the day before the colonoscopy, before 9:00, breakfast according to the list of allowed foods. Lunch and dinner - only permitted liquids.
If intestinal endoscopy is scheduled between
10:00 and 14:00.
Recommendations: the day before the colonoscopy, before 13:00, breakfast and lunch according to the list of allowed foods. Dinner - only permitted liquids.
Colonoscopy in the evening (after lunch)
If intestinal endoscopy is scheduled between 14:00 - 19:00. Recommendations: the day before the colonoscopy, breakfast, lunch and dinner until 16:00 according to the list of permitted foods. On the day of colonoscopy, from morning to 12:00 - only permitted liquids.
Stage 3. Taking the drug
To date, the recommendation of all European and American endoscopic communities is ONLY two-day separate (split) preparation.
If you have chosen the drug " MOVIPREP" .
1 day before colonoscopy.
On this day, the preparation is the same, both for colonoscopy in the morning and in the evening.
From 18:00-20:00 2 liters of liquid are taken.
1 liter of the drug "Moviprep", having previously dissolved two sachets in 1 liter of water - one small and one large. This liter is drunk gradually, over an hour. Every 10 minutes, take a glass, not in one gulp.
1 liter of liquid is required, also gradually over an hour, a glass every 10 minutes - this can be low-fat transparent broth, weak black tea without milk, compote without berries, clarified juice without pulp, non-alcoholic uncolored transparent drinks, water.
Day 2. On the day of the colonoscopy :
5 hours before the start of the study, take 2 liters of liquid as on the first day, depending on the time of your colonoscopy (see table).
| Time of your colonoscopy | Time to take 2 liters of the drug on the day of colonoscopy |
| 8.00 | 3.00-5.00 |
| 9.00 | 4.00-6.00 |
| 10.00 | 5.00-7.00 |
| 11.00 | 6.00-8.00 |
| 12.00 | 7.00-9.00 |
| 13.00 | 8.00-10.00 |
| 14.00 | 9.00-11.00 |
| 15.00 | 10.00-12.00 |
| 16.00 | 11.00-13.00 |
| 17.00 | 12.00-14.00 |
| 18.00 | 13.00-15.00 |
| 19.00 | 14.00-16.00 |
print version
TagsHealth Colonoscopy examination cleansing. movieprep
Endoscopy under sedation
Endoscopy under sedation
Sedation is a patient’s condition that most closely matches the term “medication-induced sleep.” When conducting an endoscopic examination, medications are used intravenously, which allows more precise control of the depth and duration of drug-induced sleep.
For sedation in an outpatient setting, Propofolum is most often used, which has a pronounced hypnotic effect, suppressing, among other things, the emotional component, which allows the patient to undergo the necessary procedure calmly and without fear.
When performing sedation, the effect of sleep occurs within 1-2 minutes. Medication-induced sleep during endoscopic procedures has been used for many years. Now this is a completely common and everyday technique. Patients, as a rule, tolerate it very well, regain consciousness within a few minutes after the examination and within a few hours fully return to their normal activities.
Indications for sedation during endoscopy
Sedation during endoscopy is indicated in the following cases:
- severe anxiety of the patient before the procedure;
- history of epileptic seizures;
- Parkinson's disease;
- tendency to panic attacks.
In addition, this method is preferable against the background of brain injuries and tumors affecting the central nervous system.
Special indication
to perform endoscopy under sedation is the will of the patient, caused by the reluctance to feel discomfort during diagnosis.
Preparing for endoscopy under sedation
If endoscopy with sedation is planned, then more thorough preparation for the study is necessary. A small set of mandatory examinations is carried out to assess the function of the main body systems: a general blood test (without leukemia); blood test for sugar and creatinine levels; electrocardiography (if indicated and in all patients over 40 years old).
If the patient has the results of a mandatory examination not exceeding 10 days old, the anesthesiologist-resuscitator during the consultation determines the patient’s readiness for examination under sedation, and, if necessary, prescribes additional consultations with specialist doctors, laboratory and instrumental studies in order to determine the degree of compensation for associated pathologies.
If there are no results of the mandatory examination or the period for their completion exceeds 10 days, the entire complex can be performed in the clinic as a matter of urgency before consulting an anesthesiologist. All preparatory measures serve the sole purpose of not harming the patient during the study and are carried out only if indicated.
In addition, preparation necessarily includes a certain diet. The day before the study, the patient is recommended to eat easily digestible food. The study itself is carried out on an “empty” stomach. On the day of the diagnosis, it is allowed to drink table water without gases, but no later than an hour and a half before the start of the study. In the morning, the patient must take prescribed medications for the course of treatment of existing diseases. If a joint gastro and colonoscopy is planned, then bowel cleansing (with the help of diet and laxatives) is indicated. To avoid complications, after the procedure, it is recommended to follow the diet prescribed by the doctor for a short time.
Features of endoscopy under sedation
Sedation is performed and the patient’s condition is monitored during and after it by an anesthesiologist. The study is carried out in a room specially equipped with everything necessary to monitor the patient’s condition during medicated sleep. The patient is placed on a special mobile and comfortable gurney. The anesthesiologist administers the necessary drugs intravenously. After achieving medicated sleep, the endoscopist conducts an examination. The duration of the manipulation is slightly shorter than usual. The patient awakens a few minutes after completion in a specially equipped room.
Contraindications to endoscopy under sedation
- Sedation during endoscopy is not performed if the patient has the following conditions: an allergic reaction to drugs used for anesthesia;
- hemorrhagic stroke in the last 6 months;
- signs of heart failure;
- acute myocardial infarction (or unstable angina);
- diseases of the respiratory system, which are accompanied by a decrease in blood oxygen saturation (pneumonia, bronchial asthma, COPD);
- severe anemia;
- congenital or acquired (for example, while taking medications) blood clotting disorders;
- severe renal failure (decrease in glomerular filtration rate below 30 ml/min);
- high blood pressure;
- uncompensated diabetes mellitus (a preliminary switch to insulin is required);
- unstable hemodynamics (compensation state required).
- glaucoma (risk of increased intraocular pressure);
- pregnancy period;
- recent use of alcoholic beverages or drugs;
- myasthenia gravis;
- hypercapnia (increased carbon dioxide levels in the blood);
- psychical deviations;
- sleep apnea syndrome (episodes of stopping breathing due to snoring);
- impaired liver function (cirrhosis, hepatitis, cancer).
If a patient has contraindications for anesthesia, he should pay attention to methods that will make the examination easier, or try other examination methods, for example, an x-ray of the stomach.
Possible complications
Sedation is usually easy to tolerate. The patient wakes up within 3-5 minutes after the end of the study. After which the patient continues to be under medical supervision for about another hour, and then can safely leave the clinic. On the day of the study, it is extremely undesirable for the patient to drive a vehicle or perform work that requires increased concentration or precise movements.
Among the complications most often noted:
- allergic reactions to the drug;
- dizziness;
- general weakness;
- decreased performance;
- drowsiness;
- decreased blood pressure (hypotension), increased heart rate (tachycardia); decreased clarity of vision;
- emotional lability (state of anxiety, depressed mood);
- feeling of dry mouth, hiccups, decreased appetite.
Side effects from sedation usually go away quickly, and by the end of the day the patient feels quite normal.
Gastroscopy and colonoscopy under sedation in one visit
Most often, gastro and colonoscopy are prescribed in the presence of bleeding in the digestive tract of unknown localization. These tests can be completed simultaneously during one sedation session. However, the following nuances must be taken into account:
- The time required for the diagnostic procedure will be significantly longer (usually this study takes more than an hour).
- Additional preparation is required before a colonoscopy - the use of laxatives, cleansing enemas and diet.
- Colonoscopy has its own contraindications (violation of intestinal integrity, peritonitis, diverticulitis, etc.).








