Immunohistochemistry, or immunohistochemical analysis, is a study that uses antibodies to detect certain molecules in tissue samples. This diagnostic method has found wide application in oncology.
A little theory and history. In order to detect and destroy foreign substances, the immune system uses special molecules called antibodies. They differ in specificity: each antibody can bind strictly to a specific antigen.
In 1941, American immunologist Albert Coons first decided to use antibodies in the laboratory to “recognize” bacterial proteins with them. In 1984, Argentine biochemist Cesar Milstein received the Nobel Prize for creating a hybrid of a tumor cell with a lymphocyte that could synthesize monoclonal antibodies. After this, the production of monoclonal antibodies for diagnostic and therapeutic purposes began.
In 1994, S. Taylor used immunohistochemical analysis to test 20,000 tumors and found that the diagnoses were wrong in half the cases. Immunohistochemistry has proven itself to be an effective diagnostic method.
Research method
The exceptional performance of the results obtained using the IMMULITE 2000XPi is ensured by chemiluminescent technology. The emergence of third generation tests is made possible by combining a unique enzyme-enhanced chemiluminescence with exclusive washing technology.

What target molecules are detected during immunohistochemistry?
The number of possible targets is measured in the hundreds. Before the test, the doctor must understand what he is looking for and use the appropriate antibodies. In oncology, the targets are tumor markers - substances that are completely absent in healthy cells or are present in significantly smaller quantities. Here are some examples:
- Estrogen and progesterone receptors help identify hormone-positive breast cancer and determine whether hormonal medications will help a woman.
- Prostate-specific antigen (PSA) is important in the diagnosis of prostate cancer.
- Alpha fetoprotein - present in hepatocellular carcinoma (liver cancer).
- Cytokeratins help in the diagnosis of cancer and some sarcomas (malignant tumors of connective tissue).
- The CD10 enzyme (CALLA) is associated with renal cell carcinoma, lymphoblastic leukemia.

Immunochemical analyzer ACCESS® 2
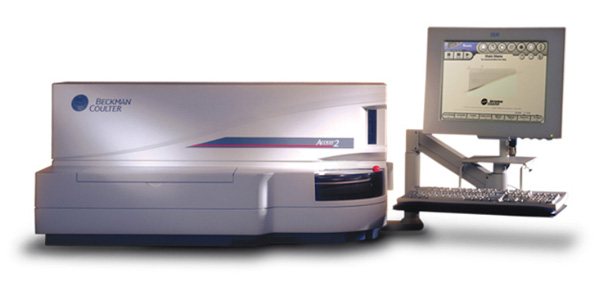
ACCESS® 2 is the first member of the Beckman Coulter family of fully automatic immunochemical analyzers.
The ACCESS® 2 immunochemiluminescence analyzer is developed on the basis of modern enzyme-linked immunosorbent assay (ELISA) technology using paramagnetic microparticles as a solid phase and enzymatically enhanced chemiluminescence as a detection method.
The combination of high performance, a sufficiently large number of reagents on board and the small size of the device best meets the needs of laboratories with a medium and small flow of immunochemical research. Among similar systems for ELISA, Access stands out for its reliability and simple design, ease of use and accuracy of the results obtained.
How it works?
Immunohistochemistry can be direct or indirect. In the first case, one type of antibody is used, which must bind to a specific target molecule. If the target molecule is present in the tissue and a reaction has occurred, the tumor tissue is stained:
- Most often, an enzyme, such as peroxidase, is attached to the antibody. This enzyme catalyzes a chemical reaction that causes the color to change.
- Sometimes fluorescein or rhodamine is added to the antibody, and the staining is detected using fluorescence microscopy.
- Indirect immunohistochemistry is generally used. In this case, two antibodies are used. One combines with the antigen, the second with the resulting antigen-antibody complex. The marker that will cause the color change is coupled to a second antibody.
The indirect method has some advantages:
- It has higher sensitivity because multiple secondary antibodies can bind to one primary antibody (the one that binds to the target protein).
- The study takes little time: it takes approximately 3 hours for the reaction to occur.
- Indirect immunohistochemistry requires a small amount of antibodies. For example, a secondary antibody directed to rabbit immunoglobulins will react to any primary antibody of “rabbit” origin. There is no need to create many different types of secondary antibodies with a staining or fluorescent label.
Brief characteristics of some tumor markers
| Tumor marker | a brief description of | Recommended area of application |
| Beta-2-microglobulin (in urine and serum) | The beta-2-microglobulin protein is identical to the light chain of HLA antigens (free and bound), and is normally detected in biological fluids only in small quantities. | It is recommended to use to confirm the diagnosis and monitor patients with multiple myeloma, non-Hodgkin's lymphoma. The increase in marker concentration depends on the stage of the disease, the degree of malignancy, and the cell type. Monitoring after organ transplantation. |
| Chorionic gonadotronin (hCG) | HCG is normally synthesized in the syncytiotrophoblast of the placenta. | In men and non-pregnant women, an increase in hCG concentration is a reliable sign of malignant growth. The determination of hCG is recommended for diagnosis, monitoring the effectiveness of therapy and early detection of relapses of trophoblastic tumors, chorionic carcinoma of the ovary or placenta, chorionic carcinoma, seminomas. It is most sensitive to carcinoma of the ovary or placenta. |
| Alpha fetoprotein (AFP) | Embryo-specific glycoprotein (up to 4% carbohydrates), similar in amino acid composition to albumin. During pregnancy, it is produced by the cells of the yolk sac, later by the liver of the embryo, as well as by the cells of the fetal gastrointestinal tract. | Recommended for identifying and monitoring the course and effectiveness of therapy for primary hepatocellular carcinoma, germinomas, identifying fetal malformations and monitoring the condition of the fetus during pregnancy. Elevated AFP levels are observed in teratocarcinomas of the yolk sac of the ovary or testes. |
| Carcinoembryonic antigen (CEA) | A glycoprotein with a high carbohydrate content, produced in the tissues of the digestive tract of the embryo and fetus. After the birth of the fetus, its synthesis is suppressed and practically not detected either in the blood or in other biological fluids of an adult healthy person. | An increase in the concentration of CEA is observed in various carcinomas of the digestive tract, as well as in lung, breast, head and neck cancer, and malignant neoplasms of connective tissue origin. With the development of tumors of various localizations, the level of CEA increases and quite accurately reflects the state of the malignant process. |
| CA 125 | A glycoprotein produced by cells of serous malignant ovarian tumors. | A marker for monitoring the course and effectiveness of therapy for various types of ovarian cancer (serous, endometrial, clear cell). The test allows you to detect relapse of the disease 3-4 months before its clinical appearance. |
| CA 15-3 | Mucin-like glycoprotein | Mainly used for monitoring breast cancer (BC). Elevated levels of the marker are observed in approximately 80% of women with metastatic breast cancer, and relapse is accompanied by a significant increase in levels long before clinical manifestations. |
| CA 19-9 | A glycoprotein produced by the epithelium of the fetal gastrointestinal tract, small concentrations are found in the mucous cells of adults, as well as in the pancreas, liver and lungs. | Used for diagnosis and treatment monitoring, as well as early detection of pancreatic, stomach, colon and rectal cancer. |
| CA 242 | The CA 242 epiton is expressed on the same mucin apoprotein as CA 19-9, while in benign tumors the expression of CA 242 is low, and in malignant tumors its expression is much higher. | Today it is one of the main markers used for the diagnosis and monitoring of pancreatic cancer, colon and rectal cancer. The specificity is much higher than that of CA 19-9, allowing diagnosis in the early stages of the disease. According to various data, this test can predict the development of relapses of colorectal cancer within 5-6 months. |
| Prostate specific antigen (PSA) | PSA is a glycoprotein secreted by prostate tubular epithelial cells. | It is the most sensitive and specific marker. Used to diagnose and monitor treatment of prostate cancer. |
| TPA cyk (cytokeratin) | It is a circulating complex of fragments of cytokeratins -8 and -18 that enters the blood during the process of tumor cell necrosis, as well as in the S, G2 and mitotic phases of the normal cell cycle, so its concentration in the serum reflects the rate of cell renewal. | It is used to differentiate stable and progressive stages of the disease, as well as to predict the monitoring of the course of the disease during the treatment of patients with epithelial cell carcinoma. |
| UBC 11 (cytokeratin) | Bladder cancer marker | A sensitive factor indicator of tumor cell proliferation in the bladder, can be used to assess prognosis, monitor and control treatment. |
| TPS | Tissue polypeptide, cytokeratin | TPS levels are determined in patients with epithelial cell carcinomas, such as breast, prostate, ovarian and gastrointestinal carcinoma. Especially in high concentrations it is detected in patients with rapid metastasis. The level before surgery has prognostic significance; a high level after chemotherapy correlates with one-year survival. |
| Tumor M2-PK | Metabolic tumor marker. Most human tumors are characterized by the production of an isomeric form of pyruvate kinase—Tumor M2-PK. Its concentration indicates a switch of cells from a normal type of metabolism to a tumor one; a high correlation is noted with the degree of malignancy (tumor stage). | Marker of the degree of aggressiveness of a malignant tumor. Reveals a specific type of metabolism of tumor cells, regardless of their origin and location. Unlike other tumor markers used in clinical practice, it is not a cumulative marker, but a metabolic marker, and enters the bloodstream early and in sufficient quantities for determination. Determination of TU M2-PL content makes it possible to early diagnose tumors, the occurrence of metastases or tumor relapses (kidney cancer, lung cancer, breast cancer, malignant tumors of the esophagus, stomach, pancreas, colorectal cancer). |
You can contact a specialist at the following email addresses:
What problems in oncology can immunohistochemistry help solve?
Immunohistochemical analysis helps oncologists:
- Classify a malignant tumor as one type or another.
- Find out in which genes of tumor cells mutations have occurred, which proteins contribute to the progression of cancer.
- Identify the primary tumor and its metastases.
- Determine whether malignant cell transformation has occurred.
- Determine the patient's prognosis.
- To figure out whether targeted therapy will help in this case.
- Determine whether tumor cells are sensitive to chemotherapy and radiation therapy.
What is the role of immunohistochemistry in modern oncology?
Immunohistochemical analysis helps study characteristics of a malignant tumor that other diagnostic methods cannot detect. This often plays an important role in clarifying the diagnosis and prescribing the correct treatment. The doctor can determine which combinations of drugs will be most effective for a particular patient, in other words, the principle of personalized treatment is implemented. This often helps improve results and select effective treatment for patients who do not respond to standard therapy.
Book a consultation 24 hours a day
+7+7+78
Immunochemical studies of blood serum
An immunological blood test is a laboratory research method that allows you to assess the state of general immunity, its tension - that is, how much the body’s defense system is involved at the time of analysis, determine the number and function of immune blood cells, and the presence of antibodies in it.
Antibodies are special immunoglobulin proteins (Ig) that are produced by the immune system in response to the entry of any foreign agent into the body to combat it. Antibodies have the ability to form strong complexes with antigens for their subsequent removal from the body.
Antigens include proteins, polysaccharides, nucleic acids, including those contained in the components of various biological structures (cells, tissues, viruses, etc.).
The ability of antigens to cause an immune response is called immunogenicity, and the ability to form complexes with antibodies is called antigenicity.
Immunological analysis can reveal:
- primary and secondary immunodeficiencies
- help in the diagnosis of autoimmune, hematological, infectious and lymphoproliferative diseases
Immunochemical research allows you to determine the level of hormones, antibodies, biologically active molecules, including for the diagnosis and control of anemia, thyroid diseases, and endocrinological disorders.
Immunoglobulins are proteins that have antibody activity (the ability to specifically bind certain antigens).
Unlike most serum proteins, which are produced in the liver, immunoglobulins are produced by plasma cells, descendants of B-lymphocyte precursor stem cells in the bone marrow. Based on structural and functional differences, there are 5 classes of immunoglobulins - IgG, IgA, IgM, IgD, IgE and a number of subclasses. Polyclonal increases in immunoglobulins are a normal response to infections.
When is an immunological blood test prescribed?
Immunological research is carried out:
- in case of recurring infectious diseases
- if the infectious disease is severe and protracted
- if you suspect congenital or acquired immunodeficiency
- if an autoimmune disease is suspected
- for allergic reactions
- before major surgery
- in case the postoperative period proceeds with complications
- in order to monitor the progress of treatment with certain groups of medications (immunosuppressants, immunomodulators, etc.)
Immunological blood test indicators
Immunological analysis includes a set of indicators that reflect the composition and functional activity of the main cells of the immune defense, broken down by cell type and the products of their activity (immunoglobulins). A comprehensive analysis of the immune system is quite complex and time-consuming, so depending on the purpose of the study, the immunological analysis may be limited to indicators representing a specific immune function or affected by a specific pathology.
Most often studied:
- Subpopulations of lymphocytes - white blood cells, various types of which recognize foreign structures (antigens), produce antibodies directed against foreign agents, regulate the intensity of immune processes, recognize and destroy altered body cells (for example, cancer cells). Immunoglobulins are antibodies whose function is to neutralize infectious pathogens and toxins. First of all, immunoglobulins of classes A, M, G are studied
- Immunoglobulins A (IgA) provide local immunity to mucous membranes. Increased levels of IgA are observed in diseases of the skin, digestive and respiratory organs. This is also typical for intoxication, alcoholism, liver and kidney pathologies.
- Immunoglobulins M (IgM) are actively produced during the body’s primary defense reaction, so their increased amounts are observed at the onset of any disease. An increased IgM value is also observed in liver diseases (primarily hepatitis or cirrhosis of the liver)
- Immunoglobulin G (IgG) is the most widespread class of immunoglobulins. They are the main defense produced in response to infection entering the body. Their task is to kill fungi, viruses, pathogenic bacteria, and neutralize toxins produced by the infectious agent. They are responsible for long-term immunity, protecting us from repeated infection.
- Immunoglobulins E (IgE) and D (IgD) are produced mainly in response to a parasitic infection (worm infestation) or in the case of atopic allergies. To determine the body's sensitivity to certain allergens, a special study is carried out - an allergy panel, which identifies specific antibodies to a specific group of allergens (usually immunoglobulins of classes E or G)
Preparing for an immunological blood test
In order for the test results to be accurate, blood should be donated on an empty stomach. It's best to do this in the morning. Optimally, the patient should not eat or drink anything other than water for 12 hours before the test. You should not drink alcohol on the eve of the test. It is advisable not to smoke for an hour before the test.
Immediately before taking the test, it is advisable to sit down and be at rest for 10-15 minutes to eliminate the influence of physical and emotional stress on the research results.
Immunochemical studies of urine proteins
Immunochemical methods for examining urine are used so that the doctor can assess the general condition of the body, as well as identify even the slightest deviations in the tests, which indicates certain diseases in the initial stage. This analysis provides a detailed, accurate picture of the disease and allows the specialist to select the most effective treatment method. The advantages of immunochemical methods of urine testing over other existing standard methods are not only a significantly higher sensitivity in the diagnosis of general proteinuria (the presence of protein in a urine test, which indicates the development of inflammatory processes of various types in the human body), but also the possibility of identifying this biological fluid of individual protein components, determining their special characteristics, so to speak, “proteomics” of urine or selective proteinuria.
Urine must be collected within 24 hours, maintaining the usual drinking regime. The jar of urine should be stored in a cool place. In the morning, at about 6-8 o'clock, empty the bladder (pour out this portion of urine). Then, during the day, collect all the urine in a clean 2-liter container. The last portion is taken exactly at the same time when the collection began the day before (at 6-8 hours). The amount of daily urine should be measured with a measuring cup, poured 10-50 ml into a clean plastic container and delivered to the laboratory of the National Medical Research Center for Hematology. When submitting an analysis to the laboratory, it is necessary to indicate the volume of daily urine.