1.General information
Familiar to many phrases, “They found protein in a urine test,” in medical language it sounds briefly: proteinuria. This is what is called the increased concentration of polypeptide amino acid compounds, proteins, in the composition of urine excreted from the body.
Most often, a patient who has laboratory-diagnosed proteinuria first thinks about something like a urogenital infection or kidney inflammation - and indeed, in many cases the reason lies precisely in this. However, the most well-known existing classifications of proteinuria (according to Bergstein, Robson, etc.) number over twenty different types and types, divided into several large groups. There is also a separate nosological code in the International Classification of Diseases: N06, “Isolated proteinuria with specified morphological lesion,” which, in turn, suggests a number of subtypes.
An increased protein content in the urine may be a physiological, natural reaction of the body to certain conditions - a transient reaction, not associated with any pathology of the urinary system and leaving no consequences. However, in most cases, this is still a symptom, a sign of nephrological trouble, which (even in the absence of other symptoms, or, more accurately, especially in this case) requires further research and clarification.
A must read! Help with treatment and hospitalization!
Publications in the media
Proteinuria is the excretion of protein in the urine in an amount of more than 50 mg/day, the most common sign of kidney damage.
Classification • Organic - due to kidney pathology, less often - extrarenal pathology • Functional (not associated with kidney disease) •• Orthostatic •• Lordotic •• Physical stress •• Fever •• Stressful •• Cold •• Idiopathic •• Obesity (with body weight more than 120 kg) • By protein composition •• Selective - represented by a protein with a molecular weight of less than 65,000 Da (mainly albumin) or a protein of a certain molecular weight (Bence-Jones protein in myeloma nephropathy) •• Non-selective - medium- and high molecular weight protein • Degree of proteinuria •• Microalbuminuria - less than 30 mcg/day •• Minimal - less than 1 g/day •• Moderate - 1-3 g/day •• Massive (nephrotic) - more than 3-3.5 g/day ( leading sign of nephrotic syndrome). Etiology • Glomerular proteinuria •• Glomerulonephritis •• Renal amyloidosis •• Diabetic glomerulosclerosis •• Renal vascular thrombosis •• Hypertension •• Congestive kidney • Tubular proteinuria •• Pyelonephritis •• Interstitial nephritis •• Urolithiasis •• Gouty nephropathy •• Kalipenic kidney •• Acute tubular necrosis •• Chronic renal graft rejection •• Fanconi syndrome • Overflow proteinuria •• Myeloma nephropathy (Bence Jones proteinuria) •• Myoglobinuria (long-term crush syndrome) •• Lysocymuria (leukemia) •• Hemoglobinuria (intravascular hemolysis). Pathogenesis. Increased filtration of protein from plasma through the glomerular filter (glomerular proteinuria, overflow proteinuria) and/or decreased tubular reabsorption of filtered protein (tubular proteinuria). Pathomorphology • Renal proteinuria - depends on the underlying disease •• Immune inflammation in glomerulonephritis •• Deposition of amyloid masses in renal amyloidosis •• Thickening of the glomerular basement membrane, expansion of the mesangium in diabetic glomerulosclerosis • Extrarenal proteinuria and overflow proteinuria - dystrophic changes in the tubular epithelium are possible • Functional proteinuria - no changes.
Clinical manifestations • Caused by the underlying disease • Possible foamy urine with massive proteinuria • Proteinuria can be a symptom of acute nephritic or nephrotic syndromes; with a relatively rapid, abrupt increase, it acts as a sign of increased activity of glomerulonephritis. Diagnostics • Detection of the fact of proteinuria •• Using strips, precipitation with sulfosalicylic or trichloroacetic acid with refractometry (methods allow you to determine the protein concentration > 20 mg / day) •• Biuret method (azotometric) •• Radioimmune method (allows you to detect prealbumin, albumin, transferrin, 2-microglobulin, 2-macroglobulin, -globulin, etc.) • Clarification of the degree of proteinuria (study of protein in daily urine) • Clarification of the nature of proteinuria - Bence-Jones protein, 2-microglobulin, myoglobin, etc.
Differential diagnosis . Determination of the glomerular or tubular nature of proteinuria. Detection of functional proteinuria. Treatment • With functional proteinuria, there is no need for treatment • Organic proteinuria •• With glomerular proteinuria - protein restriction in the diet •• Drug treatment is determined by the underlying disease.
ICD-10 • N06 Isolated proteinuria with specified morphological lesion • N39.1 Persistent proteinuria, unspecified • N39.2 Orthostatic proteinuria, unspecified • O12 Pregnancy-induced edema and proteinuria without hypertension • O14 Pregnancy-induced hypertension with significant proteinuria • R80 Isolated proteinuria
2. Reasons
The concentration and composition of proteins excreted by the urinary tract depends on a number of factors. Thus, transient and relatively normal proteinuria is a reaction to elevated temperature or physical activity, as well as orthostatic proteinuria caused by prolonged standing (usually found in adolescence and young adulthood). The protein level also increases with hematuria, i.e. in the case of the presence of blood in the urine, which can no longer be considered a normal phenomenon. In addition, the so-called False-positive laboratory results of proteinuria can be a consequence of taking antibiotics, sulfonamides, iodine-containing drugs (for example, X-ray contrast agents). In some cases, the reason for the increased protein concentration cannot be determined at all, and it remains to be assumed that the material submitted for analysis was somehow contaminated. The most common of the purely pathological causes of proteinuria are disturbances in the complex processes of blood filtration in the kidneys, in particular in the glomerular formations, or glomeruli. With glomerulonephritis and other kidney diseases, the permeability of the glomerular capillary membrane walls can increase significantly, and, accordingly, much more proteins (albumin, transferrin, etc.) penetrate into the urine than is provided by nature. However, not only glomerular structures are responsible for filtering polypeptides, and with tubular pathology (pyelonephritis, acute necrosis, etc.) proteinuria can also be observed.
The concentration of protein in the urine increases significantly and persistently during developing oncological processes and some hereditary metabolic diseases, as well as during drug addiction, intoxication with heavy metal compounds, potassium deficiency in the urine, and excess vitamin D in the body.
Visit our Nephrology page
Proteinuria
The term proteinuria refers to an increase in protein content in the urine.
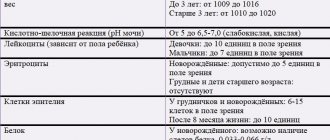
In most laboratories, when testing urine “for protein,” they first use qualitative reactions that do not detect protein in the urine of a healthy person. If protein in the urine is detected by qualitative reactions, its quantitative (or semi-quantitative) determination is carried out. In this case, the features of the methods used, covering a different spectrum of uroproteins, are important. Thus, when determining protein using 3% sulfosalicylic acid, the amount of protein up to 0.03 g/l is considered normal.
When determining the minimum amounts of protein, it is recommended to repeat the analysis; in doubtful cases, the daily loss of protein in urine should be determined. Normally, daily urine contains protein in small quantities. Under physiological conditions, the filtered protein is almost completely reabsorbed by the epithelium of the proximal tubules and its content in the daily amount of urine varies, according to different authors, from traces to 20 - 50, 80 - 100 mg and even up to 150 - 200 mg. Daily protein excretion in the amount of 30 - 50 mg/day is the physiological norm for an adult; urinary protein excretion should not exceed 60 mg/m2 of body surface per day, excluding the first month of life, when the amount of physiological proteinuria can be four times higher than the indicated values .
The general condition for the appearance of proteins in the urine of a healthy person is their sufficiently high concentration in the blood and a molecular weight of no more than 100 - 200 kDa.
transient proteinuria may appear under the influence of various factors . Such proteinuria is also called physiological , functional or benign , since, unlike pathological, it does not require treatment.
Physiological proteinuria
Transient protein excretion in the urine in healthy people may appear after heavy physical activity (long hikes, marathon running, team sports). This is the so-called working (marching) proteinuria or tension proteinuria , observed and described by many researchers. The works of these authors, illustrating the possibility of developing proteinuria under the influence of physical activity, indicate a high degree of its severity, as well as its reversibility. The genesis of such proteinuria is explained by hemolysis with hemoglobinuria and stress secretion of catecholamines with a transient disturbance of glomerular blood flow. In this case, proteinuria is detected in the first portion of urine after physical activity.
The importance of the cooling factor in the genesis of transient proteinuria was noted in healthy people under the influence of cold baths.
Albinuriasolaris is known to occur when the skin reacts severely to insolation, as well as when the skin is irritated by certain substances, for example, when it is lubricated with iodine.
The possibility of the appearance of proteinuria with an increase in the level of adrenaline and norepinephrine in the blood has been established, which explains the release of protein in the urine during pheochromocytoma and hypertensive crises.
There is alimentary proteinuria , which sometimes appears after eating a large protein meal.
The possibility of the appearance of centrogenic proteinuria in epilepsy and concussion.
Emotional proteinuria during exams has been described
Proteinuria of functional origin also includes the release of protein in the urine, described by some authors, during vigorous and prolonged palpation of the abdomen and kidney area ( palpable proteinuria ).
Feverish proteinuria is observed in acute febrile conditions, more often in children and the elderly. Its mechanism is poorly understood. This type of proteinuria persists during the period of increased body temperature and disappears when it decreases and normalizes. If proteinuria persists for many days and weeks after body temperature has normalized, then possible organic kidney disease, either new or existing, should be excluded.
In heart disease, congestive or cardiac proteinuria . As the heart failure resolves, it usually goes away.
In newborns, physiological proteinuria is also observed in the first weeks of life.
Orthostatic (postural, lordotic) proteinuria is observed in 12–40% of children and adolescents, characterized by the detection of protein in the urine during prolonged standing or walking with a rapid disappearance (transient version of orthostatic proteinuria) or a decrease in it (persistent version) in a horizontal position. Its genesis is associated with disturbances of renal hemodynamics, developing due to lordosis, compressing the inferior vena cava in a standing position, or the release of renin (angiotensin II) in response to changes in the volume of circulating plasma during orthostasis.
Physiological proteinuria is usually insignificant - no more than 1.0 g/day.
Modern research methods make it possible to identify a number of changes in the microstructure of the kidneys, the consequence of which is the so-called physiological proteinuria. Based on such considerations, many authors doubt the validity of identifying “functional” proteinuria.
Pathological proteinuria
Pathological proteinuria can be of renal or extrarenal origin.
Renal proteinuria
Renal proteinuria is one of the most important and persistent signs of kidney disease and can be glomerular , or glomerular , and tubular , or tubular . a mixed type of proteinuria develops .
Glomerular proteinuria
Glomerular proteinuria is caused by damage to the glomerular filter and occurs with glomerulonephritis and nephropathies associated with metabolic or vascular diseases. At the same time, plasma proteins are filtered from the blood into the urine in large quantities.
Various pathogenetic mechanisms underlie the disruption of the glomerular filter:
- toxic or inflammatory changes in the glomerular basement membrane (deposition of immune complexes, fibrin, cellular infiltration), causing structural disorganization of the filter;
- changes in glomerular blood flow (vasoactive agents - renin, angiotensin II, catecholamines), affecting glomerular transcapillary pressure, convection and diffusion processes;
- lack (deficiency) of specific glomerular glycoproteins and proteoglycans, leading to the loss of a negative charge by the filter.
Glomerular proteinuria is observed in acute and chronic glomerulonephritis, amyloidosis, diabetic glomerulosclerosis, renal vein thrombosis, congestive kidney, hypertension, nephrosclerosis.
Glomerular proteinuria can be selective or non-selective depending on the severity of damage to the glomerular filter.
Selective proteinuria occurs with minimal (often reversible) damage to the glomerular filter (minimal change nephrotic syndrome) and is represented by proteins with a molecular weight of no higher than 68,000 - albumin and transferrin.
Nonselective proteinuria is more common with more severe filter damage and is characterized by increased clearance of medium- and high-molecular plasma proteins (urine proteins also contain alpha2-globulins and gamma globulins). Nonselective proteinuria is observed in nephrotic and mixed forms of glomerulonephritis, secondary glomerulonephritis.
Tubular proteinuria (tubular proteinuria)
Tubular proteinuria is associated either with the inability of the tubules to reabsorb proteins that have passed through the unchanged glomerular filter, or due to the release of protein by the epithelium of the tubules themselves.
Tubular proteinuria is observed in acute and chronic pyelonephritis, heavy metal poisoning, acute tubular necrosis, interstitial nephritis, chronic kidney transplant rejection, kalipenic nephropathy, and genetic tubulopathies.
Extrarenal proteinuria
Extrarenal proteinuria occurs in the absence of a pathological process in the kidneys themselves and is divided into prerenal and postrenal.
Prerenal proteinuria develops in the presence of an unusually high plasma concentration of low molecular weight protein, which is filtered by normal glomeruli in quantities exceeding the physiological capacity of the tubules for reabsorption. A similar type of proteinuria is observed in myeloma (low molecular weight Bence Jones protein and other paraproteins appear in the blood), with severe hemolysis (due to hemoglobin), rhabdomyolysis, myopathy (due to myoglobin), monocytic leukemia (due to lysozyme).
Postrenal proteinuria is caused by the release of mucus and protein exudate in the urine due to inflammation of the urinary tract or bleeding. Diseases that may be accompanied by extrarenal proteinuria are urolithiasis, kidney tuberculosis, kidney or urinary tract tumors, cystitis, pyelitis, prostatitis, urethritis, vulvovaginitis. Postrenal proteinuria is often very minor and practically less important.
Proteinuria severity
Depending on the severity, mild, moderate and severe proteinuria are distinguished.
Mild proteinuria (from 300 mg to 1 g / day) can be observed with acute urinary tract infection, obstructive uropathy and vesicoureteral reflux, tubulopathies, urolithiasis, chronic interstitial nephritis, kidney tumors, polycystic disease.
Moderate proteinuria (from 1 to 3 g/day) is observed in acute tubular necrosis, hepatorenal syndrome, primary and secondary glomerulonephritis (without nephrotic syndrome), and the proteinuric stage of amyloidosis.
Severe or severe proteinuria is defined as a loss of protein in the urine exceeding 3.0 g per day or 0.1 g or more per kilogram of body weight in 24 hours. Such proteinuria is almost always associated with dysfunction of the glomerular filtration barrier in terms of protein size or charge and is observed in nephrotic syndrome.
Detection and quantitative assessment of proteinuria are important both for diagnosis and for assessing the course of the pathological process and the effectiveness of treatment. The diagnostic significance of proteinuria is assessed in conjunction with other changes in the urine.
Laboratory Diagnostics Doctor, Central House of Writers
Novopolotsk city hospital
Kostyuk K.S.
3. Symptoms and diagnosis
Proteinuria is situational, transient, and does not have an independent clinical picture. In cases where protein in the urine increases as a result of a pathological process, the symptoms of the underlying disease dominate, and, again, there is no need to talk about the clinic of proteinuria as such.
A daily protein output of about 0.03 grams is considered normal. If this level in a clinical urine test is significantly exceeded (and no obvious reasons for this can be found), a repeat test will be prescribed. If he also reveals proteinuria, then even in the absence of any subjective complaints, a thorough examination by a nephrologist and, possibly, related specialists will be required, since it is unreasonable and, moreover, dangerous to neglect such phenomena.
In medicine, the special term “nephrotic syndrome” is used, which implies a combination of proteinuria with a low protein content in the blood and a simultaneous increase in the concentration of lipids (fats) in the blood and urine.
About our clinic Chistye Prudy metro station Medintercom page!
Notes from a laboratory assistant. Protein in urine (proteinuria)
Authors : Kuznyak Irina
Proteinuria (the presence of protein in the urine) is a pathology at any age, under any conditions and conditions of the body. Another thing is that some types of proteinuria disappear without a trace, being only a consequence of a superload (infections with hyperthermia, for example) on the body, but without pathology in the kidneys themselves. But even with kidney pathology, the protein will not always be in the TAM (if remission is successfully achieved). All doctors know this and, depending on the specific patient, make a decision: to observe (until normalization of the TAM) or to conduct further examination of the renal system.
There are many types of proteinuria: renal (true), non-renal (false), orthostatic (lordotic), organic (damage to the kidney parenchyma), functional (without damage to the kidney tissue, a consequence of ice douches and superhuman stress in sports), physiological (in newborns), nutritional (especially for lovers of raw eggs). Under no circumstances even try to figure out what type of proteinuria you have! There is a rule: if protein is detected in the urine, you must consult a doctor. This is so serious that we can say: protein in the urine is the most important indicator in OAM. Therefore, do not ignore this point in the analysis results if you do not want to raise a patient in hemodialysis departments at an advanced age.
In private laboratories it is customary to express urine protein in MG/L, in public laboratories - in G/L. That is, 64 mg/l = 0.064 g/l.
There is also the concept of “trace protein” - this is 0.015 g/l.
If protein is detected in a general urine test, then it is necessary to check it in 24-hour urine. Determination of protein in DAILY urine is an average figure, because in a single serving could reflect protein fluctuations throughout the day. To determine the amount of protein excreted per day, the resulting protein concentration (provided that it is present, but normally it is not determined in a daily basis (not determined) by generally accepted unified methods) is multiplied by the amount of urine (in liters). They donate daily urine like this: collect it in a clean jar, starting with the second portion in the morning and ending with the first portion in the morning (take a 3-liter jar at once), the tank will have to be stored in the cold, then measure the total amount of urine collected (BE SURE TO WRITE DOWN what happened and indicate this is on the form, since the laboratory assistant also needs to multiply the amount of protein by the amount of urine excreted per day). After this, you need to mix everything and pour 50 ml into a clean container, which you will take to the laboratory.
In the general analysis, “total protein” is determined - albumins, globulins, mucus protein. There is also a diagnostic distinction between “kidney protein” and “cellular” protein in the urine. More about this: it is believed that the appearance of protein in the urine above 200 mg/l for a long time indicates the irreversibility of the process of kidney damage, but only if this protein is RENAL, that is, it has passed through the kidney filter, and is not a consequence of the destruction (presence) of cellular elements in pelvis and below (for example, leukocytes in all fields of view in the OAM) or concomitant prostatitis, bladder polyps, etc.
I always put myself in the place of the attending physician of the patients for whom I perform tests (I am happy for someone, I am upset for someone when there is a gross pathology, I sympathize with someone when it is completely unclear what is wrong with the person, and I think it’s good that it’s not me I’m treating him...), and I remember how pale I looked when I didn’t have knowledge of clinical laboratory diagnostics, but had to prescribe medications and make diagnoses based on other people’s tests. And it’s a pity for those doctors whose patients simply ignored the appointments for banal OAC and OAM, but they demand the CORRECT treatment from the doctor. Or if the laboratory “could not get into the vein”, “there is not enough blood”, “a blood clot in a test tube”...
There are several ways to determine protein in urine.
The most modern method for determining protein is pyrogallol (it is beautifully painted in different colors), it is also considered the most sensitive, but its result is 3.3 times higher than those obtained by conventional methods. And in this regard, there is often confusion in the interpretation of the results, because A milligram cannot weigh one weight on some scales, but three weights on others. In addition, it is imperative to use control solutions of not only albumin, but also globulin. The results are also affected by the use of many medications. In general, I believe that it was necessary to introduce other units of measurement in order for this to be considered a unified methodology. In the meantime, the use of this method is incorrect, since ALL laboratories in the state have not been transferred to it. After all, you can donate urine for an even more accurate diagnostic method - microalbuminuria, or MAU.
Geller's test for mild proteinuria (after measurement 0.132 g/l) and pronounced (after measurement - 19 g/l, practically serum, the renal filter almost “did not work”).
This may not be interesting, but some people confuse the Heller test (ring) and the Brandberg-Roberts-Stolnikov method (with the Ehrlich table). The Heller test is a qualitative method of determination (yes/no, that is, whether there is protein or not), and the use of dilutions with a ring test is a semi-quantitative method (Brandberg-Roberts-Stolnikov)
There is such a thing as “microalbuminuria” - this is protein in the urine of 20 mg/l, a fairly important indicator of the harbingers of incipient pathology in the glomeruli of the kidneys. Naturally, it is stupid to prescribe it if there is obvious proteinuria.
Determining protein in urine with test strips is very approximate and unreliable.
Externally, proteinuria does not manifest itself in humans in any way; edema is completely unusual.
But here is one of the cases. A 7-year-old boy recently took tests. The blood test was completely within the age norm (ESR 4 mm/h), but the urine test was simply shocking. Microscopy is scanty, normal. But his protein was 17 (!!!) g/l - it seems that this is not urine, but serum. I've never seen anything like this before. And from the clinic - lethargy and swelling on the face, which appeared a few days ago.
In the first photo, there should be a slight turbidity of varying degrees of intensity in the test tube (this is a qualitative test for protein with sulfosalicylic acid). Here it’s like chicken protein has been poured in.
On the second, there should usually be a barely perceptible (on a black background) white ring at the boundary of the media (urine of varying degrees of dilution and nitric acid). But what happened in this case was that it was necessary to dilute and dilute the urine, as in homeopathy, figuratively speaking, to “Hahnemannian dilutions”, so that this ring disappeared and the amount of protein could be determined.
Kidneys in general are “partisans” by nature; a person may not realize for many years that his kidney(s) have started a “mutiny on the ship”, and then a “bolt from the blue” will begin until it gives up OAM. But, unfortunately, it happens that they realize it is too late. It’s one thing if proteinuria was a consequence of hyperthermia, and after a week in the control TAM everything returns to normal. And it’s quite another thing if proteinuria was discovered with apparent well-being and the absence of any complaints. In any case, if in the PROTEIN column there are ANY numbers (and not “n/a”), you need to consult a doctor (even if a private laboratory has put THEIR norms in the form in the range of normal values, into which your numbers fit).
There are also albumoses in the urine and the “protein body” of Bence-Jones. But this is completely laboratory jungle, and ordinary readers are not interested.
published 06/17/2019 15:37 updated 06/17/2019 — Growth and development, Tests and examinations, Kidney and urinary tract diseases, Tests and examinations, Nephrology and urology
4.Treatment
It is easy to see that both diagnosis and subsequent therapy (if necessary) will be aimed not at proteinuria as such, but at the reasons that caused the excess presence of protein in the urine. Almost always, for kidney diseases, a special diet is prescribed (selected individually) and drugs from the group of nephroprotectors, literally “kidney protectors,” namely angiotensin-converting enzyme inhibitors (ACEIs), calcium channel blockers, statins, etc. This kind of treatment normalizes the function kidneys and, in particular, reduces the level of protein in the urine to an acceptable or normal concentration.