Red blood cells and protein in urine
are discovered, as you might guess, during a general urine test. This study is a simple, cheap and very informative way to diagnose many diseases. A general urine test can tell a lot about the state of the body as a whole and the functioning of individual organs in particular, which is why it is prescribed to almost all patients who seek medical help for the first time and is included in the list of annual medical examinations. Briefly about what protein and red blood cells are.
Protein is the main building material of the cells of a living organism, is found in all tissues and is involved in metabolic processes. Red blood cells are called red blood cells, the main function of which is to carry oxygen. Normally, a healthy person’s urine should not contain either the first or the second.
Classification
A small number of leukocytes may be found in the urine of a healthy person.
When microscopy of urine sediment, the norm is up to 3-5 leukocytes in the field of view. The norm of leukocytes according to the Nechiporenko method is less than 2000 per 1 ml, according to the Kakovsky-Addis method - up to 2,000,000 per day. Based on their origin, leukocyturia is divided into:
- Infectious
caused by urinary tract infection (pyelonephritis, cystitis). - Aseptic,
associated with inflammatory processes, MVP of non-infectious origin, mainly autoimmune (glomerulonephritis, rheumatological nephropathies, etc.).
According to the degree of severity, 2 large groups are distinguished: ordinary leukocyturia and pyuria, in which the number of cells is so large that the urine becomes cloudy, and under microscopy, leukocytes densely cover all fields of view. The presence of pyuria highly likely indicates an infectious lesion of the urinary tract.
Latent leukocyturia is distinguished separately, in which leukocytes are detected only when counting cells in special chambers (using the Nechiporenko and Kakovsky-Addis test), but are not detected during normal routine urine tests. Latent leukocyturia is often observed in young children and in patients with immunodeficiency conditions (decompensated diabetes mellitus, HIV infection).
When testing urine using test strips, incorrect results may be obtained:
- False negatives.
This is observed with high specific gravity of urine, severe glucosuria, and proteinuria. Also, an underestimation of the level of leukocytes occurs with a high concentration of ascorbic acid and taking antibacterial drugs (cephalexin, gentamicin, tetracycline). - False positives.
Overestimation of results is possible when using formaldehyde as a preservative or taking drugs that change the color of urine (nitrofurantoin, clavulanic acid).
Determination of leukocytes in urine
Kidney amyloidosis
Amyloidosis refers to a disorder of protein metabolism, in which amyloid, a protein-polysaccharide complex, is deposited in the tissues of the body. The disease most severely affects the kidneys, but also poses a danger to the heart and lungs, the nervous system and intestines are affected.
The cause of amyloidosis is most often long-term, severe infectious or chronic diseases. The main symptoms of renal amyloidosis: muscle pain, weakness, headaches, swelling, fatigue.
Red blood cells and protein in urine
- a serious reason for immediate contact with a specialist (nephrologist,
urologist
) for diagnosis and treatment.
This article does not constitute medical advice and should not serve as a substitute for consultation with a physician.
Causes of leukocyturia
UTI infections
The most common cause of leukocyturia is infectious diseases of the urinary tract. The penetration of microorganisms into the organs of the urinary tract causes an immune response - the migration of leukocytes into the tissues, the development of the inflammatory process. As a result, some leukocytes enter the urine. A distinctive feature of infectious leukocyturia is the presence of bacteriuria, an alkaline reaction of urine (pH above 7). Microscopy often reveals tripel phosphate crystals. Predominantly neutrophils are found.
- Cystitis.
With inflammation of the bladder, in addition to leukocytes, erythrocytes and an increase in the number of transitional epithelial cells are often found. - Pyelonephritis.
With inflammation of the renal pelvis, a large number of leukocytes, sometimes red blood cells, and protein are detected. The renal origin is indicated by the detection of renal epithelial cells, leukocytes, and waxy casts. - Urethritis.
With inflammation of the urethra, mainly only leukocytes are observed in the urine.
More severe forms of UTI (abscess, renal carbuncle) are also accompanied by massive leukocyturia. Depending on the severity of the inflammatory process, both moderate amounts and pyuria can be observed. Leukocyturia occurs acutely, against the background of vivid clinical symptoms (fever, dysuria), and regresses quite quickly under the influence of antibacterial therapy.
Infections of other organs
With other bacterial or viral infections, secondary kidney damage with concomitant leukocyturia is also possible. This occurs especially often in inflammatory diseases of organs anatomically close to the urinary tract - diseases of the female (colpitis, endometritis) and male reproductive system (balanoposthitis, prostatitis), pathologies in the abdominal cavity (appendicitis, pancreatitis).
Leukocyturia is observed somewhat less frequently in the following diseases:
- viral hepatitis (B, C);
- cytomegalovirus infection;
- flu;
- angina;
- pneumonia;
- otitis;
- HIV infection;
- sepsis.
With viral infections, the degree of leukocyturia is usually moderate; with bacterial infections, pyuria is possible. Elimination of the infectious focus leads to the disappearance of leukocytes from the urine.
Autoimmune diseases
An autoimmune inflammatory process in the kidneys is almost always accompanied by leukocyturia. Isolated leukocyturia is rarely observed; most often, red blood cells, a high protein concentration, and a decrease in specific gravity are also found in the urine. Microscopy reveals leukocyte and erythrocyte casts and kidney epithelial cells. Leukocytes are represented predominantly by lymphocytes.
An increase in the percentage of lymphocytes indicates an exacerbation of the disease. The level of leukocytes decreases under the influence of specific anti-inflammatory therapy when remission is achieved; slight leukocyturia can persist for a long time. Autoimmune diseases in which leukocyturia occurs:
- Glomerulonephritis.
- Lupus nephritis (lupus nephritis) with systemic lupus erythematosus.
- Scleroderma kidney in systemic scleroderma.
- Kidney damage in systemic vasculitis - polyarteritis nodosa, granulomatosis with polyangiitis.
Oncology
In case of malignant neoplasms of the urinary system (cancer of the kidney, bladder), leukocyturia develops gradually. It may appear long before any clinical signs occur. Lymphocytes predominate. In oncohematological pathologies (leukemia, lymphomas), immature forms of leukocytes are often detected - myelocytes, promyelocytes, blasts. Leukocyturia is usually moderate and decreases after courses of chemotherapy or surgical removal of the tumor.
Other reasons
- Interstitial nephritis.
It develops as a reaction to taking certain medications, especially NSAIDs (analgin, diclofenac), as well as helminthiasis (ascariasis). There is an increase in eosinophils - more than 5% and lymphocytes. - Kidney tuberculosis.
Tuberculous kidney damage is characterized by persistent moderate leukocyturia with an acidic reaction (pH 5-6) of the environment and microhematuria. - Renal transplant rejection reaction.
In acute rejection, an increase in eosinophils is detected in the urine; in chronic rejection, leukocytes are represented by lymphocytes. - Amyloidosis.
With renal amyloidosis, in some cases, leukocyturia is observed against the background of massive proteinuria.
Glomerulonephritis
Glomerulonephritis is an autoimmune disease, is a complication of certain infections (sore throat, scarlet fever, malaria, viral hepatitis, measles, etc.) or can be provoked by various allergens. Autoimmune means that the cells of the immune system mistakenly begin to attack healthy cells of their own body, in this case the glomerular cells that make up the kidney tissue.
Symptoms of the disease:
- temperature increase;
- high blood pressure;
- headache;
- swelling;
- urine the color of “meat slop.”
Glomerulonephritis is dangerous because it can result in chronic renal failure and require lifelong hemodialysis or an organ transplant. Treatment is carried out under the supervision of a nephrologist; in severe cases, hospitalization is required.
Diagnostics
If leukocyturia is detected, you must consult a general practitioner or nephrologist to find out the cause of its occurrence. The doctor asks the patient in detail about his complaints, the presence of diagnosed chronic diseases, and what medications the patient is taking. A physical examination is carried out - measuring body temperature, blood pressure, checking for the presence of peripheral edema, Pasternatsky's symptom.
It is worth noting that test strips for general urine analysis detect only neutrophils. In diseases accompanied predominantly by lymphocyturia (mainly autoimmune), in some patients the result will be negative. Lymphocytes and eosinophils can only be detected by microscopic examination of the native specimen or after staining it. If renal tuberculosis is suspected, a urine sediment specimen is stained using the Ziehl-Neelsen method.
To determine the source of leukocyturia, a 3-glass urine sample is performed. The predominance of leukocytes in the first portion indicates inflammation of the urethra, in the 3rd portion - cystitis or prostatitis. The uniform presence of leukocytes in all portions is characteristic of kidney damage. For differential diagnosis of the etiological factor, an additional examination is prescribed:
- Blood tests.
A general blood test reveals leukocytosis and an increase in ESR. A biochemical blood test reveals an increase in CRP, RF, and in case of glomerulonephritis - ASLO. In case of impaired renal excretory function, the concentration of creatinine and urea increases. - Microbiological research.
In case of UTI infections, it is necessary to culture a urine sample on nutrient media to determine sensitivity to antibiotics. - Immunological studies.
The presence of antibodies or antigens of infectious pathogens - viral hepatitis, influenza, HIV infection, etc. is examined. An analysis is also performed for autoantibodies - antibodies to double-stranded DNA, topoisomerase, antinuclear (ANA) and antibodies to neutrophil cytoplasm (ANCA). - Ultrasound.
Ultrasound of the kidneys with pyelonephritis reveals an expansion of the pyelocaliceal system, and with cystitis - thickening of the walls of the bladder. - Biopsy.
If cancer is suspected, a biopsy of the kidney or bladder is performed, followed by histological examination. To confirm amyloidosis, a tissue sample is taken from the lining of the mouth or rectum. - Consultation with other specialists.
If there are clinical signs of genital pathology, a consultation with a urologist or gynecologist is scheduled for examination, manual examination, and collection of material for further research.
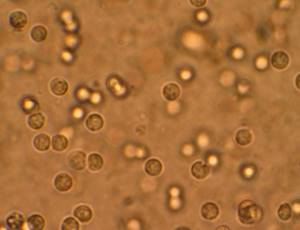
Leukocytes in urine under a microscope
In what cases is the presence of red blood cells and protein in the urine not considered a pathology?
An increased content of red blood cells and/or protein in the urine may indicate quite serious diseases. Most often we are talking about pathologies of the urinary system. Human kidneys are designed in such a way that these substances should not penetrate their walls, so it would be reasonable to assume that the problem lies either in the kidneys themselves or in what is located below.
But let's start with the valid values that do exist:
- men: red blood cells 0-1 units, protein up to 0.3 g/liter;
- women: red blood cells 0-3 units, protein up to 0.1 g/liter;
- children: red blood cells 2-4 units, protein up to 0.025 g/liter.
Protein may be present in the urine after physical exertion, stressful situations, consumption of protein foods, hypothermia, infectious diseases, allergic reactions, and prolonged stay in an upright position.
The content of red blood cells in the urine can be affected by the consumption of certain foods (spices, sour fruits, juices, alcohol) and medications (anticoagulants, sulfonamides); visiting a bathhouse or sauna and intense physical activity can also affect the results. But if a urine test showed the presence of high protein in combination with elevated red blood cells, then most likely we are talking about glameuronephritis or renal amyloidosis.
You can make an appointment with a urologist from our consultants by calling +7 (495) 125-49-50
Prices for urologist services Addresses of clinics Ultrasound of the prostate Protein in urine Blood tests for PSA Calling a urologist to your home
Correction
Conservative therapy
There are no independent methods for correcting leukocyturia. Treatment of the underlying disease is required. In case of interstitial nephritis caused by taking the drug, its discontinuation is necessary. Therapy can be carried out on an outpatient basis or in a hospital, it depends on the severity of the patient’s condition. The following medications are used:
- Antibiotics.
For cystitis, fosfomycin trometamol is prescribed; for pyelonephritis, antibiotics from the groups of penicillin (amoxicillin), cephalosporins (cefexime), and fluoroquinolones (ciprofloxacin, levofloxacin) are used. - Anti-inflammatory drugs.
Glucocorticosteroids (prednisolone) and cytostatic agents (cyclophosphamide, azathioprine) are effective in suppressing autoimmune inflammation. For lupus nephritis, synthetic antimalarials (hydroxychloroquine) are additionally used, and for scleroderma kidney - D-penicillamine. - Chemotherapy.
For oncological diseases, it is necessary to conduct courses of polychemotherapy drugs - sorafenib, sunitinib, bevacizumab. For amyloidosis, melphalan and bortezomib are prescribed.
Surgery
For kidney cancer, the main treatment method is surgical treatment - resection of the kidney or its complete removal (nephrectomy) open or laparoscopically. In case of amyloidosis, in case of development of end-stage renal failure, kidney transplantation is indicated. Patients with oncohematological pathologies undergo bone marrow transplantation.









