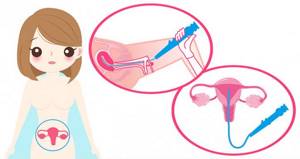
Hysteroscopy of the uterus is both a diagnostic and therapeutic procedure that allows you to examine the uterine cavity from the inside and, if necessary, perform various medical procedures, for example, remove foreign bodies, polyps, etc. Hysteroscopy is performed using special instruments that are inserted through the vagina.
- Types of hysteroscopy of the uterus
- Indications for performing hysteroscopy of the uterus
- How to prepare for hysteroscopy of the uterus
- How is hysteroscopy performed?
- Contraindications
- Recovery after hysteroscopy of the uterus
- What complications can hysteroscopy cause?
- What procedures can a gynecologist perform during hysteroscopy?
- When can hysteroscopy be performed?
- Risks of hysteroscopy
- What alternatives are there to hysteroscopy?
Types of hysteroscopy of the uterus
- Diagnostic hysteroscopy. As the name implies, this procedure does not involve therapeutic interventions. During diagnostic hysteroscopy, only a visual examination of the internal cavity of the uterus and cervical canal is performed using a special optical system. Since no surgery is performed, significant anesthesia is not required. In most cases, local anesthesia and sedation are sufficient. The recovery period after the procedure is short. No hospitalization required.
- Surgical hysteroscopy is already a therapeutic and diagnostic intervention. It allows you to detect the problem and immediately treat it. This procedure is prescribed when the diagnosis has already been established, or in cases where its probability is maximum. This is already a full-fledged operation, albeit a low-traumatic one. It requires anesthesia and is therefore performed in a hospital setting.
- Control hysteroscopy. It is carried out to monitor the condition of the uterus after surgical treatment.
Minilaparoscopy, hysteroscopy, endometrial aspiration with histological examination are an alternative method for diagnosing and treating female factor infertility in the Department of Reproductive Health of the Regional Perinatal Center of the city of Yaroslavl.
Endoscopy occupies a special place in the diagnosis and surgical treatment of female infertility: it provides a quick and extremely accurate diagnosis of the state of the woman’s reproductive system, and is a minimally invasive and minimally traumatic method of surgical treatment. Allows, for example, to preserve the fallopian tubes and ovaries during purulent salpingitis and tubo-ovarian formations, to preserve the uterus during conservative myomectomy, to restore the normal anatomy of the pelvic organs and uterine cavity, etc.
In a female infertility clinic, endoscopy makes it possible to identify and treat preclinical forms of diseases, such as the initial stages of endometriosis, tumors of the uterus and ovaries.
Minilaparoscopy is a new direction in reproductive surgery!
Unlike conventional (standard laparoscopy), this method has a number of advantages and is distinguished by the use of ultra-thin microlaparoscopic instruments (2-3 mm). Using these instruments and equipment, almost all types of surgical interventions are performed: diagnostic laparoscopy, checking the patency of the fallopian tubes - chromosalpingoscopy, resection and coagulation of foci of endometriosis, myomectomy of small nodes, removal of ovarian cysts, reconstructive plastic surgery on the fallopian tubes for infertility, with restoration their patency, operations for endocrine infertility (PCOS), organ-preserving operations for ectopic pregnancy or removal of fallopian tubes before IVF, etc. Microlaparoscopy helps relieve patients from lengthy examination and treatment for infertility, which is often harmful to their health. This does not require lengthy preoperative preparation or long hospitalization after surgery, and the rehabilitation time in the postoperative period is significantly reduced.
History of the method.
The first publications on the use of microlaparoscopy date back to the 1990s, when Dorsey & Tabb 1990 (1) and Risquez et all (2) 1991 first used this method. Surgeons obtained good results and developed new indications for the use of this method, but the only obstacle was poor video images. With the development of new technologies for the production of optics and instruments, science has made great progress: the diameter of laparoscopes and working instruments began to decrease, and visualization has significantly improved. New opportunities have opened up for the use of microlaparoscopy in the treatment of female infertility (adhesiolysis, resection and coagulation of endometriosis foci, stomatoplasty, sterilization or inactivation of the fallopian tubes, myomectomy, operations for ectopic pregnancy, cystectomy and ovarian drilling. Later, Wattiez A and all (3) in 1999 for the first time performed microlaparoscopic hysterectomy (removal of the uterus), thereby demonstrating the great potential of operative microlaparoscopy. Many surgeons demonstrate that microlaparoscopy is a highly effective method, not inferior to conventional laparoscopy and is a less invasive method that can be used in an outpatient setting using local anesthesia. (Bauer at all, 1995, Downing and Wood, 1995, Fuller, 1996, Kovacs at all 1998), therefore minimizing surgical exposure is one of the main tasks of gynecological reproductive surgeons.
Many studies show that reducing the caliber of instruments and the use of low-traumatic surgical energies and instruments, including thermocoagulation, weak laser energies, can reduce surgical trauma and, as a result, have a minimal negative impact on a woman’s reproductive health. Microlaparoscopy has great potential for diagnosing the causes of infertility, their surgical correction and the possibility of performing surgery on an outpatient basis.
The Department of Reproductive Health of the Regional Perinatal Center has the opportunity to perform these unique types of operations on the basis of a one-day hospital, equipped with high-tech medical equipment of the new generation and staffed with specially trained specialists in the field of reproductive surgery and laparoscopy.
FAST TRACK SURGERY – THE NEWEST MULTIMODAL STRATEGY FOR ACTIVE SURGICAL TREATMENT OF PATIENTS WITH GYNECOLOGICAL DISEASES
The active introduction of endoscopic treatment methods has led to a reduction in hospitalization periods, a speedy recovery and restoration of the working capacity of operated patients.
Since most approaches to surgery (surgery schemes, surgical techniques, pain management methods, principles of preoperative preparation, principles of patient care) were formed in the pre-antibiotic era, the introduction of laparoscopic surgery methods required a revision of existing ideas by the end of the 1980s. This phase transition coincided with the widespread introduction of the principles of evidence-based medicine and the revision of most established ideas, first within the framework of the Cochrane Collaboration (Cochrane Collaboration, 1988 - 2013, Great Britain), and then in the format of large-scale studies initiated by the national surgical and gynecological associations of the USA, Great Britain, France and Germany to test the entire amount of knowledge about surgery.
Conducted for 1990-2010. Multicenter, worldwide, double-blind studies testing methods of preparing patients for operations that have become unshakable stereotypes have revealed their ineffectiveness: for example, long-term preoperative bowel preparation, mandatory use of a nasogastric tube, postoperative drainages located in cavities, mandatory long-term bed rest, staged diets have proven to be the case in many surgical interventions are not only useless, but in some cases harmful.
As a result of the search for effective methods of treating surgical patients with minimal risk, a new concept arose - fast track surgery (“fast track in surgery”, “fast track surgery”, acceleration of various stages of the treatment process), or ERAS (early rehabilitation after surgery - early rehabilitation after operations). The selection of anesthesia techniques, minimally invasive surgical techniques, optimal pain control and active postoperative recovery (including early oral nutrition and mobilization) in fast track surgery reduces stress reactions and organ dysfunction, significantly reducing the time required for full recovery. The use of laparoscopic technologies corresponds to the principles of fast track surgery as much as possible. Growing interest in this program is reflected in abdominal surgery, oncology, gynecology, urology and other surgical disciplines.
>The pioneer of the multimodal fast track program in Europe, covering all phases of perioperative therapy, is Professor H. Rehlet. J. Wind (2006) summarized and identified the factors included in a multimodal fast track program in randomized trials and meta-analyses, the main ones of which are listed below.
Fast-track surgery is a system of in-depth preparation of the patient in the preoperative period in combination with a system of active postoperative rehabilitation (Prof. K.V. Puchkov, 2010-2013)
A modern computerized operating room for minimally invasive laparoscopic surgery using the example of an operating room manufactured by Karl Storz.
The evolution of surgical instruments for minimally invasive surgery.
Replacing a hand seam with a hardware seam.
Preoperative patient information
Avoiding bowel preparation before surgery
Refusal of premedication in combination with a change in the intraoperative anesthesia regimen
Using probiotics before surgery
Avoiding complete fasting before surgery
Use of dextrose (glucose) solution 2 hours before surgery in combination with adequate water and electrolyte load
Regional anesthesia or short-acting anesthetics
Adequate volume of infusion in the perioperative period
Short incisions (laparoscopy, minimally invasive approach, transverse incisions)
Prevention of preoperative hypothermia
Use of high concentrations of O2 perioperatively
Non-opioid analgesia
Avoiding routine use of drains and nasogastric tubes
span>Prokinetics
Early initiation of postoperative oral nutrition
Early mobilization
Current prospects for minimally invasive surgery are robotic surgery, “surgery of natural orifices”, “surgery of 1 window (port)”.
— WHAT IS BEHIND THIS NEW SURGICAL CONCEPT?
Until now, pelvic surgery was considered an intermediate-level surgical intervention, after which patients had to spend at least 10-15 days in the clinic. The Fast Track method has thrown away many of the rules and dogmas of surgery that have been in effect until now: patients can leave the clinic after such an operation in the coming days, again feeling cheerful and productive. “Reducing the body's stress levels leads to faster recovery” is the exact explanation of the Fast Track concept. As many years of experience have shown, operations cause stress reactions in the body, which naturally complicate its recovery. The Fast Track concept is precisely aimed at restoring normal self-regulation of the body as quickly as possible.
The concept of “fast track” covers all phases of perioperative therapy: preoperative, intraoperative and postoperative.
PREOPERATIVE STRATEGY
Patient education - explanation and real information about upcoming medical procedures, surgery, post-operative period, benefits of the fast track program. Standardization of most stages of operations and examination methods has made minimally invasive surgery a highly predictable technological medical discipline, which makes it possible, with a high probability, in contrast to traditional surgery, to inform the patient in advance about the results of the operation and the postoperative period.
No dietary restrictions before surgery. Considering that prolonging the fasting period with a decrease in the pH of gastric contents increases the risk of aspiration, the patient is allowed to drink up to 400 ml of clear liquid during the night, since this volume does not increase the risk of aspiration complications during intubation. Using the principles of evidence-based medicine, it has been demonstrated that preoperative fasting significantly reduces liver glycogen reserves and causes postoperative insulin resistance. The result of this is a decrease in the body's regenerative resources. As a result, it is justified to use 150 ml of dextrose (glucose) 2 hours before surgery, which also helps reduce feelings of hunger, thirst, discomfort, fatigue, and, consequently, the stress response. The reduction in the severity of fear as a result of the release of endogenous opioids in turn leads to a decrease in the intraoperative need for anesthetics.
According to the results of randomized studies, the need for mechanical bowel preparation for surgery is not considered justified.
INTRAOPERATIVE STRATEGY
Anesthesia that minimizes surgical stress meets the goals of fast-track surgery. The introduction into clinical practice of short-acting intravenous anesthetics (propofol), synthetic opioids (fentanyl) and muscle relaxants has made it possible to expand the indications for operations in which patients are in the clinic for no more than 24 hours, to shorten the duration of the recovery period, and to reduce the need for long-term monitoring.
The use of minimally invasive surgical techniques reduces the inflammatory component of the stress response without significantly affecting the neuroendocrine and metabolic response. Minimally invasive surgery involves reduced pain and shorter hospital stays compared to open techniques. Pain and pulmonary dysfunction are less common during laparoscopic operations; at the same time, the use of laparoscopic access, despite minimal trauma to the anterior abdominal wall, does not relieve patients from postoperative pain (as a result of irritation of the peritoneum with carbonic acid), therefore diaphragm anesthesia is relevant and sufficient during minimally invasive operations.
Directed goal therapy during surgery involves preventing intraoperative hypovolemia and excessive crystalloid infusion, which can lead to edema, poor tissue oxygenation, and delayed healing. The possibility of drinking liquid at night and refusing to prepare the bowel leads to the absence of hypovolemia at the beginning of the operation and a decrease in intraoperative infusion.
Ensuring intraoperative normothermia. The development of intraoperative hypothermia entails deterioration of hemostasis with an increase in intra- and postoperative blood loss, increased postoperative tremors with increased oxygen consumption and an increased risk of myocardial ischemia. Actively warming the patient, covering non-operative parts of the body, and administering warm infusion media help maintain normothermia.
The development of Fast Track surgery would not have been possible without advances in medical equipment, including the creation of computerized operating rooms.
POSTOPERATIVE STRATEGY
Effective pain relief. Postoperative pain is the most important factor influencing the length of a patient's postoperative hospital stay. Postoperative analgesia requires a multimodal approach with the integrated use of regional analgesia, neuronal blocks, a combination of acetaminophen and non-steroidal anti-inflammatory drugs, which reduces the use of opioids and, as a result, reduces their side effects.
Early oral hydration. Drink more than 300 ml of fluid on the day of surgery and stop the intravenous infusion on day 1.
Early restoration of enteral nutrition (6 hours after surgery) is necessary for the success of the fast track surgery program after both minor and major surgeries.
Accelerated mobilization is the early ability to ambulate for at least 6 hours out of bed during the 1st day after surgery. Bed rest worsens muscle loss and weakness, impairs pulmonary function, predisposes to venous stasis and thromboembolism, and promotes postoperative adhesions. Every effort should be made to achieve postoperative activation, which is possible with adequate analgesia.
— WHAT DOES FAST TRACK SURGERY MEAN FOR A PATIENT?
Firstly, a guarantee of faster recovery after such an operation. When using old methods of surgery, the body naturally became unbalanced due to prolonged lying down and delayed nutrition and required much more time to fully recover.
With the Fast Track method, the intestine is prepared for surgery using much more gentle methods. Lavage (cleansing enema), which until now was required according to regulations before each abdominal operation, is completely abolished within the framework of this concept. A high cleansing enema is not only unpleasant for the patient, but can also cause a shift in the composition of electrolytes (potassium, sodium, calcium, chloride) in the body, which adversely affects subsequent recovery, and is also one of the factors affecting cardiac activity and the functioning of the body’s coagulation system patient, which is one of the causes of acute intraoperative complications and complications of the early postoperative period.
In addition, previously, patients were not allowed to eat or drink the evening before surgery. As a result, patients during and after surgery had to receive more fluid infusions than required for normal organ function. According to the new technique, patients can and should drink clear liquids at least 4-6 hours before surgery.
Another dogma of traditional colon surgery was that the colon should rest after surgery, so patients could not eat regular food until a maximum of five days after surgery. Now, within a few hours after surgery, patients receive some liquid and light food. The new approach is based on the results of modern research that have shown that the intestine, thanks to the autonomic nervous system, functions around the clock, in almost any state of the body, therefore, when the main substrate of its work disappears from the intestine, it does not “rest”, but is “paralyzed”; A “paralyzed” intestine that does not perform its function “rests” worse, and thus has a bad effect on the recovery of the body as a whole.
Already six hours after the operation, patients are mobilized. Then the next day work begins on a targeted intensive recovery program.
— FAST TRACK SURGERY AND MINIMALLY INVASIVE SURGERY.
In our clinic we combine Fast Track surgery with minimally invasive laparoscopic and hysteroscopic surgery.
— MORE WORK FOR THE BENEFITS OF THE PATIENT
Directly for the operating doctor, surgery “through the keyhole” means additional labor costs. The operation requires more time. In addition, such operations require the doctor to have more experience. The technical equipment required for this is more expensive to purchase and more expensive to operate. However, we strive to use the Fast Track technique in combination with laparoscopy because... We expect maximum benefit from this for patients.
— IS THIS OPERATION METHOD SUITABLE FOR EVERY PATIENT?
For the success of the Fast Track concept, it is important that patients are well prepared for it and actively contribute to their own recovery process. Of course, each patient independently decides which concept to prefer.
We offer you medical services::
Minilaparohysteroscopic operation (diagnostic) with highly comfortable mechanical ventilation, biopsy of material - 40,000.00
Minilaparohysteroscopic surgery (therapeutic) with highly comfortable mechanical ventilation,
hospitalization, biopsy of material - 60,000.00
Indications for performing hysteroscopy of the uterus
- Infertility of unknown etiology.
- Habitual miscarriage.
- Polyps of the uterus and cervical canal.
- Foreign bodies in the uterine cavity, for example, intrauterine contraceptives.
- Pathology of the endometrium - hyperplasia, synechiae.
- Suspicion of uterine malformations.
- Metrorrhagia is non-cyclic uterine bleeding.
- Bleeding after menopause.
Currently, there is a trend away from carrying out invasive techniques purely for the purpose of examination, since this is one way or another associated with certain risks, and the necessary information can often be obtained using safer methods. The same applies to diagnostic hysteroscopy. The procedure is prescribed only if it is impossible to establish a diagnosis using other non-invasive methods.
Book a consultation 24 hours a day
+7+7+78
How to prepare for hysteroscopy of the uterus
Hysteroscopy of the uterus is an invasive procedure that carries certain risks. To minimize them, it is necessary to undergo examination and, if indicated, treatment. As part of the examination, the following tests are prescribed:
- General and biochemical analysis of blood and urine.
- Smear for flora and oncocytology (if not performed within the last year).
- Test for STIs.
- Coagulogram.
- Determination of blood group and Rh factor.
- ECG.
- Determination of markers of infectious diseases: HIV, parenteral hepatitis, syphilis.
If inflammatory gynecological processes are detected, sanitation is carried out.
Hysteroscopy is planned in accordance with the menstrual cycle. It is recommended to perform the procedure in the first days after the end of menstruation, since during this period there is no growth of the endometrium and it is easier to detect its pathology. However, if there are absolute medical indications, the procedure can be performed on any day of the cycle. Immediately before hysteroscopy, you must adhere to the following rules:
- Avoid vaginal sex 1-2 days before the scheduled procedure.
- The last meal should be at least 6 hours before the start of the intervention. This condition is necessary for safe anesthesia. Anesthesia can lead to muscle relaxation and the flow of gastric contents into the airways. This is fraught with the development of asphyxia or aspiration pneumonia, which is difficult to treat.
- You will need to shower on the day of surgery.
- Before the operating room, you must empty your bladder and remove jewelry, dentures, and contact lenses.
Infertility
Is laparoscopy and hysteroscopy performed for infertility? Is there a chance to restore reproductive function using these techniques? The causes of infertility can be very diverse. For example, adhesions in the tubes prevent sperm from moving into the ovaries. With the help of hysteroscopy, adhesions can be removed, which will clear the way for sperm.
Hysteroscopy allows you to establish an accurate diagnosis, on the basis of which the gynecologist prescribes a course of therapeutic manipulations corresponding to the clinical picture. Hysteroscopy also helps to get rid of many pathologies that impede successful fertilization:
- ovarian cysts;
- adhesive obstruction;
- tumors, cysts, polyps;
- endometriosis.
Conception after laparoscopy
Patients are interested in the question of the timing of possible pregnancy after surgical procedures. The chance of getting pregnant depends on the individual characteristics of the patient’s body, the severity of the existing pathology and the complexity of the surgery performed. Age, existing chronic inflammatory processes of the reproductive organs and complications after surgery also contribute.
Premature pregnancy after laparoscopy always ends with undesirable consequences. The time of conception must be agreed upon with the local gynecologist.
When is it advisable to plan a pregnancy? For the body to fully recover after surgical procedures, three months or six months must pass. After a thorough examination of the patient, the gynecologist makes a conclusion about the possibility/impossibility of conceiving a child. Ovarian cyst surgery delays the time of planned fertilization by six months instead of three months.
Removal of polycystic ovary syndrome does not require a long recovery period, so after 28-30 days you can think about conceiving a child. Restoring women's health after an ectopic pregnancy requires a long period of rehabilitation - at least six months. Doctors are cautious about planning conception after an ectopic pregnancy and recommend giving the body rest for about a year.
How is childbirth after laparoscopy? This operation does not leave any scars on the body of the uterus, so the woman can give birth naturally. If doctors deem it necessary, the patient will undergo a caesarean section. One should not think that weak labor is caused by a previous operation before the birth - it depends on the characteristics of the female body.
Pregnancy after hysteroscopy
Hysteroscopy is divided into two types - diagnostic and surgical. After diagnostic procedures there are no obstacles to conception. Surgical procedures establish their own rules: the body needs a recovery period. Rehabilitation depends entirely on the severity of the pathological process and the surgery performed.
As a rule, six months is enough for the body to recover after the intervention. After surgery, intrauterine infection may develop, so premature pregnancy may result in miscarriage or premature birth.
A sluggish infectious process in the uterus can also provoke fetal hypoxia, polyhydramnios, abnormal fetal position and fetoplacental insufficiency. Therefore, it is not recommended to rush with fertilization. Before conception, the gynecologist will conduct a thorough examination using instrumental and laboratory diagnostics - ultrasound, culture of vaginal flora, blood and urine tests.
To maintain the pregnancy, synthetic hormonal drugs are used (for example, Duphaston), which promote reliable fixation of the embryo to the wall of the uterus. This drug also stimulates the endometrium, prepares the uterine cavity for gestation and eliminates contraction of muscle fibers. Duphaston is prescribed in the first trimester of pregnancy.

How is hysteroscopy performed?
An hour before the patient is admitted to the operating room, premedication is administered, the purpose of which is to reduce anxiety, increase tolerance to anesthesia and reduce the secretory activity of the glands. For this purpose, a combination of drugs is prescribed, containing narcotic analgesics, antihistamines, anticholinergics and sedatives.
In the operating room, the patient is placed in a gynecological chair and anesthesia is administered. The type of anesthesia is discussed in advance, taking into account contraindications, recommendations of the anesthesiologist and the wishes of the patient.
Next, proceed directly to hysteroscopy:
- The cervical canal is expanded using special instruments.
- A sterile liquid or gas is injected into the uterus through an enlarged canal. This is necessary to expand its cavity and make it accessible for inspection and manipulation.
- Next, a hysteroscope is inserted through the cervix - a thin tube with a diameter of about 5 mm with an optical system that transmits an enlarged image to the monitor. As it is introduced, the cervical canal, intrauterine cavity and its angles are examined.
- After the diagnosis has been established, treatment is carried out using the same hysteroscope, which has a special channel for inserting surgical instruments. In this way, removal of polyps, submucosal myomatous nodes, dissection of synechiae, curettage of the endometrium, etc. can be carried out.
- After all interventions are completed, the hysteroscope and the injected liquid or gas are removed. The patient is sent to the intensive care ward, where she recovers from anesthesia under the supervision of medical staff.
What is laparoscopy?
Before talking about the indications for simultaneous laparoscopy and hysteroscopy, we will define these methods. Laparoscopy is a modern type of surgical intervention that is performed in a closed manner. This means that to access the patient's internal organs, the surgeon does not have to make a large incision in the abdomen, as with a laparotomy.
The laparoscopic operation occurs through 3-4 punctures in the abdominal area, through which instruments and a microscopic camera are inserted. It transmits an image magnified 40 times onto the screen in the operating room, which allows you to clearly and clearly view the patient’s internal organs.
Laparoscopy can be diagnostic and therapeutic. In the first case, it allows you to most accurately establish a diagnosis when other research methods have proven unreliable or ineffective. Therapeutic laparoscopy is performed to cure diseases of the reproductive system. Depending on the situation, diagnostic laparoscopy may turn into therapeutic laparoscopy if the diagnosis is confirmed and the surgeon deems it appropriate.
Recovery after hysteroscopy of the uterus
The recovery period after hysteroscopy is divided into two stages. In the early recovery period, tissues damaged during the procedure are restored—the mucous membrane of the uterus, the muscular wall, and the cervical canal. This period lasts about 2-3 weeks.
The second period takes about six months. At this time, the new endometrium will be regenerated, which must meet the functions assigned to it - grow and be rejected in the process of changing the phase of the menstrual cycle.
Bloody discharge after hysteroscopy
Moderate bleeding is possible in the first 2-3 days after hysteroscopy. This is normal, since during the procedure the cervical canal, endometrium and muscular layer of the uterus are injured. Gradually, the discharge lightens, acquires a yellowish color and continues for about 2-3 weeks. If heavy bleeding develops, you should immediately consult a doctor, as this may be a symptom of serious complications.
Painful sensations after hysteroscopy
Mild to moderate pain after hysteroscopy is normal. They are localized in the lower abdomen and can radiate to the sacrum or lower back. They arise due to stretching of the uterine cavity and injury to the cervix. To alleviate the condition, it is recommended to prescribe “strong” NSAIDs such as ketorol or indomethacin. If the pain increases and becomes unbearable, you should seek medical help immediately, as this may be a sign of serious complications.

In order for the recovery period to go smoothly, you must adhere to several rules:
- Take all medications prescribed by your doctor. As a rule, we are talking about antibiotics that are prescribed prophylactically to prevent the development of infections.
- Avoid vaginal sex until your next period.
- During the period of bleeding, it is better to use pads. Tampons are strictly prohibited.
- Also, during the recovery period it is not recommended to use vaginal suppositories, tablets and creams.
- Refrain from intense physical activity.
- Don't forget about personal hygiene. Toilet of the genital organs should be performed at least 2 times a day, and ideally after each urination and defecation.
- To prevent the development of constipation, follow your diet. Don't forget to empty your bladder in a timely manner.
Differences between laparoscopy and hysteroscopy
When a woman is prescribed laparotomy and hysteroscopy simultaneously for infertility, she should understand that these are two fundamentally different methods with different types of access to the organs of the reproductive system. What they have in common is that these are minimally invasive and gentle procedures. On the Internet on various medical sites and forums there are reviews about laparoscopy and hysteroscopy at the same time, which are not true. We strongly advise you not to listen to online advisors, but to contact your doctor, who will provide the most up-to-date and reliable information.
What complications can hysteroscopy cause?
As with any invasive intervention, complications may develop after hysteroscopy. The most formidable and dangerous of them is perforation of the uterine wall, which is accompanied by bleeding. To eliminate the perforation, repeated surgery is required to suturing the defect. If left untreated, peritonitis may develop.
There may also be other complications:
- Hematometra is the accumulation of blood in the uterine cavity due to the impossibility of its drainage. Clinically manifested by increasing spasmodic pain in the lower abdomen and deterioration in general well-being. For treatment, conservative methods can be used (prescription of drugs that improve uterine contraction or antispasmodics for pathological contraction of the cervix), or surgical methods, in which repeated intervention is performed with evacuation of the intrauterine contents.
- Infectious complications. They are manifested by an increase in body temperature, symptoms of intoxication, and pain in the lower abdomen. A little later, pathological discharge appears, which may have a foul odor.
- Bleeding. Possible after therapeutic hysteroscopy, when, for example, myomatous nodes or polyps are removed. If you experience heavy bleeding, especially if it lasts several days, you should consult your doctor.
In general, hysteroscopy is a low-traumatic intervention and the likelihood of complications after it is much lower than with other, more extensive treatment methods.
What procedures can a gynecologist perform during hysteroscopy?
Hysteroscopy is a diagnostic procedure, however, during it some additional manipulations can be performed, including therapeutic ones:
- Biopsy is a procedure during which a piece of pathologically changed tissue is removed and sent to the laboratory for histological and cytological examination. This allows you to establish a more accurate diagnosis, confirm or exclude the presence of a malignant tumor in the uterus.
- Hysteroscopy allows you to remove various pathological formations protruding into the uterine cavity, such as polyps and fibroids.
- The source of bleeding can be eliminated using electrocoagulation and low temperature (cryosurgery).
- Place contraceptive devices in the fallopian tubes.
The Euroonko clinic in Moscow offers special comprehensive programs for women, for example, hysteroscopy with separate diagnostic curettage of the cervix and uterine body. The cost of the service includes a 6-hour stay in a comfortable hospital, meals, and all related procedures.
When can hysteroscopy be performed?
Most often, gynecologists prescribe hysteroscopy in the following situations:
- Detection of atypical cells based on PAP test results.
- Vaginal bleeding between periods, postmenopause.
- Infertility is when you cannot get pregnant after a year of regular sexual activity.
- Frequent miscarriages.
- The need to clarify the condition of the uterus with scars and fibroids.
- The need to confirm or rule out certain diagnoses using biopsy.
Risks of hysteroscopy
Overall, this is a safe procedure. For two days after hysteroscopy, you may experience slight bleeding from the vagina and cramps in the lower abdomen - this is normal. More serious complications are very rare, occurring in no more than 1% of cases.
At Euroonko, the research is carried out by a highly qualified specialist - Natalya Evgenievna Levchenko, oncogynecologist, professor, doctor of medical sciences. The clinic uses equipment for hysteroscopy from the world's leading manufacturers, which allows the examination to be carried out as comfortably and safely as possible.
Why Euromed In Vitro?
- In city hospitals, hysteroresectoscopy and laparoscopy require hospitalization for 3-5 days. For us, this is surgery of one day or even several hours .
- The high qualifications of our surgeons, anesthesiologists and nurses make such operations as safe as possible and your stay in the clinic comfortable.
- We do not prescribe tests, studies or operations unless absolutely necessary.
- We use the best latest generation equipment.
What alternatives are there to hysteroscopy?
Hysteroscopy can be replaced by some other diagnostic procedures, but not in all cases:
- Transabdominal ultrasound of the pelvic organs through the anterior abdominal wall helps to identify diseases that lead to pelvic pain, menstrual irregularities, vaginal bleeding, and infertility.
- Transvaginal ultrasound is performed with a special probe inserted through the vagina. It allows you to obtain more informative images of the uterus and its appendages.
- Aspiration biopsy of the myometrium. This procedure does not require hysteroscopy: using vaginal speculum, the cervix is visualized and a tube connected to an aspirator is inserted through it.
All these studies are not as informative as hysteroscopy. However, if you start the diagnosis with them, in some cases endoscopic examination of the uterus may not be required. Sometimes these diagnostic methods are used as an alternative if there are contraindications for hysteroscopy for one reason or another.
Book a consultation 24 hours a day
+7+7+78










