Fast Facts About General Anesthesia
Here are some key points about general anesthesia. More detailed and supporting information can be found in the main article.
- The anesthesiologist usually administers a general anesthetic before surgery
- There are some risks associated with the use of general anesthetics, but they are relatively safe when used correctly
- Very rarely, a patient may experience unintentional awakening during surgery
- Side effects of general anesthesia may include dizziness and nausea
- The mechanisms by which anesthesia works are still only partially understood.
General anesthetics cause reversible loss of consciousness and analgesia necessary for surgery . The mechanism of action of anesthetics is not fully understood. There are several theories about this.
General anesthesia is essentially a medically induced coma, not sleep. Anesthetic drugs make the patient indifferent and turn off consciousness .
They are usually administered intravenously or by inhalation . Under anesthesia, the patient does not feel pain and may also experience amnesia.
The drugs will be administered by an anesthesiologist, who will also monitor the patient's vital signs during the procedure.
In this article, we'll look at a number of topics, including the possible side effects of general anesthesia, the risks involved, and some theories about how they work.
Anesthesia for laparoscopic operations
Myth No. 1. For laparoscopic operations, only local anesthesia is used. In fact, almost all laparoscopic surgeries require general anesthesia. Only sometimes (for short-term interventions and during diagnostic procedures) anesthesia of a limited area of the body is used - spinal epidural anesthesia or regional anesthesia. In this case, the injection is given in the spine area, and sensitivity is immediately lost in the entire lower part of the body. In this case, unlike deep (general) anesthesia, the patient remains conscious. This anesthesia allows you to maintain communication with the patient during the operation to avoid complications.
To use spinal-epidural anesthesia, the doctor must have experience and the highest qualifications, since minimal deviation from the technique causes negative consequences for health. In the medical field, not a single case of severe complications of spinal-epidural anesthesia has been recorded, since such anesthesia in the clinic is carried out by anesthesiologists with at least 10-15 years of practical experience.
Myth No. 2. You can avoid general anesthesia for laparoscopy. The choice of anesthesia method during laparoscopic operations is within the competence of the physician. The exception is cases when the doctor does not find contraindications for the use of either local or general anesthesia - then the patient’s opinion may have weight when making the final decision. Doctors do not recommend refusing general anesthesia, because it is much calmer and more convenient for the patient to fall asleep before the operation and wake up healthy than to listen to medical terms for an hour, flinching at every incomprehensible word. Myth No. 3. General anesthesia during laparoscopy is dangerous! The experience of Best Clinic doctors says that general anesthesia is a stopping factor that frightens some patients, especially older ones. This negative attitude towards general anesthesia has been formed over many years and is based on the negative experience of friends and relatives who have undergone operations in municipal hospitals. In recent years, everything has changed, but you can still hear that “after general anesthesia you may not wake up” or “you may lose your mind while recovering from anesthesia.”
In fact, these statements are nothing more than myths that have no relation to modern anesthesiology. General anesthesia during laparoscopy is safe and comfortable. A variety of methods and areas of anesthesia opens up the opportunity for the doctor to choose a method that suits a particular patient, focusing on age, health status and type of operation. The methods of intravenous, inhalation and endotracheal (combined) anesthesia deserve the greatest attention in practice.
Myth No. 4. Intravenous anesthesia can cause severe allergies. Any medicine can cause an allergy, so before undergoing surgery using intravenous anesthesia, our patients undergo a specific test for sensitivity to the anesthetic drug. To reduce risks to zero, Best Clinic uses the modern hypoallergenic drug Diprivan.
Intravenous anesthesia is used only for short-term laparoscopic operations, the duration of which is up to 20 minutes. This group of procedures includes uterine curettage and other simple gynecological operations. In general, recovery from short-term intravenous anesthesia is easy and quick. In our medical center, an assistant anesthesiologist - an anesthetist - is with the patient throughout the entire period of restoration of consciousness.
Myth No. 5. Inhalation anesthesia is not used for laparoscopic operations because it does not provide complete pain relief and has a bad effect on the body. We still hear from some representatives of the older generation about the dangers and unreliability of inhalation anesthesia. “Experts” assure that you can recover from such anesthesia right on the operating table. However, such “horror stories” are completely untrue:
- Firstly, toxic nitrous oxide has not been used for inhalation anesthesia for a long time; it has given way to safe inert gases - xenon and sevoran. The gas enters the body through the mask, causing muscle relaxation and temporary loss of consciousness and sensitivity.
- Secondly, to carry out inhalation anesthesia, the latest anesthesia equipment is used (at Best Clinic this is the Draeger Primus device), which monitors the patient’s most important vital signs during the operation. Thus, the doctor instantly notices any changes in the condition of the person being operated on and takes action. Premature recovery of the patient from anesthesia is excluded.
The main advantage of inhalation anesthesia over intravenous anesthesia is considered to be safety, because the gas is removed from the body without being absorbed and without having a direct effect. When performing laparoscopy, inhalation techniques are used for operations that last up to 45 minutes - removal of cysts or fibroids of the cervix and uterus, dissection of adhesions, removal of appendicitis, etc.
Myth No. 6. After endotracheal anesthesia, you can be damaged in your mind, become mentally retarded, inhibited, etc.
Such “horror stories” have no scientific basis. Modern complex or endotracheal anesthesia is considered the standard of pain relief throughout the civilized world. Why? Because this technique:
- puts the patient into the deepest sleep through the simultaneous use of intravenous and inhaled drugs;
- provides the doctor with the highest degree of control over the patient’s condition, because there is direct access to the respiratory system.
Oxygen is constantly supplied to the tissues of the body. As a result, the patient can remain unconscious for a very long time, without harm to health or any significant changes in condition. Recovery from anesthesia takes place, as in other cases, under the supervision of an anesthesiologist. The person returns to consciousness quickly enough - in no more than two hours. Endotracheal anesthesia is used for long surgical procedures - removal of the uterus, excision of large areas of tissue, etc.
Story
General anesthetics have been widely used in surgery since 1842, when Crawford Long prescribed diethyl ether to a patient and performed the first painless operation.
On October 16, 1846, American dentist and surgeon Thomas Morton first administered ether anesthesia to a patient to remove a submandibular tumor.
In Russia, the first operation under anesthesia was performed on February 7, 1847 by Pirogov’s friend at the professorial institute, Fyodor Inozemtsev.
Pirogov himself performed the operation using anesthesia a week later. Over the course of a year, 690 operations were performed under anesthesia in 13 cities of Russia, 300 of which were performed by Pirogov!
Soon he took part in military operations in the Caucasus. Here, for the first time in the history of medicine, he began to operate on the wounded with ether anesthesia. In total, the great surgeon performed about 10,000 operations under ether anesthesia.
Laparoscopy in gynecology: when is it applicable?
Surgeries on the abdominal and pelvic organs without... an incision? What once could have been the plot of a fantasy story is now a reality. The topic of our article is laparoscopy. We talked about its use in gynecological practice with Radmila Borisovna Prokhorenko, a gynecologist at the Expert Clinic Irkutsk.
— Radmila Borisovna, how often is laparoscopy used in gynecology? What is this method?
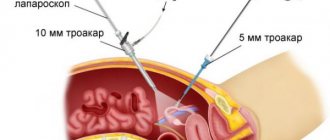
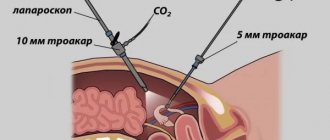
“This is a modern surgical method that is widely used in the treatment of many diseases of the abdominal organs, including gynecological ones. Its main feature is that it is minimally invasive; manipulations are carried out using endoscopic instruments. First, small holes are formed in the anterior abdominal wall. Then special hollow tubes - trocars - are inserted into them. Instruments and a miniature camera are inserted through the trocars.
Diagnostic laparoscopy is performed if other diagnostic methods are ineffective. For example, if you suspect an ectopic pregnancy, with chronic pelvic pain syndrome, or infertility of unknown origin. During the procedure, the identified pathology is eliminated, and thus, diagnostic laparoscopy becomes therapeutic.
— Is laparoscopy used for female infertility?
- Yes, very wide. The most common form of female infertility is tubal-peritoneal, which involves laparoscopic dissection of adhesions and tubal plasty. If there are pronounced structural changes in the fallopian tubes, they are removed.
Also, one of the causes of infertility may be polycystic ovary syndrome. In this case, if hormonal treatment is ineffective, patients undergo drilling (point puncture) of the ovaries using laparoscopic access.
Another cause of infertility is minor forms of endometriosis. They can lead to immunological infertility. In this case, these lesions are excised through laparoscopic access. Subsequently, the woman receives hormonal treatment.
— A relatively common gynecological pathology is uterine fibroids. Is laparoscopy used in the treatment of this disease?
- Yes, to remove fibroids. This is called laparoscopic myomectomy. How is it made? The principle of operation is the same. Through small holes in the abdominal wall, special instruments are inserted into the abdominal cavity. With its help, the serous, muscular lining of the uterus is dissected. Myomatous nodes are removed, after which the uterine wall is sutured.
For more information about removing uterine fibroids, read our article: Fibroids: to remove or not? When will myomectomy help?
— Is laparoscopy used when removing the uterus?
- Yes. In this way, you can do uterine amputation (removal of the uterus without the cervix), hysterectomy (removal of the uterus with the cervix) both with and without appendages. This requires good surgical skills and special equipment (morcellator), which allows you to crush and remove the amputated organ through an 11-mm trocar.
— What anesthesia is used in gynecology during laparoscopy?
— This is endotracheal anesthesia using muscle relaxants. The patient cannot breathe on her own during surgery; an artificial lung ventilation device does this for her.
— How does a doctor decide that a woman is best suited for treatment using the laparoscopic method?
— If possible, it is better to perform the operation using a laparoscopic approach, since this is associated with minor surgical trauma, less pain and blood loss, quick recovery, and a lower likelihood of scarring and infectious complications. However, there are also contraindications here.
- Which?
— Literally 20 years ago, one of the contraindications was a one-time abdominal surgery. Now the situation has changed; the approach to choosing a treatment method is determined individually in each specific case. For example, if a woman has a history of some serious surgical intervention (part of the intestine was removed, there was diffuse peritonitis or large blood loss, that is, when we suspect a massive adhesive process in the abdominal cavity), then the laparoscopic method is contraindicated. Uncomplicated appendectomy or cesarean section, of course, are not a contraindication.
Contraindications also include: severe obesity or exhaustion of the patient (cachexia), coagulopathy (blood clotting disorder), diseases of the cardiovascular and respiratory systems, late pregnancy, acute infectious diseases.
You can make an appointment with an obstetrician-gynecologist at the Expert Clinic Irkutsk here
The editors recommend:
A mystery disease: what is endometriosis? Who can benefit from hysteroscopy?
For reference:
Prokhorenko Radmila Borisovna
Graduate of Irkutsk State Medical University with a degree in General Medicine in 1996. In 1998, she completed her internship in obstetrics and gynecology. Over the years I have undergone advanced training. Currently, he is the head of the gynecological department, obstetrician-gynecologist at Clinic Expert, Irkutsk. Receives at the address: Irkutsk, st. Kozhova, 9A.
Side effects
Nausea is a common side effect of general anesthesia.

There are a number of potential side effects of anesthesia.
Some people may experience none, others several. None of the side effects are particularly long-lasting and usually occur immediately after anesthesia.
Side effects of general anesthesia include:
- temporary confusion and memory loss, although this is more common in older people
- dizziness
- difficulty urinating
- bruising or soreness from the IV
- nausea and vomiting
- trembling and chills
- sore throat due to breathing tube
Risks
In general, general anesthesia is safe. Even very sick patients can be safely anesthetized. The surgical procedure itself involves much greater risk.

Modern general anesthesia is an incredibly safe procedure.
However, older adults and those undergoing lengthy procedures are most at risk for complications . These findings may include postoperative confusion , heart attack, pneumonia, and stroke.
Some specific conditions increase the risk for a patient undergoing general anesthesia, for example:
- obstructive sleep apnea, a condition in which people stop breathing while sleeping
- seizures
- existing heart, kidney or lung disease
- high blood pressure
- alcoholism
- smoking
- previous negative reactions to anesthesia
- medications that may increase bleeding - aspirin, warfarin , for example
- drug allergy
- diabetes
- obesity or overweight
Unintentional intraoperative awakening
This refers to rare cases where patients report remaining conscious during surgery, long after the anesthetic should have taken effect . Some patients are aware of the procedure itself, and some may even feel pain.
Unintentional intraoperative awakening is incredibly rare, affecting approximately 1 in every 19,000 patients under general anesthesia.
Because of the muscle relaxants used at the same time as anesthesia, patients are unable to let their surgeon or anesthesiologist know that they still know what is happening.

Unintentional intraoperative awakening is more likely during emergency surgery.
Patients who experience unintentional intraoperative awakening may suffer from long-term psychological problems. Most often, awareness is short-lived and only sounds, and occurs before or at the very end of the procedure.
According to a recent large-scale study of this phenomenon, patients experienced involuntary twitching , stabbing pain, pain, paralysis and suffocation, among other sensations.
Because unintentional intraoperative awakening is rare, it is unclear exactly why it occurs.
Laparoscopy of uterine fibroids
In Russia, laparoscopy has been performed for about 15 years. Good results and positive reviews of laparoscopic removal of ovarian cysts have become the basis for the wider introduction of this method in gynecology. Now they are trying to replace almost all abdominal surgeries on the pelvic and abdominal organs with this manipulation. This popularity of the technique is justified by minimal trauma and preservation of the functions of the reproductive system, minimal risks during surgery, and a quick recovery period for the patient.
Laparoscopy is also used as a diagnostic method (MRI and ultrasound are not always informative). Based on the data obtained, surgeons can determine the extent of resection - conservative or radical. The main indications for surgical intervention are rapid growth or large size of the formation, pressure on regional tissues with limitation of their functions, suspicion of atypia, identification of subserous nodes, internal deformations, infertility caused by the tumor.
The patient’s preparation is standard: tests, bowel cleansing, administration of sedatives the day before surgery. Depending on the clinical picture, there are several ways to remove adenomyoma. Radical involves eliminating the pathology of the uterus and cervix; in some cases, the cervix is preserved. Conservative - enucleation or excision of a small area of the base tissue while preserving reproductive function.
The operation is performed under general anesthesia or epidural anesthesia. To insert the instruments, 3-4 punctures are made in different places of the abdominal cavity. To provide access to the organ, carbon dioxide is injected into the cavity. Through the remaining punctures, a camera with a lighting device connected to a monitor and surgical instruments are inserted. In this way, it is possible to remove even large fibroids, and postoperative sutures will be slightly noticeable.
Types
There are three main types of anesthesia . General anesthesia is just one of them.
Local anesthesia is another option. It is done before minor surgeries such as toenail removal. This reduces pain in small, focused areas of the body, but the person receiving treatment remains conscious.
Regional anesthesia is another type. It numbs the entire part of the body - the lower half, for example, during childbirth. There are two main forms of regional anesthesia: spinal anesthesia and epidural anesthesia.
Spinal anesthesia is used for operations on the lower extremities and abdomen. The anesthetic is injected through a special very thin needle into the intervertebral space of the lumbar region . Epidural anesthesia is used for long-term pain relief. Can be used for operations on the chest, abdomen, and lower extremities. During an epidural, a thin plastic catheter is inserted through which a local anesthetic is injected. Pain relief can last as long as needed.
Read more about pain relief during operations.
- home
- For patients
- Anesthesia during operations
When performing surgical interventions, we use all main types of anesthesia.
- Local anesthesia, which provides pain relief directly to the surgical site, is used for minor open surgeries.
- Epidural anesthesia, which leads to pain relief of the lower half of the body, is performed in cases where contact between the doctor and the patient is necessary. This type of anesthesia is possible for large open operations on the pelvic organs.
- General anesthesia, which puts the patient into deep sleep, is used for all hysteroscopic and laparoscopic operations.
The most commonly used type of anesthesia in my practice is general multicomponent anesthesia with artificial ventilation. This type of anesthesia provides excellent conditions for the surgeon to perform the operation, minimizes blood loss during the operation, and creates an ideal psycho-emotional mood for the patient before and after the intervention.
Before the operation, the anesthesiologist examines the patient, conducts an additional physical examination, gets acquainted with the examination data and tests, and selects the optimal type and dosage of anesthetics for a particular patient.
We strive to use the most gentle controlled anesthesia when performing minimally invasive surgical operations. In this regard, we have abandoned the use of medical gases (nitrous oxide, fluorotane, xenon and others). We use multi-anesthesia, simultaneously using an individually selected set of infusion and injection drugs. It allows:
- control the depth of anesthesia required during a given operation for a particular patient;
- relax the muscles of the abdominal wall;
- ensure rapid recovery of the patient from anesthesia after completion of the operation.
Multi-anesthesia is carried out using modern medications that do not cause allergic or other side effects and do not affect memory.
“So, has the operation already been completed?” - this is the most common question from patients after surgery, which the anesthesiologists at the clinic where I perform operations are proud of. Premedication is carried out in the ward so that the patient falls asleep and does not see the operating room environment. The created calm psycho-emotional mood, controlled depth and duration of anesthesia provide ideal conditions for the blood supply to the internal organs and the hemodynamics of the patient’s body. This makes it easier for the surgeon to perform the operation, prevents the development of intraoperative complications and ensures a smooth course of the postoperative period. Multi-anesthesia creates optimal conditions for the patient to recover from anesthesia: the patient wakes up in the room immediately after the end of the operation.
When performing artificial ventilation of the lungs, we use both classical intubation and laryngeal masks with a catheter, depending on the volume of the operation performed. During the operation, an excellent expert-class anesthesia-respiratory apparatus is used. Reliable and informative monitoring equipment controls the depth of anesthesia based on respiratory and hemodynamic parameters.
For intensive treatment, the clinic always has an intensive care unit ready with an artificial ventilation device and monitoring equipment. Recovery from anesthesia is carried out under the control of respiratory parameters, hemodynamics and the function of the central nervous system.
We consider it very important to have an anesthesiologist on duty around the clock after surgery. The anesthesiologist who performed the anesthesia stays with the patient for the next 24 hours along with the surgeon on duty from the operating team that performed the operation.
When you write a letter, know that it goes to me on my personal email.
[email protected] +7 495 222-10-87 Telemedicine
I always answer all your letters myself. I remember that you trust me with the most valuable things - your health, your destiny, your family, your loved ones, and I do everything possible to justify your trust. Every day I spend several hours answering your letters. By sending me a letter with a question, you can be sure that I will carefully study your situation and, if necessary, request additional medical documents. Vast clinical experience and tens of thousands of successful operations will help me understand your problem even from a distance.
Many patients do not require surgical treatment, but rather properly selected conservative treatment, while others require urgent surgery. In both cases, I outline a course of action and, if necessary, recommend additional examinations or emergency hospitalization. It is important to remember that some patients require preliminary treatment of concomitant diseases and proper preoperative preparation for successful surgery. In the letter, be sure (!) to indicate age, main complaints, place of residence, contact phone number and email address for direct communication. So that I can answer all your questions in detail, please send along with your request scanned reports of ultrasound, CT, MRI and consultations of other specialists. After reviewing your case, I will send you either a detailed response or a letter with additional questions. In any case, I will try to help you and justify your trust, which is the highest value for me.
Sincerely yours, surgeon Konstantin Puchkov
Local vs General
There are a number of reasons why general anesthesia may be chosen over local anesthesia.
This choice depends on age, health and personal preference.
The main reasons for choosing general anesthesia are:
- The procedure will likely take a long time.
- There is a possibility of significant blood loss.
- This may affect breathing, for example during breast surgery.
- The procedure will make the patient feel uncomfortable.
- It is difficult for the patient to maintain a forced position during surgery.
The purpose of general anesthesia is to induce:
- pain relief or elimination of the natural response to pain
- amnesia or memory loss
- immobility or elimination of motor reflexes
- dream
- relaxation of skeletal muscles
However, the use of general anesthesia poses a higher risk of complications than local anesthesia. If the surgery is minor, then the patient is offered local anesthesia, especially if he has a condition such as sleep apnea or other risk factors.
1.What is laparoscopy and why is it performed?
Laparoscopy
is an operation using a thin, lighted tube inserted through a small incision into the abdominal cavity to diagnose problems with the internal or pelvic organs in women. Laparoscopy is performed to identify problems such as cysts, adhesions, fibroids, and to detect infections. During laparoscopy, tissue samples may be taken using a laparoscope for further biopsy.
In many cases, laparoscopy can be performed instead of abdominal surgery, which involves making a large incision in the abdomen. Laparoscopy, unlike laparotomy, does not cause much stress for the patient and is ideal for simple operations. Often, the patient does not even need to stay overnight in the hospital.
Why perform laparoscopy?
Laparoscopy allows:
- Check for growths (eg tumors) in the abdomen or pelvis and, if possible, take samples.
- Diagnose conditions such as endometriosis, ectopic pregnancy, or pelvic inflammatory disease (PID).
- Identify the reasons why a woman cannot get pregnant. These could be cysts, adhesions, fibroids or infections. Laparoscopy can reveal the cause of infertility.
- Do a biopsy.
- Determine whether cancers diagnosed in other parts of the body are spreading to the abdominal organs.
- Check for damage to internal organs, such as the spleen, after injury or accident.
- Perform a tubal ligation.
- Operate on a hiatal hernia or inguinal hernia.
- If necessary, remove organs such as the uterus, spleen, gallbladder (laparoscopic cholecystectomy), ovaries or appendix (appendectomy). Partial removal (resection) of the colon can also be done using laparoscopy.
- Find the cause of sudden or persistent pain in the pelvic area.
A must read! Help with treatment and hospitalization!
Preoperative assessment
Before undergoing general anesthesia, patients should undergo a preoperative assessment to determine the most appropriate medications, their amount and combination.
Some of the factors that should be examined in the preoperative assessment include:
- body mass index (BMI)
- disease history
- age
- medications taken
- time before anesthesia
- alcohol or drug use
- use of pharmaceuticals
- examination of the oral cavity, teeth and respiratory tract
- cervical spine mobility study
It is important that you answer these questions accurately. For example, if a history of alcohol or drug use is not mentioned, insufficient anesthesia may be given, which could lead to dangerously high blood pressure or unintentional intraoperative awakening.
Stages
The Gödel classification, developed by Arthur Ernest Gödel in 1937, describes four stages of anesthesia. Modern anesthetics and updated methods of drug have improved the speed of onset of anesthesia , overall safety and recovery, but the four stages remain essentially the same:

General anesthesia is similar to a comatose state and different from sleep.
Stage 1 or induction . This phase occurs between the administration of the drug and loss of consciousness. The patient moves from analgesia without amnesia to analgesia with amnesia.
Stage 2, or arousal stage . The period after loss of consciousness, characterized by agitated and delirious activity. Breathing and heart rate become erratic, and nausea, dilated pupils, and holding your breath may occur.
Due to irregular breathing and the risk of vomiting, there is a danger of suffocation. Modern fast-acting drugs are aimed at limiting the time spent on the 2nd stage of anesthesia.
Stage 3 or surgical anesthesia : muscles relax, vomiting stops, breathing is suppressed. Eye movements slow and then stop. The patient is ready for surgery
Stage 4, or overdose : if too much anesthetic has been administered, then depression of the brain stem occurs . This leads to respiratory and cardiovascular collapse.
The anesthesiologist's priority is to get the patient to stage 3 anesthesia as quickly as possible and keep him there throughout the operation.