The diagnosis of Ureaplasma infection is made on the basis of a detailed medical history, examination, tests: urethral smear, PCR examination of urethral scraping, blood ELISA, urine test.
Today, the most informative diagnostic method for determining ureaplasmosis is the use of the PCR method. This test is used to examine samples of a patient's secretions and blood. PCR gives very high efficiency in diagnosing not only ureaplasmosis, but also a large number of other sexually transmitted diseases. If this analysis confirms the presence of ureaplasma in the smear, a culture is also required, which determines the number of bacteria in the body. It is culture that makes it possible to find out whether the presence of ureaplasma in the discharge is a pathology or is it a normal carriage. Cultures are often done along with an antibiogram. Thus, the doctor can immediately determine what types of antibacterial drugs a given type of ureaplasma is sensitive to. An auxiliary serological test can be used to isolate specific antibodies to ureaplasmosis. Useful for recurrent forms of the disease and the formation of complications.
Ureaplasma: symptoms in men
In men, signs of ureaplasmosis include chronic inflammatory processes in the prostate (prostatitis), appendages (epididymitis) or urethra. Often there is discharge from the urethra, itching and burning in this area, and pain in the lower abdomen.
With an infection caused by ureaplasma, symptoms in men may also include infertility. Ureaplasma parvum and others are able to penetrate sperm, disrupting their motility and reducing the chances of fertilization of the egg.
What does ejaculate culture show?
All bacteria, viruses and other microorganisms that can be detected in semen are divided into groups:
- symbionts - physiological microflora that does not cause harm to the human body, takes an active part in maintaining the biocenosis;
- opportunistic - do not cause harm at their normal concentrations, but can cause the development of pathology if permissible standards are exceeded. For example, staphylococcus is found in any man, but in normal quantities the microbe does not pose any threat to the body. When exposed to various endogenous or exogenous factors, the microbe can begin active division. In such situations, staphylococcus in sperm culture in large quantities may indicate the development of cystitis, urethritis, vesiculitis, prostatitis;
- pathogenic – normally such pathogens should not be present. These are foreign bacteria that enter the body during infection. The most common pathogens detected are sexually transmitted diseases.
If a particular pathogen is detected, the doctor prescribes or adjusts a treatment regimen for the infection. When you receive the result, show it to your doctor.
Ureaplasma: symptoms in women
Manifestations of ureaplasmosis may be as follows:
• Discharge from the genital tract;
• Unpleasant sensations during sexual intercourse;
• Pain in the lower abdomen, as well as in the urethral area;
• Itching in the urethra;
• Frequent inflammation of the genitourinary system and mucous membranes (vulvovaginitis, urethritis, etc.).
In pregnant women with an infection caused by ureaplasma, symptoms and complications can vary from chronic inflammation of the genitourinary organs to premature birth or infection of the fetus. Therefore, active ureaplasma during pregnancy increases the risks for the mother and the unborn child.
Patient preparation rules
U/g fence. Standard conditions:
During the working day ML "DILA".
Important:
- For 2 days before collecting the material, do not use topical medications (suppositories, douches, etc.), refrain from sexual intercourse - Refrain from urinating for 2 hours - Donate before treatment or no earlier than after 21 days after completion of the course of antibacterial, antimycotic therapy (unless otherwise determined by the attending physician).
Possible:
Deviations from standard conditions are possible in agreement with the doctor.
Attention:
The conditions for preparing for the delivery of urogenital material are determined by the doctor.
With special instructions from a doctor, it is taken in accordance with the specified collection point. Another type of BM.
Standard conditions: During the working day of ML "DILA".
Attention:
For this method, different types of biomaterial can be used (this is determined only by the customer, pointing in the direction).
You can add this study to your cart on this page
Treatment of ureaplasmosis
If ureaplasma is detected, treatment is carried out if the microbe is the cause of chronic inflammation, infertility, etc. If the cause of the disease is ureplasma, treatment is prescribed with antibiotics. The choice of antibiotic should be made by a doctor, since self-medication of ureaplasmosis often not only does not bring the desired result, but can also lead to the development of microbial resistance to the antibiotic. Thus, over the past few years, the number of tetracycline-resistant strains of Ureaplasma urealyticum and parvum has been increasing.
Of particular importance is the treatment of ureaplasma (parvum, urealiticum) in men and women when planning pregnancy. The decision to treat ureaplasma parvum and others during pregnancy is made taking into account its duration, as well as after carefully weighing the possible risks for the child and mother from ureaplasma and antibiotic therapy. Usually, they try to treat ureaplasma during pregnancy at a later stage (after 20 weeks), when the effect of antibiotics on fetal development becomes minimal.
How to protect yourself and your loved ones from contracting ureaplasma infection?
Ureaplasmosis is most often transmitted sexually. The best prevention of this disease is to adhere to the culture of sexual relations. It is necessary to beware of casual or promiscuous sexual intercourse. It is recommended to use barrier contraception such as a condom. It is with its help that you can protect yourself not only from ureaplasmosis, but also from other STDs.
Professor Azizov’s clinic employs highly professional specialists. We have all the necessary modern equipment for diagnosing and treating ureaplasma infection. We will be happy to help you solve your problem.
Doctors:
Azizov Akhmed Pirmagomedovich - urologist-andrologist, sexologist, doctor of medical sciences, professor Salimgereev Ruslan Alevdinovich - urologist-andrologist, doctor of the 1st category Isakhanov Isakhan Daudgadzhievich - urologist Azizova Muslimat Akhmedovna - obstetrician-gynecologist Gamidova Albina Abdullatipovna - obstetrician-gynecologist
Diagnosis of ureaplasmosis
To make a diagnosis, a combination of clinical picture and laboratory data is necessary. It must be remembered that ureaplasma parvum and urealyticum are opportunistic microbes, so it is not always possible to establish a diagnosis of ureaplasmosis based only on test results. Likewise, it is impossible to accurately establish the presence of the microbes Ureaplasma urealyticum, parvum and the development of the disease only on the basis of clinical data, without objective laboratory confirmation.
Culture for ureaplasma parvum and urealiticum in men and women
Culture for ureaplasma is the “gold standard” for diagnosing ureaplasma parvum and its other types. The discharge from the genitourinary tract is inoculated onto nutrient media.
When diagnosing ureaplasma in men, the following material is used for inoculating ureaplasma parvum, etc.: urethral smear, ejaculate, prostate secretion. Urine can also be used to test for ureaplasma in men.
Cultures for ureaplasma parvum and others in women are taken from smears from the vagina, urethra, and cervix. Urine in women is not used for ureaplasma testing.
If, after a certain period of time, growth of ureaplasma parvum or another type of ureaplasma parvum or its other type is obtained on a nutrient medium, then you can evaluate the result and clarify the diagnosis. Normally, the result will be negative; if there is activity of Ureaplasma parvum, etc., it will be positive. In asymptomatic carriage, culture for ureaplasma has low rates - less than 10 to 4 degrees of colony-forming units of ureaplasma/swab/ml.
Indicators above 10 to 4 degrees for ureaplasma parvum and others indicate activation of the infection. With a result of 10 to 4 degrees in culture for ureaplasma and higher, its sensitivity to antibiotics is determined. When indicators are greater than 10 in 4 CFU/swab/ml in culture for Ureaplasma parvum and other microbes, the microbe is tested for sensitivity to different types of antibiotics, assessed quantitatively, as well as by the nature of colony growth. If culture indicators are more than 10 to grade 4 for ureaplasma, treatment (choice of antibiotic) will depend on these characteristics.
Cultures for ureaplasma parvum and others are carried out not only if a urogenital infection is suspected, but also to monitor the effectiveness (if ureaplasma was detected) of treatment (approximately at the end of the second week after discontinuation of the drug). The success of treatment can be judged by the titer. If the culture result reveals a titer of less than 10 to 4 degrees for ureaplasma, then there is a significant positive effect of treatment. If the titer is more than 10 to 4 degrees for ureaplasma, then correction of treatment and its continuation is necessary.
Analysis methods
Depending on the symptoms, the doctor decides which biomaterial to donate (blood, urine, smear, scraping) and what method it will need to be examined. Let us tell you in more detail about the most reliable and frequently prescribed types of biomaterial tests for ureaplasmosis [9,10].
- Cultural method (bacteriological culture) . This analysis method is used to detect ureaplasma more often than others. Its essence lies in placing biomaterial (a smear from the cervix or the mucous membrane of the urethra, less often urine or prostate secretion) in a special nutrient medium. If there are ureaplasmas in the material, they begin to actively multiply, which is recorded by a specialist. Bacterial culture is also used to determine the sensitivity of infectious agents to various types of antibiotics (for prescribing a specific drug). This method has a high level of accuracy, but you will have to wait quite a long time for results - from four to eight days.
- PCR . Polymerase chain reaction is one of the most accurate (method sensitivity is about 96%)[11] and fastest tests for ureaplasmosis today. The result of the laboratory test can be obtained within four hours. For analysis, vaginal discharge and urine are usually taken. PCR allows you to find sections of the RNA of the causative agent in the body, even if the microorganisms are contained in the sample in minute quantities. However, the method has its drawbacks: it does not provide (unlike culture) information about the activity of ureaplasmas, and may be false positive (if the sample is contaminated) or false negative (for example, if a person was treated with antibiotics less than a month before the test).
- ELISA. Enzyme immunoassay is carried out by placing biomaterial (in this case blood) on a special strip with antigens of the pathogen. The study does not show the presence of microorganisms themselves, but the presence of antibodies in the sample. For each infection, special immune proteins are produced, so the diagnosis based on the test result can be made with a high degree of accuracy. It usually takes no more than one day to get results. The disadvantage is that test results within a given infection cannot always be accurately interpreted. The study is rather of an additional nature, so it is unacceptable to use it as a leading test in establishing the diagnosis of ureaplasmosis.
All these methods of testing for ureaplasma are considered quite accurate and reliable. Although the latter indicator strongly depends on the quality of the biomaterial, which is influenced, among other things, by the patient’s compliance with the rules of preparation for the study.
How to submit biomaterial for analysis for ureaplasma
If the patient donates blood, the procedure is performed on an empty stomach, in the morning. When studying by molecular biological methods, the first portion of freely released urine is collected. When taking a scraping from the urethra, a man will have to refrain from going to the toilet two hours before the examination. Women do not undergo a scraping (nor do they take a smear) during menstruation. Both sexes should avoid sexual intercourse for two to three days before the test.
To take a smear or scrape, the patient can perform genital hygiene the evening before the test, but not later. You should not use any ointments or gels.
There are additional rules for ladies. A few days before taking a smear test for ureaplasmosis, you should not use local contraceptives (suppositories, ointments, vaginal tablets)[12], douche, or wash yourself with hot water.
Both women and men need to remember that when taking any test for ureaplasmosis, you cannot take antibacterial drugs. If such drugs were taken less than a month before the study, it is necessary to warn the doctor about this [13].
Decoding the analysis for ureaplasma: norm and pathology
After the patient has been tested for ureaplasma, the doctor determines the presence of the disease based on normal values. It is worth remembering that the presence of ureaplasma or other foreign microorganisms in the body does not mean that a person is sick and needs treatment. Additional tests may be required to determine the presence of an inflammatory process.
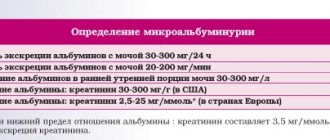
During PCR diagnostics, the amount of ureaplasma RNA in the sample should not exceed 104 CFU per 1 ml; if the titer is higher, this indicates the presence of pathological activity of microorganisms. The same figure is considered the norm for the result of the cultural method of analysis (seeding).
If ELISA was chosen as an additional research method, then the titer (the amount of antibodies in the sample) will be indicated on the form and, ideally, the word “normal” should appear next to it. The specifics of the analysis may vary in different clinics, therefore the normal figure may be different. You need to focus on the reference values given by the laboratory. There are also situations when the result obtained is considered doubtful, then the patient is prescribed another test.
Testing for ureaplasmosis is just one of a large list of preventive tests that a person should undergo at least once a year. Particular attention should be paid to the issue for people at risk (those with weakened immune systems, those who frequently change sexual partners, those who have had pelvic diseases) and those suffering from infertility.
Test for antibodies to Ureaplasma urealyticum, parvum IgG, IgA, IgM
Ureaplasma parvum and urealiticum, as opportunistic organisms, weakly provoke immune reactions. Therefore, it is not always possible to detect antibodies to Ureaplasma urealyticum and parvum in the blood. If ureaplasmosis is suspected, this type of study is auxiliary and can provide some additional information on the nature of the infection.
Antibodies to Ureaplasma urealyticum, parvum of the IgG class indicate the presence of immunity against ureaplasma parvum or urealyticum. IgG to Ureaplasma urealyticum, parvum can be detected in the complete absence of clinical symptoms. An increase in the titer of IgG antibodies to Ureaplasma parvum and others in paired sera taken at a two-week interval indicates a current infection. IgA to ureaplasma parvum and urealiticum is also found in some healthy people. But if within two weeks there is an increase in already high IgA titers, you can think about a current infection caused by ureaplasma parvum or others.
Detection of DNA from Ureaplasma urealyticum, parvum
It is carried out using the PCR technique, which makes it possible to detect microbial DNA particles present in a material sample in quantities above threshold values. A positive test result occurs in the presence of infection, or in carriers of ureaplasma when there are no symptoms.
If there is an infection that could be caused by ureaplasma, treatment is carried out after laboratory confirmation. To obtain an accurate result, laboratory tests for ureaplasma parvum and others must be carried out in combination.
How to prepare
Proper preparation for bacteriological seeding of sperm.
- toilet of the penis and hands (soap + water)
- sexual abstinence 2 days (48 hours);
- the day before the study, do not eat salty, hot, spicy foods, or alcoholic drinks. The same applies to all medications that contain ethanol;
- When taking antibiotics, a sperm sample is given 2-3 weeks after the end of the dose.
- masturbate and collect ejaculate in a container without touching the walls of the container