Assessment of external respiration function plays an important role in the diagnosis of a large number of diseases of the lungs and bronchi, making it possible to detect changes even before the appearance of their first signs, and to determine the dynamics of changes during treatment. For this purpose, different methods are used today, but one of the most informative and at the same time safe is spirography.
What is spirography
Spirography or spirometry is a diagnostic method for studying the function of external respiration and is the main way to assess the functional state of the lungs and bronchi. It is widely used in pulmonology and therapy, since it allows you to establish:
- the volume of air inhaled and exhaled, which is called the tidal volume of the lungs;
- what is the maximum volume of air a person can calmly exhale with a deep breath, i.e. vital capacity of the lungs (VC);
- the volume of air exhaled during a full exhalation after taking the deepest possible breath, which is called forced vital capacity (FVC);
- the volume of air remaining in the lungs after a quiet exhalation (functional residual capacity) and after a forceful exhalation;
- total lung capacity;
- forced expiratory volume in the 1st second of exhalation (FEV1) with extremely deep inspiration and forced expiration;
- instantaneous, peak volumetric velocity;
- minute volume of breathing, i.e. the amount of air entering the lungs per minute;
- maximum productive pulmonary ventilation (MPV) - a completely individual indicator showing breathing patterns for 1 minute;
- breathing frequency, i.e. the number of respiratory movements performed per minute.
Additionally, the Tiffno index (IT) is determined, which is the ratio of FEV1/FVC.
Thus, spirography provides a large amount of information about the functioning of the respiratory organs of a particular patient, which allows not only to detect signs of pathological changes, but also to develop the most effective treatment tactics. As a result, it is possible to discover:
- airway obstruction;
- the severity of the current disease;
- signs of bronchial asthma and chronic obstructive pulmonary disease (COPD);
- hidden bronchospasm;
- a number of diseases of the respiratory and cardiovascular systems;
- disorders caused by certain neurological diseases.
The procedure can be performed on children as young as 5 years old. But due to age, it does not always turn out to be informative, since it can be difficult to explain to a child what is required of him, especially when performing forced exhalation.

Expert Opinion of a Doctor
Currently, many are worried about the consequences of a coronavirus infection: fatigue, decreased performance, complications such as lung damage. The sooner rehabilitation begins, the better the recovery results will be.
Pak Andrey Igorevich
Neurologist, chiropractor
Experience: 1 year
How is the treatment carried out?
What methods are used
To assess respiratory function, the most common methods used are:
- spirometry;
- spirography;
- peak flowmetry;
- body plethysmography;
- analysis of the gas composition of air.
The use of these methods makes it possible to estimate lung volume (residual, vital, minute, forced), expiratory flow (peak and maximum).
Additionally, functional tests are used, which allow one to evaluate the parameters of external respiration when using provocative tests, stress tests with physical activity, as well as when using bronchodilators.
Indications for spirography
Since spirography is a safe and fairly simple diagnostic method, it is widely used in pulmonology, as well as in therapy for suspected pulmonary diseases. Namely, it is prescribed for:
- prolonged cough, persisting for more than 3-4 weeks, for no apparent reason, including after suffering from bronchitis or ARVI;
- diagnosing diseases of the respiratory system by other methods;
- presence of a feeling of pressure and heaviness in the chest, shortness of breath;
- difficulties when inhaling/exhaling;
- disruption of gas exchange processes;
- audible whistling or wheezing during inspiration;
- frequent bronchitis, attacks of shortness of breath, difficulty breathing;
- suspected of having Goodpasture's syndrome, scleroderma.
Spirography is also recommended for anyone who has a long history of smoking.

Spirography is also indicated for preventive purposes. Therefore, it is included in the list of mandatory studies to be performed during the annual preventive medical examination. In addition, it is prescribed to people working in hazardous industries and children with close relatives who have chronic respiratory diseases or allergic reactions manifested by bronchospasm. It is also used to make adjustments to the treatment of bronchial asthma and COPD.
Features of preparation
To obtain the most accurate data, spirography requires simple preparation. Thus, you should refrain from eating food 6-8 hours before the test, so the test is usually scheduled for the morning. It is also not recommended to drink strong tea or coffee or smoke before the procedure. The day before, you should have a light dinner and avoid alcohol and energy drinks. It is allowed to drink a glass of warm water an hour before the examination. In addition, it is better to refuse morning exercises, if such is practiced.
You should come to spirography in loose, comfortable clothes that do not restrict breathing. Therefore, it is better not to wear a tie, tight underwear, etc. The procedure itself is carried out approximately 20 minutes after the patient arrives at the clinic. This time is required for the functioning of the respiratory and cardiovascular systems to fully normalize after physical activity.

On the recommendation of your attending physician, before spirography, you should take a break from using bronchodilators, which are often prescribed for bronchial asthma, COPD and other obstructive respiratory diseases. Thus, the use of short-acting β2-antagonists, in particular Salbutamol, Ventolin, Berodual, should be discontinued at least 6 hours before spirography. Inhalations of long-acting β2-antagonists, i.e. Seretide, Foster, Foradil, Symbicort, Serevant and the use of Oxis must be carried out no later than 12 hours before the study. As for long-acting theophyllines, for example, Spiriva, the drug is discontinued one day before spirography. But you should stop taking these medications only in consultation with your doctor.
Sign up for spirography in Moscow
In our clinic, you can undergo an FVD examination with interpretation for a fee and immediately after receiving the results, consult a doctor for diagnosis and treatment planning. The doctor will analyze test data and medical history and develop optimal treatment tactics.
You can sign up for the procedure in Moscow at the address: Komsomolsky pr., 17, building 11. At the Alfa Health Center clinic, examinations are carried out in comfortable conditions. Friendly administrators will meet you, answer your questions, and show you to your office.
We have an affordable price for spirometry with interpretation. The cost of consultation with specialized specialists can be found in the price list on the website.
How is spirometry performed?
In essence, spirography and spirometry are the same thing. The only difference between these concepts is that spirometry can be called the process of performing the study, and with spirography, its result is given in the form of a graph that accurately describes the function of the lungs. Today these concepts are identical and interchangeable.
Nowadays, computer spirometry is used almost everywhere to assess respiratory function, although previously mechanical devices, usually of the water type, were used for these purposes. Modern digital devices, called spirographs, allow you to take the necessary readings in different modes and automatically calculate the necessary ratios, which significantly speeds up and simplifies diagnostics. The system additionally takes into account the patient’s weight, height, gender, and age.
Spirography can be performed during quiet breathing in order to determine the vital capacity of the lungs, during forced (sharp, strong) exhalation and with functional tests:
- a test with a bronchodilator allows you to detect hidden bronchospasm, which makes the diagnosis more accurate and allows you to better assess the effectiveness of the therapy;
- expert provocative test with methacholine - used to definitively confirm or remove the diagnosis of bronchial asthma, as it allows you to accurately detect the tendency of the bronchi to spasm and develop hyperreactivity syndrome.
The apparatus for performing spirography can be closed or open. In the first case, it has the form of a hermetically sealed transparent chamber connected to the recording part. Open devices provide inhalation of atmospheric air and consist of a computer of one size or another and a mouthpiece with sensors attached to it.
Directly performing spirography is as follows:
- the patient takes a comfortable sitting position;
- they put a special soft clothespin on his nose and give him a special mouthpiece connected to an apparatus, which must be pressed tightly to his lips;
- Initially, you should breathe calmly for 10 seconds through your mouth, inhaling and exhaling through the mouthpiece, but so that you do not have to tilt your head or stretch your neck;
- at the command of the doctor performing the procedure, you should take the deepest possible breath, and then exhale sharply and forcefully;
- at the doctor’s command, take frequent and deep breaths for 12 seconds.
To achieve the correct execution of forced exhalation, it may take 3-8 attempts, since a coughing fit, closure of the vocal cords, early stop of exhalation, and blocking of the mouthpiece lead to inaccurate results.
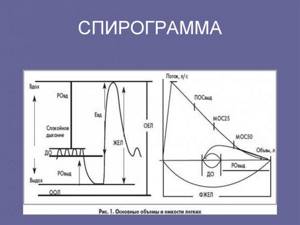
The study lasts 15-45 minutes. After the procedure is completed, the computer draws up a graph based on the results of the study, which is called a spirogram. If deviations are detected in it, the procedure is usually repeated, sometimes more than once. If the changes are persistent and persist from study to study, the patient is recommended to undergo additional diagnostic procedures or perform spirometry with a bronchodilator.
For example, in controversial cases, a study of the characteristics of lung diffusion can be performed, i.e., the quality of oxygen supply from the lungs to the blood and the removal of carbon dioxide. A change in this parameter indicates severe respiratory dysfunction. Patients may also be recommended to undergo bronchospirometry, i.e., insertion of a bronchoscope under anesthesia to assess the functionality of each lung separately, calculating its minute volume, vital volume and a number of other indicators.
In combination with spirography, ECG, ultrasound of the heart and x-ray of the lungs are often prescribed, as this makes it possible to accurately determine the presence or absence of a connection between pathologies of the bronchopulmonary and cardiovascular systems.
Decoding the results
Interpretation of research results is the task of a specialist. In this case, it is necessary to take into account not only the data obtained, but also the quality of the procedure performed, the possibility of false positive and false negative interpretation.
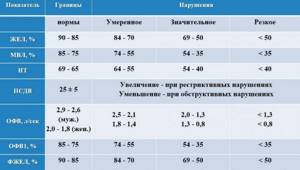
The conclusion is drawn up by comparing the obtained data with normal indicators of FEV1, VC, FVC, IT, MVL and others. In healthy people, these values are always above 80% of normal values. The presence of pathological changes is indicated by receiving data below 70% of normal values.
Breathing rate
Initially, respiratory rate indicators are assessed, i.e. the number of inhalations and exhalations made per minute. Normally, an adult makes 16-20 breathing movements per minute, children - more depending on age. This indicator is influenced by the patient’s body position during the study, the degree of emotional arousal and food consumed the day before. If these conditions for performing spirography have not been violated, an increase in respiratory rate may indicate the presence of:
- pneumonia;
- tuberculosis;
- fibrosis;
- pulmonary edema;
- pulmonary atelectasis;
- arterial thromboembolism.
If increased respiratory movements are combined with a decrease in depth, this may be a sign of dry pleurisy, acute myositis, intercostal neuralgia, rib fractures, and the presence of metastases in the lungs.
A decrease in respiratory rate is characteristic of brain lesions, in particular meningitis, tumors, cerebral edema and hemorrhages into the brain.
Tidal volume
Tidal volume (TV) - the amount of air inhaled in 1 breath. Normally, it is 0.5-0.8 l, but a diagnostic parameter is considered to be its decrease against the background of an increase in respiratory rate or vice versa. Thus, an increase in tidal volume with an increase in respiratory rate is observed at elevated body temperature or the presence of anemia. A decrease in both indicators is typical for pulmonary emphysema, severe narrowing of the trachea, and diseases that cause depression of the function of the respiratory center located in the brain.
Minute breathing volume
MVR is calculated by taking the product of respiratory rate and tidal volume. Therefore, the normal MOD in an adult is about 4-10 liters. This parameter is important for assessing the quality of ventilation of the smallest components of the lungs, the alveoli. After all, with deep and shallow breathing, the air entering the lungs fills them differently. With shallow, frequent breathing, it may not reach the alveoli, which reduces the quality of gas exchange processes in the body.
An increase in MOD indicators may indicate the development of mild to moderate pulmonary or heart failure, thyrotoxicosis, or damage to the central nervous system. A decrease in this value is a sign of severe pulmonary or heart failure, myxedema or respiratory depression.
But the MOD largely depends on the psychological state of the patient, the degree of fitness of the lungs, and metabolic characteristics. Therefore, this indicator is often perceived as auxiliary.
Vital capacity of the lungs
Vital capacity does not show the total volume of the lungs, but the maximum possible volume of air that a particular person is able to inhale and exhale, i.e. it also includes the reserve volume of inhalation and exhalation. In a healthy adult, this figure is 3000-5000 ml and is close to the proper vital lung capacity (VLC) calculated individually using a mathematical formula.
JEL for adult men = (27.63 – 0.122 x B) x L;
JEL for adult women = (21.78 – 0.101 x B) x L.
B – age in years, L – height in cm.
Normally, the difference between the obtained and calculated indicators should not be more than 15%. A larger difference is typical for:
- pneumothorax;
- lung abscess;
- Bekhterev's disease;
- tuberculosis;
- exudative pleurisy;
- pneumonia;
- pneumofibrosis;
- emphysema;
- atelectasis;
- kyphoscoliosis;
- disorders of the central nervous system;
- pathologies of the cardiovascular system.
A slight decrease in vital capacity indicates obstructive bronchial disease.
Forced vital capacity
This indicator, abbreviated as FVC, should normally be no more than 100-300 ml less than VC. With its help, you can evaluate the elasticity of the lungs, the quality of functioning of the respiratory muscles and the patency of the bronchi.
If the difference between VC and FVC increases to 1500 ml or more, the presence of:
- obstructive bronchitis;
- bronchial asthma;
- emphysema.
Forced expiratory volume in 1 second
FEV1 is an individual indicator depending on gender, age and weight. In a healthy person it should be in the range of 1.4-4.2 l/sec. But the result obtained during spirography must be compared with the expected one, which is calculated for each patient separately using the formula:
FEV1 for men = 0.036∙height – 0.031∙weight;
FEV1 for women = 0.026∙height – 0.028∙weight.
Deviation of the obtained FEV1 from the expected value is an indicator of the presence of chronic bronchial obstruction, and also allows you to monitor the dynamics of the disease.
The average volumetric velocity (AVR), which reflects the speed of forced exhalation in the middle of the respiratory movement, will help to detect obstructive diseases in the early stages of development.
Tiffno index
IT is calculated as the ratio of FEV1 to vital capacity and in healthy people it is 70-90%. This indicator decreases when:
- bronchial asthma;
- chronic obstructive bronchitis;
- emphysema.
The type of obstruction can be determined by IT. Additionally, a test with bronchodilators is carried out and, if after this test the FB increases, the reason is bronchospasm. If the situation does not change, you should look for the root of the problem in other pathologies.
Maximum ventilation
In healthy adults, MVL is 50-180 l/min. A decrease in this indicator is characteristic of the development of respiratory or heart failure.
Air speed indicators
These parameters are calculated using a rather complex algorithm, which consists of constructing a triangle on the resulting spirogram. Normal values are considered to be 160-300 mm/min.
Thus, it is impossible to make a diagnosis based on changes in only one of the spirometry indicators. The data obtained are always assessed in a complex manner and changes in a number of parameters indicate the presence of a particular disease, which is additionally confirmed by other instrumental studies.

Contraindications for FVD
It is strictly prohibited to conduct external respiration examination if the following cases are detected:
- children under five years of age;
- patients over 75 years of age;
- there are mental disorders associated with following instructions;
- fever or acute infectious diseases;
- pregnancy;
- high blood pressure;
- epilepsy;
- recent stroke;
- acute stage of myocardial infarction;
- recently undergone operations.
This limitation applies due to the fact that during the study of respiratory function there is an increase in the load on intracranial, intra-abdominal and intrathoracic pressure, as well as tension in the respiratory muscles and osseous-ligamentous apparatus.










