directions
Shoulder pain is not always associated with injuries caused by falls or accidents. The shoulder joint experiences a huge daily load, which, due to its anatomical structure, leads to injuries such as dislocations, subluxations, sprains, etc. The shoulder joint itself is a rather complex structure of the human body, consisting of fibers not strengthened by muscles, which allows the arms to be mobile and perform the functions of movement, rotation, tilt, extension, and flexion. At the same time, such a design leads to frequent injuries and diseases of the joint.
Currently, work is underway on the website to change the price list; for current information, please call: 640-55-25 or leave a request, and an operator will contact you.
Our clinics in St. Petersburg
Structural subdivision of Polikarpov Alley Polikarpov 6k2 Primorsky district
- Pionerskaya
- Specific
- Commandant's
Structural subdivision of Zhukov Marshal Zhukov Ave. 28k2 Kirovsky district
- Avtovo
- Avenue of Veterans
- Leninsky Prospekt
Structural subdivision Devyatkino Okhtinskaya alley 18 Vsevolozhsk district
- Devyatkino
- Civil Prospect
- Academic
For detailed information and to make an appointment, you can call +7 (812) 640-55-25
Make an appointment
We draw your attention to the schedule of technological breaks in the CT and X-ray rooms.
The nature and extent of injury, the presence of disease and pathology can be determined by such an informative diagnostic study as radiography of the shoulder.
In St. Petersburg, you can have an X-ray of the shoulder joint done in almost any medical institution - from a clinic to a hospital and a multidisciplinary medical center. But if you want to save time without wasting it in queues, or you need urgent examination and emergency medical care due to an injury, if you want to have an X-ray of the shoulder joint done with good and safe equipment, then sign up and come to the medical office. The trauma department of the clinic is equipped with the latest digital X-ray device Clinomat (made in Italy), which allows us to quickly, efficiently and fully provide all types of X-ray examinations.
Shoulder dislocation
Shoulder dislocations are the most common dislocations. The essence of the phenomenon is that the head of the humerus, under the influence of mechanical forces, loses articulation with the articular surface of the scapula and shifts to one side or another.
The anatomical structure of the shoulder joint allows the humerus a large range of motion, this joint is one of the most mobile in the body, however, the disadvantage of this is the tendency for instability of the humeral head, even despite the ligaments, tendons and its capsule that strengthen the joint, as well as the articular lip of the scapula, partially clasping the head of the shoulder. This is the reason why shoulder dislocations are much more common than others.
Normal anatomical relationships in the shoulder joint. The head of the humerus in the glenoid cavity of the scapula.
The causes of shoulder dislocation are severe trauma to the joint, when the head of the shoulder slides to the side under powerful force. Dislocation can also occur in people who engage in activities that involve repeated, range-of-motion movements of the shoulder (such as swimming or volleyball). In this case, the tendon-capsular apparatus of the joint gradually becomes overstretched and dislocation can occur even with minor impact. In addition, congenital underdevelopment of the ligamentous-tendon structures and the peculiarities of the angle of inclination of the glenoid cavity of the scapula contribute to dislocations. Typically, with traumatic shoulder dislocations, the soft tissue structures of the joint are affected, and if they are severely damaged or inadequately treated, dislocations can recur even under minimal impact (for example, lifting your arm up to straighten your hair). This phenomenon is called habitual shoulder dislocation. The problem is that instability of the shoulder leads to increased wear and tear of the cartilage of its head, that is, to arthrosis of the shoulder joint.
Shoulder dislocations can occur in different directions, but the most common is anterior dislocation, often accompanied by a separation of the anterior part of the labrum. A similar injury to the lip is called a Bankart injury (named after the English surgeon Arthur Sidney Bankart)
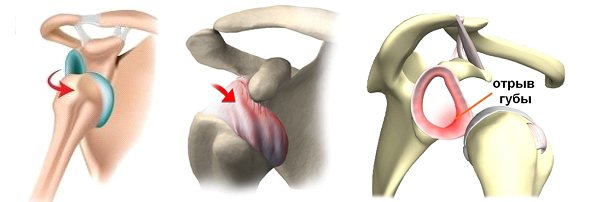
In some cases, at the moment of rolling over the edge of the shoulder blade, the head of the humerus can, in addition to the cartilaginous lip, tear off a fragment of its bone tissue. In this situation, it is customary to speak of a Bankart bone injury.
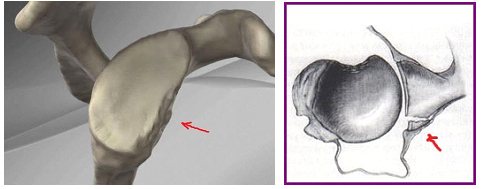
Diagram of a Bankart bone lesion. The location of the marginal scapula fracture is marked with red arrows.
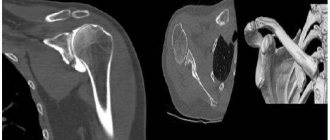
Radiological image (CT) of a bony Bankart lesion (lower right arrow).
However, at the moment of rolling, injury may occur not only to the shoulder blade, but also to the head of the shoulder itself. The fact is that under the articular cartilage of the head lies a relatively soft spongy bone that can be crushed under mechanical stress, which leads to the so-called depressed (impression) Hill-Sachs fractures (after the names of the American surgeons who described them) or to cartilaginous fractures of the head of the humerus (small Hill-Sachs).

On the left image (x-ray), the arrow indicates an impression fracture of the humeral head, on the middle and right - a fracture of the cartilage of the humeral head (intraoperative arthroscopic picture).
Treatment of primary traumatic shoulder dislocations is usually non-surgical and comes down to wearing a bandage, physiotherapy and strengthening exercises. When a habitual shoulder dislocation or chronic instability develops, preference is given to a surgical approach, the technique of which is selected based on diagnostic findings, the clinical picture and the patient’s requirements for the final result (for some, everyday stress is enough, for others, they plan to return to sports).
For typical (cartilaginous) isolated Bankart lesions, the method of choice is refixation of the labrum to the site of the avulsion. Currently, the operation is performed arthroscopically. As a fixator, absorbable or non-absorbable anchors are used, which are inserted into the bony edge of the scapula, and the torn lip is attracted to them with threads.

From left to right: refixation scheme, radiologically determined fixators and arthroscopic picture of the suture according to Bankart (1-articular surface of the scapula, 2-lip with sutures, 3-head of the humerus)
In cases of Bankart bone damage, a number of operations have been proposed, but the most common and generally giving the lowest percentage of relapses is the Latarjet-Bristow operation, the principle of which is quite simple, but the low-traumatic performance of which requires a highly qualified surgeon.

The essence of the Latarget-Bristow operation is to cut off the coracoid process (coracoid) of the scapula and move it with the blood-supplying muscle pedicle to the anterior edge of the articular surface of the scapula, followed by fixation with screws. Thus, the displaced fragment fills the bone defect and prevents the head of the humerus from excessively moving anteriorly and dislocating.
In cases of Hill-Sachs injury, treatment tactics are varied. There are many classifications of Hill-Sachs fractures by area and depth of impression (Rowe, Franceschi, Calandra et all., Flatow-Warner, etc.), but in general the choice of method depends on the extent of the damage, the presence of pain, instability in the joint and associated injuries ( for example, the same Bankart injury). As a rule, if the damage is considered clinically significant, surgical treatment is chosen, the goal of which is to restore normal or at least acceptable biomechanics of the joint. Existing techniques include plastic surgery of the joint capsule, elevation of the depressed surface of the humeral head, replacement of the defect with one’s own or cadaveric bone tissue, replacement with a metal implant, and if instability persists, Bankart or Latarget-Bristow surgery is added.

From left to right: bone defect on the articular surface of the humeral head, intraoperative picture, final radiograph.

A. Bone defect of the humeral head. B. Collection of cadaveric graft. C. Insertion of the graft with screw fixation. D. Final radiological picture.
Replacement of the Hill-Sachs defect with a cadaveric allograft with the addition of the Latarjet-Bristow operation. Postoperative radiograph (skin staples).
Surgical outcomes for shoulder dislocation vary. The result depends on the nature and extent of the injury, the chosen intervention, rehabilitation measures and the patient's requirements for the function of the shoulder joint.
In what cases is an x-ray examination of the shoulder prescribed?
An X-ray of the shoulder joint is prescribed by a doctor if there is a suspicion of a fracture of the neck (surgical and anatomical) of the humerus, dislocation of the head of the humerus, damage to the clavicle, the presence of joint diseases such as arthritis, osteoarthritis, etc. X-ray of the shoulder joint is also done in case of restriction of movement of the upper limb, pain during movement, swelling, crunching, injury (suspicion of dislocation or fracture) of the shoulder, to exclude tumor processes, foreign bodies, malformations and congenital pathologies, etc.
Main types.
The classification is quite extensive and is carried out according to various indicators. It is customary to distinguish congenital (with joint dysplasia) and acquired types over time. The latter is divided into:
- Primary traumatic. Accounts for more than 50% of the instability. Occurs when the upper limb is hit, falls on the shoulder, or jerking movements. Athletes are at risk.
- Habitual. Occurs due to unstable joint function. The cause may be an untreated injury (fracture, capsule disruption), as well as connective tissue dysplasia, muscle weakness when there is a load on the joint.
Dislocations are also classified by location:
- 1. Front. One of the most common, accompanied by a displacement to the front of the shoulder. Its consequence is a Bankart injury - a separation of the anterior part of the labrum.
- 3. Rear. Characterized by a backward shift. An uncommon occurrence, it occurs when a person falls on his arms extended forward. As a result, the posterior part of the labrum may become damaged.
- 3. Lower. In this case, the victim is unable to return the limb to its natural position and holds it above the body. The injured part moves downwards.
According to the time that has passed since the injury, dislocations are distinguished:
- Fresh (up to three days).
- Stale (from three days to three weeks).
- Old (more than three weeks old).
The success of subsequent treatment and recovery depends on this indicator.
What does an x-ray of the shoulder joint show?
On an X-ray of the shoulder joint, the radiologist will be able to see various damage caused by injuries or diseases, confirming or refuting the diagnosis. For example, X-ray signs of diseases such as arthrosis, arthritis, etc. clearly visible on an x-ray of the shoulder. The doctor will be able to examine in detail and evaluate the condition of the humerus, scapula, the distance between the bones that form the joint, the contours and condition of the joint space, etc. Based on the X-ray findings, the attending physician makes a diagnosis and develops a treatment regimen.
What to do if these symptoms occur?
If the patient has every reason to believe that he has a dislocation, then the first step is to contact a specialist. You cannot adjust the joint yourself, as this can lead to dire consequences: even greater trauma to the joint tissue, nerve damage, loss of motor function and sensitivity of the upper limb. Only a specialist can correctly assess the injury and prescribe the appropriate course of treatment. The sooner the victim is seen, the easier it is to solve the problem and the greater the chance of avoiding complications. As the day passes, muscle contraction will occur, making it more difficult to act promptly on the affected area. When transporting the patient to a doctor's appointment, the limb should be fixed in the position in which it was dislocated. You should not perform a reduction if the victim cannot return it to the reverse position on his own. To reduce pain, apply a cold compress to the injury site. To make an accurate diagnosis, it is necessary to explain in detail how exactly the incident happened.
The procedure for performing an X-ray examination of the shoulder joint
When performing an X-ray of the shoulder joint, the patient must undress to the waist. Depending on the type of projection (direct or lateral), the patient lies on a special table, or the picture is taken in a standing position. The patient is covered with a lead apron, which protects the person from the negative effects of X-rays. The duration of the procedure is several minutes. After this, the image is processed, a radiologist describes the image and issues a conclusion, the patient is sent to the attending physician or to recommended specialists.
Contraindications for diagnosis
Pregnant women
Most diagnostic tests, with the exception of ultrasound, are contraindicated for pregnant women. It is undesirable to take an X-ray, since its ionizing radiation can negatively affect the development of the fetus and cause serious pathologies in it. In exceptional cases, an x-ray of the shoulder joint may be prescribed to a pregnant woman if this is a vital indication. Only the patient's shoulder area is exposed to irradiation, and the rest of the body is carefully covered with a special vest or apron.
Children up to three months
A fragile child's body is much more susceptible to negative X-ray radiation than an adult's body. The main danger is the possible malignant degeneration of tissue cells that fall into the irradiation area. Just as in the previous case, radiography of the shoulder joint is prescribed only if absolutely necessary. X-rays are allowed for children over 14 years of age.
When undergoing other X-ray examinations on the same day
X-rays should not be done frequently. Repeating this procedure twice a day is prohibited.
If there are foreign metal bodies in the joint area
Metallic elements can reflect X-rays and prevent them from reaching the film on which the image is taken. Patients whose joints have fixing bolts or who have metal prostheses installed are not sent for an x-ray, since the information content of the resulting image will be minimal.
Clinical picture
The main problem with shoulder subluxation is instability of the glenohumeral joint. The anatomy of this joint allows for a large range of motion, which is accompanied by a loss of stability. A study conducted by Basmajian determined that the supraspinatus muscle and also the posterior fibers of the deltoid muscle play a key role in preventing humeral subluxation. Chaco and Wolf also confirmed in their study that the supraspinatus muscle is very important in preventing inferior subluxation of the humerus. Shoulder subluxation occurs during abduction and external rotation.
Other studies indicate that the most important ligamentous structure for maintaining proper alignment of the humerus and also for preventing shoulder subluxation is the inferior glenohumeral ligament. This ligament is most important in external rotation and abduction during the throwing movement.
Shoulder subluxation can lead to soft tissue damage because traction can occur due to gravitational forces and a weak shoulder provides poor protection. This is usually quite painful and may be accompanied by partial numbness in the shoulder, arm and hand.
Rating scales
Oxford Shoulder Instability Test (OISS)
The OISS is a 12-item questionnaire with five correct Likert responses for each question and has a range from 0 to 48 (with a score of 48 indicating better shoulder function). The OISS was developed and validated to assess shoulder instability and has also been tested to assess sensation in patients with shoulder instability.
Western Ontario Shoulder Instability Index (WOSI)
The WOSI is a 21-item questionnaire with a 100 mm horizontal visual analogue scale below each patient response question and ranges from 0 to 2100 as a percentage, with 100% representing the best possible shoulder-related quality of life. The WOSI is a carefully developed and evaluated instrument for patients with shoulder instability that has been demonstrated to have excellent sensitivity for posterior instability.