Hematocrit - what is it, what does it depend on
Hematocrit analysis provides data on the ratio of the volume of red blood cells to the total volume of blood; sometimes this indicator refers to the ratio of the volume of all formed elements to the total volume. There is no particular difference between the interpretations; 99% of the blood cell volume is made up of red cells. More often, hematocrit is recorded as a percentage of the total volume, less often as a ratio of cell volume to total blood volume.
This indicator is determined as part of a general blood test complex. It is classified as secondary and is calculated based on data on the number of red blood cells. Occasionally, direct measurement of hematocrit is performed by centrifuging the sample. This procedure allows you to separate plasma from formed elements and directly measure this indicator.
Indications and preparation for analysis
Indications for hematocrit analysis are symptoms indicating the development of anemia or other diseases of the blood or hematopoietic system. These include:
- Pale or jaundiced skin
- Enlarged spleen, liver
- Changes in the size of lymph nodes
- Digestive disorders
- Skin and hair problems (rashes, ulcers on mucous membranes, hair loss or brittleness)
In addition to identifying anemia, the analysis allows us to identify other diseases, for example, polycythemia (a chronic disease in which the bone marrow produces an excess amount of red blood cells) of various origins. This study is also used when it is necessary to assess the need for blood transfusion and calculate the required volume of transfusion.
No special preparation is required for the hematocrit test. It is necessary to follow the standard rules for conducting a general blood test:
- Blood is drawn early in the morning.
- You should not eat food 6-10 hours before the test.
- Avoid alcohol 2-3 days before the procedure.
Patients who smoke are advised to abstain from smoking for at least 2-3 hours before blood collection. If these recommendations are not followed, the analysis may give unreliable results. This is due to the fact that the composition of the blood is subject to strong fluctuations depending on the action of various environmental factors.
Anemia
Iron deficiency
Gastritis
Jaundice
27263 06 November
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Anemia: causes, symptoms, diagnosis and treatment methods.
Definition
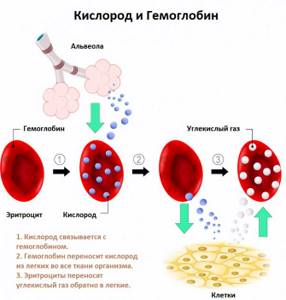
Anemia is a decrease in hemoglobin content and/or a decrease in the number of red blood cells per unit volume of blood, leading to a decrease in the supply of oxygen to tissues.
The diagnosis of anemia is made when hemoglobin decreases below 130 g/l in men and below 115 g/l in women. In children, the age of the child is taken into account when diagnosing anemia.
Anemia occurs in a number of diseases (ulcers and polyps of the gastrointestinal tract, chronic kidney disease, cancer, infectious diseases, helminthic infestations, etc.). The lower the hemoglobin level, the more severe the anemia.
Causes of anemia
Anemia can occur as a result of impaired red blood cell production, increased destruction of red blood cells, or loss of red blood cells in the blood.
Statistics say that the most common is anemia that occurs after
blood loss
(acute or chronic). Acute is considered blood loss with a blood volume of more than 500-700 ml (in adults), which occurs over a short period of time. Blood loss can be visible (bleeding from wounds, hematemesis, uterine, nasal bleeding) and initially hidden (bleeding into the intestines, into the abdominal cavity and/or pleura, large hematomas).
Chronic blood loss develops as a result of minor but prolonged blood loss (heavy and prolonged menstruation, stomach ulcers, cancer, hemorrhoids, hemodialysis procedures, etc.). Over time, minor blood loss leads to depletion of iron stores in the body, when the amount of iron lost by the body exceeds its intake from food. As a result of iron deficiency, hemoglobin synthesis is disrupted.

Each mature red blood cell leaves the bone marrow with a “set” of 250-500 million hemoglobin molecules. The hemoglobin molecule consists of a protein part (four globin subunits) and a non-protein iron-containing group (heme). The main biological function of hemoglobin is the transport of oxygen from the lungs to the tissues and the transport of carbon dioxide from the tissues to the lungs. The lifespan of red blood cells is about 120 days.
Iron deficiency can occur due to decreased iron absorption as a result of various diseases of the duodenum and initial parts of the small intestine (enteritis, tumors, conditions after surgical interventions in this area of the intestine). Conditions leading to a decrease in the level of blood proteins that transport iron (nephrotic syndrome, impaired protein-synthetic function of the liver, malabsorption syndrome, nutritional deficiency) can also lead to its decrease and, as a result, to anemia.
Iron deficiency anemia associated with initially insufficient iron levels (lack of iron in the mother during pregnancy) is observed in newborns and young children.
Anemia due to impaired hematopoiesis occurs:
- in case of insufficient intake into the body or impaired absorption in the gastrointestinal tract of the components necessary for the formation of red blood cells (vitamin B6, vitamin B12, folic acid, etc.);
- damage to bone marrow cells—precursors of red blood cells—by toxic substances and ionizing radiation;
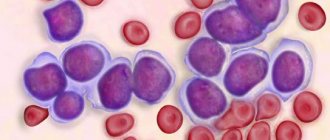
- formation of secondary foci of tumor cells in the bone marrow (metastasis);
- disruption of the synthesis of the non-protein part of hemoglobin (heme) and the accumulation of its toxic products;
- dysregulation of red blood cell formation (decreased production of a hormone that stimulates the growth and reproduction of red blood cells (erythropoietin) or exposure to inhibitors).
Other anemias - hemolytic - develop as a result of increased destruction of red blood cells under the influence of both hereditary and acquired factors.
The development of hereditary hemolytic anemia is associated with genetic defects (impaired activity of erythrocyte enzymes, impaired structure or synthesis of hemoglobin, defects in erythrocyte membranes).
Acquired hemolytic anemia can be caused by the destruction of red blood cells as a result of exposure to antibodies, mechanical damage to the membrane of red blood cells, chemical damage to red blood cells, lack of vitamins, and destruction of red blood cells by parasites.
Classification of anemia
1. Anemia associated with blood loss:
- spicy,
- chronic.
2. Anemia resulting from hematopoietic disorders:
- anemia associated with impaired hemoglobin formation;
- anemia associated with impaired DNA and RNA synthesis;
- anemia associated with disruption of red blood cell division processes;
- anemia associated with inhibition of proliferation (reproduction) of bone marrow cells.
3. Anemia associated with increased blood destruction (hemolytic anemia):
- hereditary hemolytic anemia;
- acquired hemolytic anemia.
Symptoms of anemia
The severity of anemia depends on the severity of the disease and the speed of its development. The lower the hemoglobin and the faster the anemia develops, the more pronounced the clinical picture.
There are general (nonspecific) manifestations of anemia and signs that are specific to a certain type of anemia.
To nonspecific signs
Anemia includes pallor of the skin, weakness, increased fatigue, drowsiness, dizziness, fainting, tinnitus, flashing “spots” before the eyes, shortness of breath, palpitations, rapid pulse, etc.
The absence of these signs does not exclude the presence of anemia, since with mild and moderate forms of the disease, as well as its slow development, the clinical picture may be blurry.
Clinical manifestations of iron deficiency
in the body: dry skin, violation of the integrity of the epidermis, brittle nails, hair, ulcerations and cracks in the corners of the mouth, muscle weakness. There may be a burning sensation of the tongue, a perversion of taste in the form of an indomitable desire to eat chalk, toothpaste, soil, raw cereals, raw meat, as well as an addiction to certain odors (acetone, gasoline).
Iron deficiency is characterized by damage to the gastrointestinal tract (gastritis).
Vitamin B12 deficiency
can also manifest itself as damage to the gastrointestinal tract (atrophic gastritis) and neurological symptoms (paresthesia, sensory disturbances, numbness of the extremities). In extremely severe cases of the disease, mental disorders, delusions, hallucinations, acquired dementia, etc. are observed.
Clinical picture of folic acid deficiency
very similar to vitamin B12 deficiency, but in folate deficiency conditions there are no neurological symptoms and inflammation of the tongue rarely occurs. Folic acid deficiency leads to exacerbation of schizophrenia, increased frequency and severity of epilepsy attacks.
For hemolytic anemias
Characterized by yellowness of the skin and mucous membranes, an increase in the size of the spleen, and a tendency to form stones in the bile ducts.
With massive hemolysis of erythrocytes (hemolytic crisis), in addition to anemia, jaundice and deterioration of the general condition, nausea, vomiting, confusion, convulsions, and the development of acute renal and/or cardiovascular failure may be observed.
With aplastic anemia, which occurs against the background of suppressed proliferation of bone marrow cells, hemorrhages occur (mainly in the thighs, legs, abdomen, hematomas are formed at injection sites). Bronchitis and pneumonia are often diagnosed.
Diagnosis of anemia
Anemia can occur under the influence of a wide variety of factors. The most common are deficiency anemias (iron deficiency, B12 deficiency, folate deficiency, etc.).
An important role in identifying the cause of anemia is played by information obtained from interviewing the patient: age, the presence of occupational hazards, the nature of the diet, the presence of concomitant diseases, taking medications, information about heredity, etc. Examination data are no less important: changes in the color and condition of the skin; enlarged lymph nodes, liver, spleen; presence of damage to the nervous system.
The first stage of diagnosing anemia usually includes the following studies:
- clinical blood test: determination of hemoglobin concentration, number of erythrocytes, leukocytes, hematocrit and erythrocyte indices (MCV, RDW, MCH, MCHC), leukocyte formula and ESR (with microscopy of a blood smear in the presence of pathological changes);
Blood test for hematocrit

The manipulation is performed in the morning, blood is taken from a vein or from a finger. At the Medart clinic, the most modern equipment is used for analysis, so the sampling is most often done from a vein.
To obtain the material, special vacuum containers (vacutainers) are used. This is a modern syringe replacement that provides a number of benefits for the patient:
- Virtually painless procedure.
- Minimum time to obtain the required amount of blood.
- Accurate calculation of the amount of reagent and blood.
- Minimum time for conducting the study and issuing results to the patient.
Modern technologies allow the procedure to be carried out as quickly as possible, without consequences for health.
Norms
The normal hematocrit level depends on the age and gender of the person. For a mature woman it is 37-50%, for a man 34-45%. For newborns, this figure may be higher and ranges from 35 to 65%. As people grow older, the hematocrit decreases, reaching minimal levels in the elderly. This is the result of decreased bone marrow activity and decreased production of blood cellular elements.
A decrease in normal hematocrit in women is associated with regular blood loss during menstruation. High values in children are a manifestation of active processes in the development of red bone marrow and other hematopoietic organs.
It is important to consider that after massive blood losses and blood transfusions, determining the hematocrit level will give results with a large error. To reliably assess this indicator in such cases, it is necessary to wait a certain time.
It may take up to 3 months for complete physiological restoration of red blood cell levels to normal levels. This period is the life cycle of red blood cells, during which the cellular composition of the blood is renewed.
Hematocrit: normal indicators
Each person has about 4.5-5 liters of blood in his body. It consists of heavy red blood cells and light, light-colored plasma. When settling, the red blood cells sink down and the plasma rises to the top if the blood was collected using an anticoagulant.
If the test is taken in a dry tube, the blood coagulates, forming a fibrin clot. It will contain red blood cells and serum. It differs from plasma in a lighter color, since it does not contain fibrinogen (a protein component). In the human body, blood is represented by plasma with platelets, erythrocytes and leukocytes dissolved in it, as well as other proteins. Most of the components are absent in the blood serum.
Normal hematocrit readings for different categories of patients:
- Men: 0.44-0.48, and sometimes up to 0.52. Such high values are indicators of the norm, since male blood is renewed less frequently than female blood.
- Women: 0.36-0.43. During pregnancy, starting from the 20th week of pregnancy, the hematocrit level begins to decrease.
- Children: 0.44-0.62 - for newborns, 0.32-0.44 - for infants up to 3 months, 0.36-0.44 - for children up to one year, 0.37-0.44 - for children up to 10 years. In the future, normal indicators are determined by a person’s gender and state of health.
A decrease or increase in blood hematocrit indicates the degree of concentration of red blood cells in it.
Hematocrit increased
An increase in the level of red blood cells detected in a hematocrit analysis may indicate various pathological conditions. The most common:
- Primary erythrocytosis. It occurs as a result of overactive production of red blood cells, including immature forms. May indicate the development of tumors in the bone marrow.
- Secondary erythrocytosis. Develops as a consequence of pathologies of the respiratory and cardiovascular systems (heart defects, respiratory failure).
- Reduced plasma volume. May indicate the development of peritonitis, leukemia, kidney disease. Often occurs with extensive burns, when blood plasma sweats through the damaged dermis.
- Dehydration. Observed in uncompensated diabetes mellitus, it can result from diarrhea, vomiting, excessive sweating and lack of fluid in the diet.
Erythrocytosis can develop in heavy smokers, especially if smoking has led to secondary damage to the respiratory system and heart. In this case, the body turns on mechanisms to compensate for insufficient oxygenation due to a significant increase in the number of red cells.
An increase in hematocrit is not always a consequence of disease. An increase in the number of red blood cells is considered normal for residents of mountainous areas and professional climbers. When exposed to high altitude conditions for a sufficiently long time, the body compensates for the lack of oxygen and atmospheric pressure by increasing the production of red blood cells.
Erythrocytosis is often asymptomatic and is discovered by chance during a blood test for other reasons. Only with a significant increase in hematocrit are the following observed:
- Pain in joints, muscles.
- Dyspnea.
- High blood pressure.
- Ringing in the ears and dizziness.
- Increased sweating, sleep disturbances.
These symptoms are not specific, so if such ailments occur, you should consult a doctor for further diagnosis.
To restore the physiological level of hematocrit, it is necessary to find out the reason that led to an increase in the amount of blood cells and eliminate it. For example, if erythrocytosis was caused by dehydration (lack of water in the body - dehydration), it is enough to restore the normal amount of fluid to normalize this indicator.
There is no need to self-medicate; only a specialist can accurately determine the cause of the increase in hematocrit and prescribe the correct diagnosis and treatment. Therefore, if there are any changes in the blood test, you should consult a specialist and strictly follow the recommendations received.
Low hematocrit
The fewer red blood cells in the blood and the smaller their size, the lower the hematocrit level. If the hematocrit value drops to 20-25%, then the person is diagnosed with anemia. This condition may be caused by a decrease in the level of red blood cells in the blood. This condition is called erythrocytopenia. Low hematocrit is also observed when water accumulates in the body - this condition is called overhydration. The hematocrit will decrease as the level of proteins in the body increases, which contribute to fluid retention. This condition is called hyperproteinemia.
Causes of low hematocrit:
- Bleeding. Circulating blood volumes are replenished quickly due to the administration of infusion solutions, but it will take some time for red blood cell counts to return to normal.
- Anemia and leukemia, taking cytostatics and antitumor drugs, kidney paresis, which are accompanied by insufficient production of red blood cells in the bone marrow.
- The death of red blood cells is caused by hemolytic anemia, which develops during a person’s life or is inherited from blood relatives, intoxication of the body with hemolytic toxins, for example, salts of heavy metals, as well as diseases such as malaria and typhoid fever.
- Administration of significant volumes of fluids through a vein to patients with impaired renal function. This entails an increase in the total volume of blood, but the number of red blood cells in it will remain the same.
- Second half of pregnancy. At the same time, the plasma level increases, and the erythrocyte level remains at the same levels.
- Anemia, regardless of its nature.
- Overhydration of the body due to water intoxication, circulatory failure, disorders of the kidneys and other excretory systems.
- An increase in protein levels in the blood due to vomiting, diarrhea, myeloma, Hodgkin lymphoma and other pathological conditions. The level of the liquid component of the blood increases, but the level of red blood cells remains at the same level.
In children, the hematocrit level will decrease for the same reasons as in adult patients. However, pathologies in a child often have a much more pronounced clinical picture and are more severe.