In modern medical practice, the concept of hysteroscopy of the uterus is often encountered. Hysteroscopy of the uterus is one of the most effective methods of examining the uterine cavity from the inside using a special device with a video camera (hysteroscope) for timely diagnosis and detection of intrauterine pathologies, as well as the possibility of performing some operations without incisions and sutures. Depending on the purpose for which this study is performed, hysteroscopy can be divided into two types: diagnostic and surgical. To examine or confirm the diagnosis, diagnostic hysteroscopy is performed on an outpatient basis. This procedure takes from 5 to 25 minutes and does not require anesthesia (in some cases, local anesthesia is possible). Surgical hysteroscopy is a surgical intrauterine intervention, the operation is performed under short-term general anesthesia.
Preparation for hysteroscopy
Before this procedure, you need to undergo a general examination by a gynecologist and pass a number of tests:
- general analysis of urine and blood;
- HIV testing;
- vaginal smear
A complete list of necessary tests is provided by the medical institution.
You also need to undergo an examination, which includes an examination by a therapist, an ECG, fluorography, and an ultrasound of the pelvic organs.
Hysteroscopy is prescribed a few days after the end of menstruation. On the day of hysteroscopy, you should not drink or eat. When preparing for hysteroscopy of the uterus, you should abstain from sexual intercourse for three days before the procedure. Avoid taking any medications for a week (unless prescribed for medical reasons).
Hysteroscopy is a section of modern operative gynecology
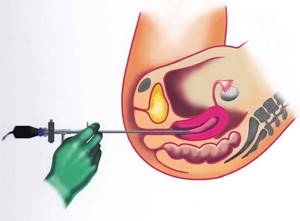
Hysteroscopy is an examination of the uterine cavity using an optical system that is inserted through the vagina, and then the cervix and uterine cavity. After inserting the system (a thin tube, 3.2 to 10 mm thick, which contains a light-conducting fiber, a channel for fluid and instruments), and then filling the uterus with a sterile solution (to straighten the uterus and rinse the cavity), the walls of the uterus are examined from the inside. The image is displayed on the monitor using a special video camera. In some cases, you can record the resulting video (Fig. 1-2).
Rice. 1. General view of the operating room during hysteroscopy
Rice. 2. The hysteroscope is inserted into the uterine cavity
During hysteroscopy, the walls of the uterus are examined from the inside. The cervical canal and the mouths of the fallopian tubes are also examined, which is very important for infertility (Fig. 3).
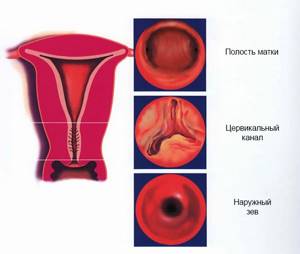
Rice. 3. Normal appearance of the cervix, cervical canal and uterine cavity
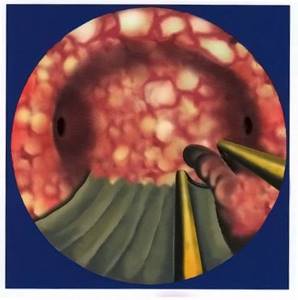
If the gynecologist sees changed areas of the mucous membrane, you can take a targeted biopsy (a piece of tissue) or cauterize the area (Fig. 4).
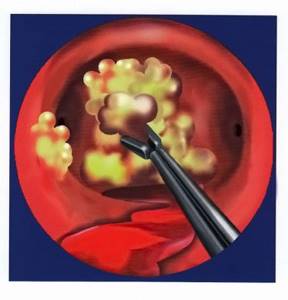
Rice. 4. Biopsy of an area suspicious for endometrial cancer
If necessary, it is possible to remove almost any intrauterine pathology, for example, removal of endometrial and cervical canal polyps (Fig. 5-6).
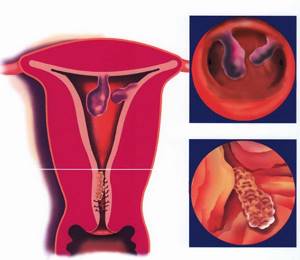
Rice. 5. This is what polyps of the endometrium and cervical canal look like
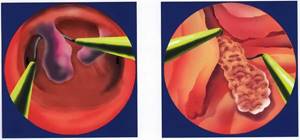
Rice. 6. Removal of polyps with an electric loop during hysteroresectoscopy
This is what laser removal of an endometrial polyp looks like:
Sometimes polyps are so large that they are difficult to remove. For this purpose, a hysteroresectoscope .
In addition, with hysteroscopy, it is possible to dissect the intrauterine septum, dissect adhesions and synechiae, enucleate myomatous nodes, remove foreign bodies (for example, a spiral) or remnants of the fertilized egg, as well as resection of the endometrium (Fig. 7-12).
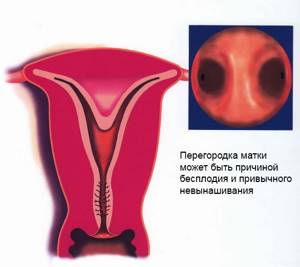
Rice. 7. General view of the uterine septum. It is worth distinguishing the uterine septum from a bicornuate uterus
Rice. 8. Removal of the uterine septum
Video of uterine septum removal performed by me:
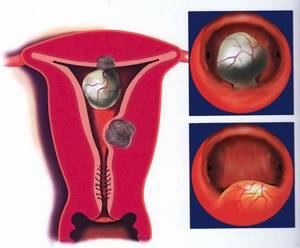
Rice. 9. Submucous uterine leiomyoma (different types)
Rice. 10. Resection of submucosal leiomyoma (hysteroresectoscopic myomectomy)
Removing a myomatous node using a hysteroresectoscope in a typical case may look like this:
In complex cases, for example, with several nodes and adenomyosis, like this:
In the office version without anesthesia using LASER it’s like this:
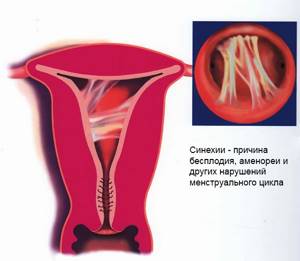
Rice. 11. Synechia in the uterine cavity
Rice. 12. Separation of intrauterine synechiae
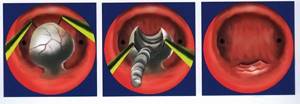
In addition, hysteroscopy can be used to perform endometrial resection and ablation (Figure 13) for chronic uterine bleeding, avoiding the need for hysterectomy (removal of the uterus).
Rice. 13. Resection of hyperplastic endometrium using a hysteroresectoscope
Statistics show that a diagnosis made by a doctor and not verified by hysteroscopy can be wrong in almost a third of patients. But the diagnosis confirmed by hysteroscopy is confirmed during other operations in 90% of cases. In addition, almost half of women are also diagnosed with combined pathology, i.e. in addition to the known disease, another, the symptoms of which were masked by the underlying disease. For example, an endometrial polyp that was located behind a submucous leiomyomatous node.
Hysteroscopy is a microsurgical intervention. It allows you to avoid large, abdominal operations, in which the wall of the abdomen is cut, and then the wall of the uterus. It is quite logical that minimal intervention also produces minimal consequences, which is why hysteroscopic surgery is the main method of intervention in women of reproductive age. After all, any intervention in the uterine cavity leaves a mark that can result in subsequent infertility.
What types of hysteroscopy are there:
- office hysteroscopy
- “diagnostic” hysteroscopy (Fig. 14)
- operative hysteroscopy - resectoscopy (Fig. 15)

Rice. 14. Standard hysteroscope with connected camera, light guide and fluid supply hose
Rice. 15. Hysteroresectoscope - a special hysteroscope with a device for working with electric loops and other electrodes (Fig. 16)

Rice. 16. Instruments used in hysteroscopy and hysteroresectoscopy
What can be done with a hysteroscope:
- make the correct diagnosis (endometrial hyperplasia and cancer, fibroids, adenomyosis, polyp, synechiae in the uterine cavity, uterine septum, etc.)
- remove the polyp (Fig. 6)
- remove the myomatous node (Fig. 10)
- cut the intrauterine septum (Fig.


- dissect intrauterine synechiae (Fig. 12)
- remove the ingrown intrauterine device and other foreign bodies (for example, fragments of fetal bones after unsuccessful abortions)
- perform surgical sterilization
- eliminate the causes of persistent bleeding by performing resection and/or ablation of the endometrium (Fig. 13)
What are the indications for hysteroscopy:
- menstrual irregularities (especially bleeding)
- suspicion of intrauterine pathology (submucous myoma, endometrial hyperplasia and polyp, adenomyosis, malformations, synechiae in the uterine cavity, foreign body in the uterine cavity, as well as endometrial cancer)
- infertility
- recurrent early pregnancy loss with suspected anatomical cause
- surgical sterilization
Hysteroscopy is a microsurgical intervention. It allows you to avoid large, abdominal operations in which the abdominal wall and uterus are cut. It is clear that minimal intervention also produces minimal negative consequences, therefore hysteroscopy should be the main method of intrauterine surgery in women of reproductive age.
Contraindications for hysteroscopy:
- clear suspicion of cancer
- acute inflammatory process of the genital organs
- the presence of gynecological pathology, which cannot be cured with hysteroscopy or the risk outweighs the benefit
- diseases with a significant risk of developing complications associated with fluid overload, anesthesia (heart failure, renal failure, pulmonary edema, severe acute inflammatory processes, other severe, decompensated diseases).
Anesthesia method for hysteroscopy:
- usually general anesthesia
- although local anesthesia may be used
- office hysteroscopy is performed without anesthesia (although, in some cases, it causes pain)
Length of hospital stay:
- 1 day
- after resectoscopy with removal of a large node and/or endometrium, a stay of up to 2-3 days is possible
Where is hysteroscopy performed:
- hysteroscopy is performed in a hospital
- office hysteroscopy can be performed on an outpatient basis
What complications are possible with hysteroscopy:
- uterine perforation, cervical injury
- bleeding
- fluid overload with development of pulmonary edema
- air embolism (up to the death of the patient)
- infectious complications
What tests are necessary before hysteroscopy (order No. 676 of the Ministry of Health of Ukraine):
- Blood type, Rh
- Complete blood count + platelets
- General urine analysis
- Blood glucose
- Coagulogram
- Electrolytes, proteins, liver, kidney. complex
- Blood for RW, HIV, HbsAg, HCV
- ECG, therapist
- Fluorography
- Vaginal smear
- Cytogram of the cervix
- Colposcopy
The doctor who will perform the hysteroscopy must be familiar with the results of the ultrasound examination.
A couple of comments about preparing for hysteroscopy:
Unfortunately, in most medical institutions in the city and region, hysteroscopy has very significant disadvantages:
1. Outdated foreign or inexpensive Russian equipment with large-diameter optics is used, which requires expansion of the cervical canal, injures the cervix and has undesirable consequences for women planning to have children 2. Outdated equipment (hysteromat) is not used or is used, allowing for precise regulation and control intrauterine pressure, the amount of fluid introduced and removed, which leads to extravasation of an increased amount of fluid, pulmonary edema. Increased pressure in the uterine cavity leads to cases of air embolism and even death
Therefore, the key to successful hysteroscopy is not only the qualifications of the doctor, but also the availability of modern equipment, as well as the doctor’s ability to use all the capabilities of modern hysteroscopy.
I don’t think it’s superfluous to mention the safety rules during hysteroresectoscopy:
- If the difference between the injected and withdrawn fluid is 1000 ml or more, stop the operation
- Limit the total operation time to 50 minutes
- Rules for using a hysteropump: maximum flow rate 200 ml/min, flushing pressure - 75 mmHg, suction pressure - 0.25 bar
- In this case, it is permissible to briefly exceed these parameters for a period of no more than 5 minutes.
- At the first signs of hypervolemia and the anesthesiologist reports a problem, stop the operation within 1 minute
- In case of risky interventions, the team’s readiness to switch to laparoscopy.
Digests on hysterosopia can be viewed here.
How is surgical hysteroscopy performed?
All manipulations are performed on a gynecological chair. Most often, general anesthesia is used during hysteroscopy to avoid pain. After treating the patient’s external genitalia with an alcohol solution, the cervical canal is carefully dilated and a hysteroscope is inserted into the uterus. Next, a thorough and consistent examination of the walls of the uterine cavity, the mouths of the fallopian tubes and the cervical canal is performed. Based on this examination, a diagnosis is established, and if necessary, surgical treatment is performed (biopsy, curettage, removal of polyps, myomatous nodes and other procedures). All material removed during surgery is sent for research to make a more accurate diagnosis.
When is diagnostic hysteroscopy needed?
The indications for office and regular hysteroscopy are almost the same - with the difference that diagnostic hysteroscopy is not advisable in the presence of serious problems: large polyps, septa, myomatous nodes. In other words, if an operation is planned, and not just a biopsy, then it makes sense to immediately perform a regular therapeutic hysteroscopy in order to combine examination and surgical intervention.
Diagnostic hysteroscopy is used primarily for examination of infertility and if an intrauterine pathological process is suspected.
Recovery after hysteroscopy
Within a few hours after the end of this operation, the patient is usually discharged from the hospital. In the postoperative period, minor or moderate pain in the lower abdomen is possible. This is absolutely normal, because... During the hysteroscopy procedure, the uterine cavity is stretched with liquid or gas. Small bleeding for 2-3 days is also acceptable, because the mucous membrane and blood vessels inside the uterus are injured. If pain or bleeding increases, you should immediately consult a doctor.
For effective recovery in the postoperative period, a number of recommendations must be followed:
- observe sexual rest for 3-4 weeks;
- It is forbidden to visit the bathhouse and sauna, as well as take a bath for at least 3 weeks;
- Avoid intense physical activity and heavy lifting for a month.
Are there any side effects or complications from hysteroscopy?
The most common side effects of the procedure are bleeding and minor pain, as mentioned above. Very rarely, small holes in the uterus from the hysteroscope are possible. If this happens, you must stay in the hospital overnight. It is also possible, although not common, to have an infection of the uterus as a result of hysteroscopy.
You should contact your doctor if you have any problems such as:
- Temperature.
- Unexplained pain that is not relieved by pain medication.
- Increased flow, which is dirty and unpleasant.
- Heavy bleeding.
Contraindications to hysteroscopy
Like any surgical intervention, hysteroscopy has a number of contraindications:
- developing pregnancy;
- malignant neoplasms in the cavity and cervix;
- infectious diseases (sore throat, flu, pneumonia, etc.);
- acute inflammatory diseases of the genital organs;
- cervical stenosis;
- uterine bleeding;
- serious chronic diseases of internal organs (heart, liver, kidneys).
What are the different types of hysteroscopy?
- By purpose, diagnostic, therapeutic and control hysteroscopy is distinguished. There is also hysteroresectoscopy - but this is already a full-fledged surgical intervention. This division is, in fact, arbitrary, because often during the examination there is a need to simultaneously perform one or another surgical procedure.
- Depending on the type of stretching medium, hysteroscopy can be gas or liquid. In order for the walls of the uterus to straighten out and make it possible to see them perfectly, it is necessary to expand the organ and stretch it. To do this, either carbon dioxide or a liquid (sterile water, saline solution, glucose solution, etc.) is injected into the uterine cavity.
Hysteroscopy to remove polyps
Polyps are often found in the cervix and uterine cavity. Polyps are pathological neoplasms on the mucous membrane. They are attached to the uterus by a base or stalk and have a smooth or ribbed surface. The presence of polyps in the uterus can cause many problems for women and is characterized by the following manifestations: spotting between menstrual cycles, nagging pain in the lower abdomen or pain during sexual intercourse. Therefore, timely treatment of these formations is necessary. The most effective method of solving this problem is hysteroscopy. Preparation for the operation and the procedure itself were described above. After the doctor finds the site of attachment of the polyp, he cuts off the stalk of the polyp using flexible scissors. Then the doctor clamps the cut polyp with forceps and carefully removes it from the uterine cavity.
Hysteroscope

The procedure is an examination of the inside of the uterus using a hysteroscope. This device is a thin tube with a diameter of about half a centimeter with an optical system and a light source, which allows you to perform all manipulations not blindly, but accurately. Hysteroscopes can be rigid or flexible.
Hysteroscopes are divided into diagnostic and operational. Operating rooms allow for therapeutic manipulations, as they are equipped with an instrumental channel through which a medical instrument is inserted.
The diagnostic device allows you to examine the inner surface of the uterus in order to then determine treatment tactics.
Doctor's comment

Are you scheduled for office hysteroscopy, but you doubt the advisability of it? But, unlike surgery, your body will not be exposed to anesthetics, and after the examination you can go home. Meanwhile, thanks to the capabilities of the equipment used, it is possible to detect even pathology whose size does not exceed 2 mm. Moreover, the identified deviation can be immediately eliminated. It’s not for nothing that office hysteroscopy is called the “gold standard” in gynecology. Perhaps you are afraid of the examination? But the diameter of the instrument does not exceed three millimeters, so the procedure is painless, and its duration is no more than 20 minutes. By the way, during the procedure you will be able to watch the doctor’s actions on the monitor and even ask him questions that interest you. Do you still have doubts? Call or make an appointment and we will discuss your upcoming examination together.
Endoscopist Natiya Vitalievna Chekhoeva
Why is it better to do office hysteroscopy at the Swiss University Hospital?
- Our Center employs doctors of the highest category, who have performed more than 1,000 gynecological examinations; each of our specialists is able to skillfully perform more than 100 types of operations in their specialization.
- Every year, doctors at our clinic consult more than 5,000 patients; many of our specialists are consultants in other well-known medical institutions.
- The specialists of our clinic, using innovative methods in examination and treatment, have achieved amazing results in solving the problem of infertility. Our gynecologists and surgeons have accounted for more than 600 children born whose mothers were diagnosed with infertility.
- We are one of the few domestic clinics operating according to the traditions of Western European universities. We also cooperate with leading university clinics in France, Switzerland and Germany.










